Sexual Abstinence and Sperm Quality
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reference Sheet 1
MALE SEXUAL SYSTEM 8 7 8 OJ 7 .£l"00\.....• ;:; ::>0\~ <Il '"~IQ)I"->. ~cru::>s ~ 6 5 bladder penis prostate gland 4 scrotum seminal vesicle testicle urethra vas deferens FEMALE SEXUAL SYSTEM 2 1 8 " \ 5 ... - ... j 4 labia \ ""\ bladderFallopian"k. "'"f"";".'''¥'&.tube\'WIT / I cervixt r r' \ \ clitorisurethrauterus 7 \ ~~ ;~f4f~ ~:iJ 3 ovaryvagina / ~ 2 / \ \\"- 9 6 adapted from F.L.A.S.H. Reproductive System Reference Sheet 3: GLOSSARY Anus – The opening in the buttocks from which bowel movements come when a person goes to the bathroom. It is part of the digestive system; it gets rid of body wastes. Buttocks – The medical word for a person’s “bottom” or “rear end.” Cervix – The opening of the uterus into the vagina. Circumcision – An operation to remove the foreskin from the penis. Cowper’s Glands – Glands on either side of the urethra that make a discharge which lines the urethra when a man gets an erection, making it less acid-like to protect the sperm. Clitoris – The part of the female genitals that’s full of nerves and becomes erect. It has a glans and a shaft like the penis, but only its glans is on the out side of the body, and it’s much smaller. Discharge – Liquid. Urine and semen are kinds of discharge, but the word is usually used to describe either the normal wetness of the vagina or the abnormal wetness that may come from an infection in the penis or vagina. Duct – Tube, the fallopian tubes may be called oviducts, because they are the path for an ovum. -

Differential Sperm Motility Mediates the Sex Ratio Drive Shaping Mouse
bioRxiv preprint doi: https://doi.org/10.1101/649707; this version posted May 24, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Differential sperm motility mediates the sex ratio drive shaping mouse sex chromosome evolution Rathje CC1, Johnson EEP2, Drage D3, Patinioti C1, Silvestri G1, Affara NA2, Ialy-Radio C4, Cocquet J4, Skinner BM2,5, Ellis PJI1,5* 1 School of Biosciences, University of Kent, Canterbury, CT2 7NJ, United Kingdom 2 Department of Pathology, University of Cambridge, Tennis Court Road, Cambridge, CB2 1QP, United Kingdom 3 University Biomedical Services, University of Cambridge, Cambridge, United Kingdom 4 Department of Development, Reproduction and Cancer, INSERM, U1016, Institut Cochin, Paris, France; CNRS, UMR8104, Paris, France; Université Paris Descartes, Sorbonne Paris Cité, Faculté de Médecine, Paris, France. 5 These authors contributed equally * Corresponding author: Peter Ellis Email: P.J.I.Ellis @kent.ac.uk Tel: +44(0)1227 82 3526 KEYWORDS: Sex ratio, sex chromosomes, transmission ratio, evolution, sperm, fertilisation 1 bioRxiv preprint doi: https://doi.org/10.1101/649707; this version posted May 24, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Summary The search for morphological or physiological differences between X- and Y-bearing mammalian sperm has provoked controversy for decades. -

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

THE PHYSIOLOGY and ECOPHYSIOLOGY of EJACULATION Tropical and Subtropical Agroecosystems, Vol
Tropical and Subtropical Agroecosystems E-ISSN: 1870-0462 [email protected] Universidad Autónoma de Yucatán México Lucio, R. A.; Cruz, Y.; Pichardo, A. I.; Fuentes-Morales, M. R.; Fuentes-Farias, A.L.; Molina-Cerón, M. L.; Gutiérrez-Ospina, G. THE PHYSIOLOGY AND ECOPHYSIOLOGY OF EJACULATION Tropical and Subtropical Agroecosystems, vol. 15, núm. 1, 2012, pp. S113-S127 Universidad Autónoma de Yucatán Mérida, Yucatán, México Available in: http://www.redalyc.org/articulo.oa?id=93924484010 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Tropical and Subtropical Agroecosystems, 15 (2012) SUP 1: S113 – S127 REVIEW [REVISIÓN] THE PHYSIOLOGY AND ECOPHYSIOLOGY OF EJACULATION [FISIOLOGÍA Y ECOFISIOLOGÍA DE LA EYACULACIÓN] R. A. Lucio1*, Y. Cruz1, A. I. Pichardo2, M. R. Fuentes-Morales1, A.L. Fuentes-Farias3, M. L. Molina-Cerón2 and G. Gutiérrez-Ospina2 1Centro Tlaxcala de Biología de la Conducta, Universidad Autónoma de Tlaxcala, Tlaxcala-Puebla km 1.5 s/n, Loma Xicotencatl, 90062, Tlaxcala, Tlax., México. 2Depto. Biología Celular y Fisiología, Instituto de Investigaciones Biomédicas, Universidad Nacional Autónoma de México, Ciudad Universitaria, 04510, México, D.F., México. 3Laboratorio de Ecofisiologia Animal, Departamento de Fisiologia, Instituto de Investigaciones sobre los Recursos Naturales, Universidad Michoacana de San Nicolás de Hidalgo, Av. San Juanito Itzicuaro s/n, Colonia Nueva Esperanza 58337, Morelia, Mich., México * Corresponding author ABSTRACT RESUMEN Different studies dealing with ejaculation view this Diferentes estudios enfocados en la eyaculación, process as a part of the male copulatory behavior. -

Revised Glossary for AQA GCSE Biology Student Book
Biology Glossary amino acids small molecules from which proteins are A built abiotic factor physical or non-living conditions amylase a digestive enzyme (carbohydrase) that that affect the distribution of a population in an breaks down starch ecosystem, such as light, temperature, soil pH anaerobic respiration respiration without using absorption the process by which soluble products oxygen of digestion move into the blood from the small intestine antibacterial chemicals chemicals produced by plants as a defence mechanism; the amount abstinence method of contraception whereby the produced will increase if the plant is under attack couple refrains from intercourse, particularly when an egg might be in the oviduct antibiotic e.g. penicillin; medicines that work inside the body to kill bacterial pathogens accommodation ability of the eyes to change focus antibody protein normally present in the body acid rain rain water which is made more acidic by or produced in response to an antigen, which it pollutant gases neutralises, thus producing an immune response active site the place on an enzyme where the antimicrobial resistance (AMR) an increasing substrate molecule binds problem in the twenty-first century whereby active transport in active transport, cells use energy bacteria have evolved to develop resistance against to transport substances through cell membranes antibiotics due to their overuse against a concentration gradient antiretroviral drugs drugs used to treat HIV adaptation features that organisms have to help infections; they -

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -

Nutrition in Andrology, Gynaecology and Obstetrics
Appendix No. 2 to the procedure of development and periodical review of syllabuses Nutrition in Andrology, Gynaecology and Obstetrics 1. Imprint Faculty name: English Division Syllabus (field of study, level and educational profile, form of studies, Medicine, 1st level studies, practical profile, full time e.g., Public Health, 1st level studies, practical profile, full time): Academic year: 2019/2020 Nutrition in Andrology, Gynaecology and Module/subject name: Obstetrics Subject code (from the Pensum system): Educational units: Department of Social Medicine and Public Health Head of the unit/s: Dr hab. n. med. Aneta Nitsch - Osuch Study year (the year during which the 1st-6th respective subject is taught): Study semester (the semester during which the respective subject is Winter and Summer semesters taught): Module/subject type (basic, corresponding to the field of study, Optional optional): Teachers (names and surnames and Anna Jagielska, MD degrees of all academic teachers of Aleksandra Kozłowska, BSc respective subjects): ERASMUS YES/NO (Is the subject available for students under the YES ERASMUS programme?): A person responsible for the syllabus (a person to which all comments to Anna Jagielska, MD the syllabus should be reported) Number of ECTS credits: 2 Page 1 of 4 Appendix No. 2 to the procedure of development and periodical review of syllabuses 2. Educational goals and aims The aim of the course is to provide students with: 1. The principles of nutrition during adolescence, adulthood and eldery. 2. The relationship between nutrition and fertility, fetal status and communicable diseases in the adults life. 3. Basics of dietary advices for men and women in the reproductive years. -

Semen Arousal: Its Prevalence, Relationship to HIV Risk Practices
C S & lini ID ca A l f R o e l s Klein, J AIDS Clin Res 2016, 7:2 a e Journal of n a r r DOI: 10.4172/2155-6113.1000546 c u h o J ISSN: 2155-6113 AIDS & Clinical Research Research Article Open Access Semen Arousal: Its Prevalence, Relationship to HIV Risk Practices, and Predictors among Men Using the Internet to Find Male Partners for Unprotected Sex Hugh Klein* Kensington Research Institute, USA Abstract Purpose: This paper examines the extent to which men who use the Internet to find other men for unprotected sex are aroused by semen. It also looks at the relationship between semen arousal and involvement in HIV risk practices, and the factors associated with higher levels of semen arousal. Methods: 332 men who used any of 16 websites targeting unprotected sex completed 90-minute telephone interviews. Both quantitative and qualitative data were collected. A random sampling strategy was used. Semen arousal was assessed by four questions asking men how much they were turned on by the way that semen smelled, tasted, looked, and felt. Results: 65.1% of the men found at least one sensory aspect of semen to be “fairly” or “very” arousing, compared to 10.2% being “not very” or “not at all” aroused by all four sensory aspects of semen. Multivariate analysis revealed that semen arousal was related to greater involvement in HIV risk practices, even when the impact of other salient factors such as demographic characteristics, HIV serostatus, and psychological functioning was taken into account. Five factors were found to underlie greater levels of semen arousal: not being African American, self-identification as a sexual “bottom,” being better educated, being HIV-positive, and being more depressed. -

Commentary Unprotected: Condoms, Bareback Porn, and the First Amendment
Commentary Unprotected: Condoms, Bareback Porn, and the First Amendment Bailey J. Langnert ABSTRACT In November 2012, Los Angeles County voters passed Measure B, or the Safer Sex in the Adult Film Industry Act. Measure B mandated condom use by all porn performers in adult films produced within county borders and created a complex regulatory process for adult film producers that included permitting, mandatory public health trainings, and warrantless administrative searches. Shortly after its passage, Vivid Entertainment filed a lawsuit to enjoin the enforcement of Measure B, arguing that the Measure violated their First Amendment right to portray condomless sex in porn. In December 2014, the Ninth Circuit upheld the district court's decision upholding the constitutionality of Measure B. Notably, the mainstream discourse surrounding the Measure B campaign, as well as the legal arguments put forth in the lawsuit, focused exclusively on straight pornography while purporting to represent all porn. As a result, an entire genre of condomless pornography went unrepresented in the discussion: bareback porn, which portrays intentional unprotected anal sex between men. Excluding bareback porn from the lawsuit represented a missed opportunityfor Vivid in its challenge of Measure B. There are several political messages underlying bareback porn unique to that genre that might have resulted in the t The author received a law degree from the University of California, Berkeley, School of Law (Boalt Hall) in 2015. As a law student, the author worked as a Teaching Assistant in the First Year Legal Writing Program and served as a Senior Board Member of the Boalt Hall Women's Association. -
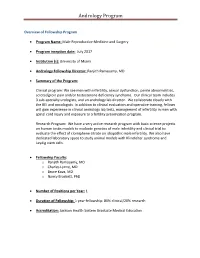
Andrology Program
Andrology Program Overview of Fellowship Program Program Name: Male Reproductive Medicine and Surgery Program inception date: July 2017 Institution (s): University of Miami Andrology Fellowship Director: Ranjith Ramasamy, MD Summary of the Program: Clinical program: We see men with infertility, sexual dysfunction, penile abnormalities, scrotal/groin pain and/or testosterone deficiency syndrome. Our clinical team includes 3 sub-specialty urologists, and an andrology lab director. We collaborate closely with the REI and oncologists. In addition to clinical evaluation and operative training, fellows will gain experience in clinical andrology lab tests, management of infertility in men with spinal cord injury and exposure to a fertility preservation program. Research Program: We have a very active research program with basic science projects on human testis models to evaluate genetics of male infertility and clinical trial to evaluate the effect of clomiphene citrate on idiopathic male infertility. We also have dedicated laboratory space to study animal models with Klinefelter syndrome and Leydig stem cells. Fellowship Faculty: o Ranjith Ramasamy, MD o Charles Lynne, MD o Bruce Kava, MD o Nancy Brackett, PhD Number of Positions per Year: 1 Duration of Fellowship: 1 year fellowship: 80% clinical/20% research Accreditation: Jackson Health System Graduate Medical Education Andrology Program Who to contact regarding the program: Millie Ferro Urology Administration M-814 Leonard M. Miller School of Medicine Contact e-mail: [email protected] Contact phone number: (305) 243-3246 Fax: (305) 243-6597 Contact Website: Overview of Fellowship Program / Description of Program: The Male Reproductive Medicine and Surgery Fellowship will enable the fellow to acquire an advanced body of knowledge and level of skill in the management of reproductive and sexual health diseases in order to assume a leadership role in teaching and research in the field. -

Sperm Motility, Oxidative Status, and Mitochondrial Activity: Exploring Correlation in Different Species
antioxidants Article Sperm Motility, Oxidative Status, and Mitochondrial Activity: Exploring Correlation in Different Species Alessandra Gallo 1,* , Maria Consiglia Esposito 1 , Elisabetta Tosti 1 and Raffaele Boni 1,2,* 1 Department of Biology and Evolution of Marine Organisms, Stazione Zoologica Anton Dohrn, Villa Comunale, 80121 Naples, Italy; [email protected] (M.C.E.); [email protected] (E.T.) 2 Department of Sciences, University of Basilicata, 85100 Potenza, Italy * Correspondence: [email protected] (A.G.); [email protected] (R.B.); Tel.: +39-081-5833233 (A.G.); +39-0971-205017 (R.B.) Abstract: Sperm quality assessment is the first step for evaluating male fertility and includes the estimation of sperm concentration, motility, and morphology. Nevertheless, other parameters can be assessed providing additional information on the male reproductive potential. This study aimed to evaluate and correlate the oxidative status, mitochondrial functionality, and motility in sperma- tozoa of two marine invertebrate (Ciona robusta and Mytilus galloprovincialis) and one mammalian (Bos taurus) species. By combining fluorescent staining and spectrofluorometer, sperm oxidative status was evaluated through intracellular reactive oxygen species (ROS) and plasma membrane lipid peroxidation (LPO) analysis. Mitochondrial functionality was assessed through the mitochondrial membrane potential (MMP). In the three examined species, a negative correlation emerged between sperm motility vs ROS levels and LPO. Sperm motility positively correlated with MMP in bovine, whereas these parameters were not related in ascidian or even negatively related in mussel sper- matozoa. MMP was negatively related to ROS and LPO levels in ascidians, only to LPO in bovine, Citation: Gallo, A.; Esposito, M.C.; and positively related in mussel spermatozoa. -

Gay Men and Barebacking: Radical Or Realistic?
Eric J. Roberson ENG 3305 – Essay Writing Dr. JoAnn Pavletich – UHD Fall 2009 Semester 2 Dec. 2009 Gay Men and Barebacking: Radical or Realistic? By Eric J. Roberson Prepared for Dr. JoAnn Pavletich ENG 3305 Advanced Essay Writing Fall 2009 Semester Gay Men and Barebacking: Radical or Realistic? Page 1 of 17 By Eric J. Roberson Gay Men and “Barebacking”: Radical or Realistic? By Eric J. Roberson Sex is not a competitive sport, and if you are gay and think it is then you should listen up! “HIV is a serious long-term condition, and young gay men remain the group of young people most at risk” (“UK Same-Sex Relationships 1). Some gay men willfully and deliberately discard condoms in preference for unprotected sex. Regardless of your age, this essay will not convince you on what to do with your “hard on,” but it may help you decide to get tested and to put on a condom before your next casual sexual encounter. Consider these three simple solutions: communication before sex, compassion for others, and condoms for casual encounters. If you happen to be straight and are reading this essay, do not put it down. Straight people who have gay friends may learn about some of the challenges gay men face in leading fulfilling relationships. You may also gain ideas on how to be more supportive. Regardless of your sexual orientation, the goal is to expose how the internet has shaped the practice of barebacking and other mitigating factors that compel gay men to consciously and explicitly eschew condoms during anal intercourse – colloquially known as “barebacking” (Gastaldo, et.