Sexually Transmitted Infections (Stis)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -

Nutrition in Andrology, Gynaecology and Obstetrics
Appendix No. 2 to the procedure of development and periodical review of syllabuses Nutrition in Andrology, Gynaecology and Obstetrics 1. Imprint Faculty name: English Division Syllabus (field of study, level and educational profile, form of studies, Medicine, 1st level studies, practical profile, full time e.g., Public Health, 1st level studies, practical profile, full time): Academic year: 2019/2020 Nutrition in Andrology, Gynaecology and Module/subject name: Obstetrics Subject code (from the Pensum system): Educational units: Department of Social Medicine and Public Health Head of the unit/s: Dr hab. n. med. Aneta Nitsch - Osuch Study year (the year during which the 1st-6th respective subject is taught): Study semester (the semester during which the respective subject is Winter and Summer semesters taught): Module/subject type (basic, corresponding to the field of study, Optional optional): Teachers (names and surnames and Anna Jagielska, MD degrees of all academic teachers of Aleksandra Kozłowska, BSc respective subjects): ERASMUS YES/NO (Is the subject available for students under the YES ERASMUS programme?): A person responsible for the syllabus (a person to which all comments to Anna Jagielska, MD the syllabus should be reported) Number of ECTS credits: 2 Page 1 of 4 Appendix No. 2 to the procedure of development and periodical review of syllabuses 2. Educational goals and aims The aim of the course is to provide students with: 1. The principles of nutrition during adolescence, adulthood and eldery. 2. The relationship between nutrition and fertility, fetal status and communicable diseases in the adults life. 3. Basics of dietary advices for men and women in the reproductive years. -
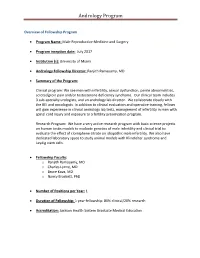
Andrology Program
Andrology Program Overview of Fellowship Program Program Name: Male Reproductive Medicine and Surgery Program inception date: July 2017 Institution (s): University of Miami Andrology Fellowship Director: Ranjith Ramasamy, MD Summary of the Program: Clinical program: We see men with infertility, sexual dysfunction, penile abnormalities, scrotal/groin pain and/or testosterone deficiency syndrome. Our clinical team includes 3 sub-specialty urologists, and an andrology lab director. We collaborate closely with the REI and oncologists. In addition to clinical evaluation and operative training, fellows will gain experience in clinical andrology lab tests, management of infertility in men with spinal cord injury and exposure to a fertility preservation program. Research Program: We have a very active research program with basic science projects on human testis models to evaluate genetics of male infertility and clinical trial to evaluate the effect of clomiphene citrate on idiopathic male infertility. We also have dedicated laboratory space to study animal models with Klinefelter syndrome and Leydig stem cells. Fellowship Faculty: o Ranjith Ramasamy, MD o Charles Lynne, MD o Bruce Kava, MD o Nancy Brackett, PhD Number of Positions per Year: 1 Duration of Fellowship: 1 year fellowship: 80% clinical/20% research Accreditation: Jackson Health System Graduate Medical Education Andrology Program Who to contact regarding the program: Millie Ferro Urology Administration M-814 Leonard M. Miller School of Medicine Contact e-mail: [email protected] Contact phone number: (305) 243-3246 Fax: (305) 243-6597 Contact Website: Overview of Fellowship Program / Description of Program: The Male Reproductive Medicine and Surgery Fellowship will enable the fellow to acquire an advanced body of knowledge and level of skill in the management of reproductive and sexual health diseases in order to assume a leadership role in teaching and research in the field. -

Andrology Lab Booklet
or Reprod er f uc nt ti e ve C M n a e c d i i r c e i Andrology Center and n m e A C e 3 9 n 9 tr 1 um t. E Es Reproductive Tissue Bank xcellentiae Who We Are What We Offer The Andrology Center and Reproductive Tissue Bank - The Andrology Center and Reproductive Tissue a section of the Glickman Urological & Kidney Institute Bank’s specialized laboratory offers a wide variety at Cleveland Clinic - provides specialized tests and of comprehensive tests and the latest technology services to evaluate male infertility. Our laboratory to meet patient needs. The Andrology Center offers offers referring physicians and patient’s quantifiable both research and clinical services. Our laboratory results using the latest state-of-the art technology. uses the latest World Health Organization (WHO, We are located in the Building X, which is part of the Fifth Edition, 2010) guidelines and reference ranges Downtown Main campus. in the evaluation of semen samples. Additionally, our laboratory’s Therapeutic Sperm Banking As part of the American Center for Reproductive program provides a complete fertility preservation Medicine, the Andrology Center and Reproductive service including a reliable system for the long-term Tissue Bank is staffed with highly qualified and preservation of human semen, epididymal aspirate experienced laboratory technologists who are well and testicular tissue. trained in fertility testing and certified by the American Society of Clinical Pathologists (ASCP). Our laboratory is certified by the Clinical Laboratory Improvement Table of Contents Amendments (CLIA) and the Department of Health and Human Services. -

Ejaculation Problems3 9
1 6 Fact Sheet 7 12 2 8 11 Ejaculation Problems3 9 4 10 5 What is ejaculation? 1 Bladder 2 Vas deferens Ejaculation is the release of semen from the penis 3 Urethra at orgasm (sexual climax). When a man is sexually 1 stimulated, the brain sends signals to the genital 6 4 Penis area through nerves in the spinal cord to make the 5 Scrotum 7 12 pelvic muscles contract. 2 8 6 Seminal vesicle 11 7 Rectum At orgasm, waves of muscle contractions transport 3 the sperm, with a small amount of fluid, from the 8 Prostate gland testes through to the vas deferens. The seminal 9 9 Epididymis vesicles and prostate contribute extra fluid to 4 10 Testicle protect the sperm. 10 11 Cowper’s gland 5 This mixture of sperm and fluid (semen) travels 12 Ejaculatory duct along the urethra to the tip of the penis where it is ejaculated (released). What are ejaculation problems? More details about premature ejaculation can be found in a separate1 Bladder Andrology Australia fact Men can experience different kinds of ejaculation sheet. 2 Vas deferens problems, including: 3 Urethra The other ejaculation4 Penis problems are less common • premature ejaculation than premature ejaculation5 Scrotum but can also cause distress for the man and his partner. • retrograde ejaculation 6 Seminal vesicle 7 Rectum • delayed ejaculation (or no ejaculation) What causes ejaculation problems? 8 Prostate gland • painful ejaculation. Ejaculation problems9 Epididymis can have a variety of 10 Testicle How common are ejaculation causes, both physical and psychological. Physical causes include11 Cowper’s some gland illnesses such problems? as diabetes, some 12typesEjaculatory of surgery duct or trauma, some types of inflammation or infection, certain Premature ejaculation is the most common male medicines, and chemical imbalances in the brain sexual problem and affects men of all ages. -

Male Anorgasmia: from “No” to “Go!”
Male Anorgasmia: From “No” to “Go!” Alexander W. Pastuszak, MD, PhD Assistant Professor Center for Reproductive Medicine Division of Male Reproductive Medicine and Surgery Scott Department of Urology Baylor College of Medicine Disclosures • Endo – speaker, consultant, advisor • Boston Scientific / AMS – consultant • Woven Health – founder, CMO Objectives • Understand what delayed ejaculation (DE) and anorgasmia are • Review the anatomy and physiology relevant to these conditions • Review what is known about the causes of DE and anorgasmia • Discuss management of DE and anorgasmia Definitions Delayed Ejaculation (DE) / Anorgasmia • The persistent or recurrent delay, difficulty, or absence of orgasm after sufficient sexual stimulation that causes personal distress Intravaginal Ejaculatory Latency Time (IELT) • Normal (median) à 5.4 minutes (0.55-44.1 minutes) • DE à mean IELT + 2 SD = 25 minutes • Incidence à 2-11% • Depends in part on definition used J Sex Med. 2005; 2: 492. Int J Impot Res. 2012; 24: 131. Ejaculation • Separate event from erection! • Thus, can occur in the ABSENCE of erection! Periurethral muscle Sensory input - glans (S2-4) contraction Emission Vas deferens contraction Sympathetic input (T12-L1) SV, prostate contraction Bladder neck contraction Expulsion Bulbocavernosus / Somatic input (S1-3) spongiosus contraction Projectile ejaculation J Sex Med. 2011; 8 (Suppl 4): 310. Neurochemistry Sexual Response Areas of the Brain • Pons • Nucleus paragigantocellularis Neurochemicals • Norepinephrine, serotonin: • Inhibit libido, -

Sexually Transmitted Infections and Semen Quality from Subfertile Men
Bai et al. Reproductive Biology and Endocrinology (2021) 19:92 https://doi.org/10.1186/s12958-021-00769-2 RESEARCH Open Access Sexually transmitted infections and semen quality from subfertile men with and without leukocytospermia Shun Bai1†, Yuan Li2†, Yangyang Wan1†, Tonghang Guo1, Qi Jin1, Ran Liu1, Wenjuan Tang1, Meiying Sang1, Yuanyuan Tao1, Baoguo Xie3, Yun Zhao1, Wei Li1, Xiangdong Xu1, Qiuling Yue4*, Xuechun Hu5* and Bo Xu1* Abstract Background: The role of sexually transmitted infections (STIs) in semen parameters and male infertility is still a controversial area. Previous studies have found bacterial infection in a minority of infertile leukocytospermic males. This study aims to investigate the prevalence of STIs in semen from subfertile men with leukocytospermia (LCS) and without leukocytospermia (non-LCS) and their associations with sperm quality. Methods: Semen samples were collected from 195 men who asked for a fertility evaluation. Infection with the above 6 pathogens was assessed in each sample. Sperm quality was compared in subfertile men with and without LCS. Results: The LCS group had significantly decreased semen volume, sperm concentration, progressive motility, total motility and normal morphology. The infection rates of Ureaplasma urealyticum (Uuu), Ureaplasma parvum (Uup), Mycoplasma hominis (MH), Mycoplasma genitalium (MG), Chlamydia trachomatis (CT), herpes simplex virus-2 (HSV-2) and Neisseria gonorrhoeae (NG) were 8.7 %, 21.0 %, 8.2 %, 2.1 %, 3.6 %, 1.0 and 0 %, respectively. The STI detection rates of patients with LCS were higher than those of the non-LCS group (52.3 % vs. 39.3 %), although there was no statistically significant difference between the two groups (P = 0.07). -

Guideline Development Group Meeting WHO Guidelines for the Prevention, Diagnosis, and Treatment of Infertility
Guideline Development Group Meeting WHO Guidelines for the Prevention, Diagnosis, and Treatment of Infertility Biographies of External Experts October 2018 Anna Krawczak Anna is a Board member, Fertility Europe, Association of European Patient Fertility Societies (Infertility Treatment and Adoption Support, Our Stork, Warszawa, Poland). She was also an advisor to MOH in Polish IVF Reimbursement Program Committee. She is a member of Fertility Europe, ESHRE, and American Anthropological Association. Her PhD thesis was on gamete and embryo donation in public discourse. Barbara Collura Barbara is the President and CEO of RESOLVE, The National Infertility Association in Washington, D.C., USA. The association act as an advocacy for infertile couples and through her leadership, the association has been involved with establishment of National Infertility Awareness Week (NIAW) and Personhood initiatives programs. Barbara Collura joined RESOLVE in September 2004 as the Director, Chapter & Constituent Services. In April 2007, Barbara was named Chief Staff Officer of RESOLVE. As President/CEO, she represents RESOLVE at a number of national conferences, committees and organizations including the National Committee on the Oversight of Assisted Reproductive Technologies (NCOART), the American Society for Reproductive Medicine (ASRM), the Advisory Council of the National Institute of Child Health and Human Development, and she served as a Board member of the National Health Council. Rita Sembuya Miss Sembuya is a founding member and Executive Director of Joyce Fertility Support Centre in Kampala, Uganda. The centre serves as an advocacy group for infertile couple in and around Uganda. She has worked with societies such as ESHRE, companies such as Merck and individual experts to highlight the burden of infertility amongst women in low-middle-income countries. -

Andrology Male Infertility Questionnaire
Andrology Male Infertility Questionnaire WE WOULD ASK THAT YOU PLEASE FILL IN THE FOLLOWING QUESTIONNAIRE AS COMPLETELY AND ACCURATELY AS POSSIBLE BEFORE YOU SEE THE MALE FERTILITY SPECIALIST. ALL PROVIDED INFORMATION WILL REMAIN CONFIDENTIAL. IT WILL BE RELEASED ONLY WITH YOUR WRITTEN PERMISSION AND WILL BE USED TO HELP US TREAT YOU. Dr. James M. Hotaling |Dr. Alex Pastuszak UTAH MEN’S HEALTH | AHEAD OF THE CURVE 5126 DAYBREAK PARKWAY, SOUTH JORDAN, UT 84009 FAX: 801-581-6127 UTAH MEN’S HEALTH | Ahead of the Curve Andrology Male Infertility Questionnaire * Indicates a required field. Current Partner History *Pregnancy with current partner? Yes No If yes, did pregnancy result in a child? Yes No If yes, children’s ages. ______________________________________________________________________________ *How many years have you had unprotected sex not resulting in pregnancy? ______________________________________________________________________________ *How often do you have sex per month? ______________________________________________________________________________ Ejaculation Painful? Yes No *Semen Color White Yellow Brown Red *More semen when younger? Yes No *Erection problems? No Sometimes Mostly Always *Urination painful after sex? Yes No *Urine cloudy after sex? Yes No *Contraception Never used Birth control pill Intrauterine device Condom Diaphragm Other Revised 17 March 2017 UTAH MEN’S HEALTH | Ahead of the Curve Andrology Male Infertility Questionnaire * Indicates a required field. Date when contraception last used. _____________________________________________________ -

Examination and Processing of Human Semen
WHO laboratory manual for the Examination and processing of human semen FIFTH EDITION WHO laboratory manual for the Examination and processing of human semen FIFTH EDITION WHO Library Cataloguing-in-Publication Data WHO laboratory manual for the examination and processing of human semen - 5th ed. Previous editions had different title : WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 1.Semen - chemistry. 2.Semen - laboratory manuals. 3.Spermatozoa - laboratory manuals. 4.Sperm count. 5.Sperm-ovum interactions - laboratory manuals. 6.Laboratory techniques and procedures - standards. 7.Quality control. I.World Health Organization. ISBN 978 92 4 154778 9 (NLM classifi cation: QY 190) © World Health Organization 2010 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications— whether for sale or for noncommercial distribution—should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expres- sion of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specifi c companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Essentials in Male Sexual History Taking
Stefan Arver Centre for andrology and Sexual Medicine Karolinska University Hospital Stockholm, Sweden ESSENTIALS IN MALE SEXUAL HISTORY TAKING Overview Congenital disorders Malformations –Disorder of Sexual Development Acquired conditions in childhood Trauma, severe medical disorders Childhood trauma Pubertal development Sexual history Sexual experiences Relationship history Medical history Congenital conditions DSD –disorder of sexual development Early repeated traumatisation of genital region Hypospadia common disorder Micropen is Conditions affecting fertility Pubertal disorders – praecox, delayed puberty Problems related to puberty Pubertas paecox –sexual maturation prior to social development Pubertas tarda –2% of men puberty after age of 16 Loss of social context and development –psychological proble when peers start to develop and mature as sexual individulas Lack of muscle and hight development –change of role and p capacity –outside sports activities Adulthood and late adolescens Define the problem: Erectile dysfunction – inability to achieve and maintain erection sufficient for sexual activity Premature ejaculation – Intravaginal latency < 1 min Lack of control Psychosocial distress Ejaculatio tarda – inability to achieve orgasm (ejaculation) Retrograde ejaculation ”Sexological” aspects Patient’s own description Sexual behavior & patterns previous positive and negative sexual experiences Sexual satisfaction; does the problem cause distress? Start and development of problem(s) Always? Acquired? Acute or gradual Global or situational Experience from treatment and ”own measures” ”Sexological” aspects Partner ? reactions, partners problems Disease(s), impairment(s), medication(s): ‐ limitations/resourses ‐ coping ‐ cultural & social aspects Insights, expectations, motivation Partner aspects Evaluate the partners percieved problem Who is really the ”patient”? Is there a consensus of the problem? Take home message An adequate case history must include: Impairment/Psych.