The Diverse Contribution of Keratinocytes to Immune Responses in Skin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cytokine Nomenclature
RayBiotech, Inc. The protein array pioneer company Cytokine Nomenclature Cytokine Name Official Full Name Genbank Related Names Symbol 4-1BB TNFRSF Tumor necrosis factor NP_001552 CD137, ILA, 4-1BB ligand receptor 9 receptor superfamily .2. member 9 6Ckine CCL21 6-Cysteine Chemokine NM_002989 Small-inducible cytokine A21, Beta chemokine exodus-2, Secondary lymphoid-tissue chemokine, SLC, SCYA21 ACE ACE Angiotensin-converting NP_000780 CD143, DCP, DCP1 enzyme .1. NP_690043 .1. ACE-2 ACE2 Angiotensin-converting NP_068576 ACE-related carboxypeptidase, enzyme 2 .1 Angiotensin-converting enzyme homolog ACTH ACTH Adrenocorticotropic NP_000930 POMC, Pro-opiomelanocortin, hormone .1. Corticotropin-lipotropin, NPP, NP_001030 Melanotropin gamma, Gamma- 333.1 MSH, Potential peptide, Corticotropin, Melanotropin alpha, Alpha-MSH, Corticotropin-like intermediary peptide, CLIP, Lipotropin beta, Beta-LPH, Lipotropin gamma, Gamma-LPH, Melanotropin beta, Beta-MSH, Beta-endorphin, Met-enkephalin ACTHR ACTHR Adrenocorticotropic NP_000520 Melanocortin receptor 2, MC2-R hormone receptor .1 Activin A INHBA Activin A NM_002192 Activin beta-A chain, Erythroid differentiation protein, EDF, INHBA Activin B INHBB Activin B NM_002193 Inhibin beta B chain, Activin beta-B chain Activin C INHBC Activin C NM005538 Inhibin, beta C Activin RIA ACVR1 Activin receptor type-1 NM_001105 Activin receptor type I, ACTR-I, Serine/threonine-protein kinase receptor R1, SKR1, Activin receptor-like kinase 2, ALK-2, TGF-B superfamily receptor type I, TSR-I, ACVRLK2 Activin RIB ACVR1B -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
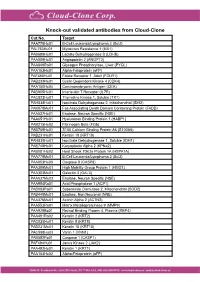
Knock-Out Validated Antibodies from Cloud-Clone Cat.No
Knock-out validated antibodies from Cloud-Clone Cat.No. Target PAA778Hu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAL763Hu01 Myxovirus Resistance 1 (MX1) PAB698Hu01 Lactate Dehydrogenase B (LDHB) PAA009Hu01 Angiopoietin 2 (ANGPT2) PAA849Ra01 Glycogen Phosphorylase, Liver (PYGL) PAA153Hu01 Alpha-Fetoprotein (aFP) PAF460Hu01 Folate Receptor 1, Adult (FOLR1) PAB233Hu01 Cyclin Dependent Kinase 4 (CDK4) PAA150Hu04 Carcinoembryonic Antigen (CEA) PAB905Hu01 Interleukin 7 Receptor (IL7R) PAC823Hu01 Thymidine Kinase 1, Soluble (TK1) PAH838Hu01 Isocitrate Dehydrogenase 2, mitochondrial (IDH2) PAK078Mu01 Fas Associating Death Domain Containing Protein (FADD) PAA537Hu01 Enolase, Neuron Specific (NSE) PAA651Hu01 Hyaluronan Binding Protein 1 (HABP1) PAB215Hu02 Fibrinogen Beta (FGb) PAB769Hu01 S100 Calcium Binding Protein A6 (S100A6) PAB231Hu01 Keratin 18 (KRT18) PAH839Hu01 Isocitrate Dehydrogenase 1, Soluble (IDH1) PAE748Hu01 Karyopherin Alpha 2 (KPNa2) PAB081Hu02 Heat Shock 70kDa Protein 1A (HSPA1A) PAA778Mu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAA853Hu03 Caspase 8 (CASP8) PAA399Mu01 High Mobility Group Protein 1 (HMG1) PAA303Mu01 Galectin 3 (GAL3) PAA537Mu02 Enolase, Neuron Specific (NSE) PAA994Ra01 Acid Phosphatase 1 (ACP1) PAB083Ra01 Superoxide Dismutase 2, Mitochondrial (SOD2) PAB449Mu01 Enolase, Non Neuronal (NNE) PAA376Mu01 Actinin Alpha 2 (ACTN2) PAA553Ra01 Matrix Metalloproteinase 9 (MMP9) PAA929Bo01 Retinol Binding Protein 4, Plasma (RBP4) PAA491Ra02 Keratin 2 (KRT2) PAC025Hu01 Keratin 8 (KRT8) PAB231Mu01 Keratin 18 (KRT18) PAC598Hu03 Vanin 1 (VNN1) -

Evolutionary Divergence and Functions of the Human Interleukin (IL) Gene Family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W
UPDATE ON GENE COMPLETIONS AND ANNOTATIONS Evolutionary divergence and functions of the human interleukin (IL) gene family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W. Nebert3* and Vasilis Vasiliou1 1Molecular Toxicology and Environmental Health Sciences Program, Department of Pharmaceutical Sciences, University of Colorado Denver, Aurora, CO 80045, USA 2Department of Clinical Pharmacy, University of Colorado Denver, Aurora, CO 80045, USA 3Department of Environmental Health and Center for Environmental Genetics (CEG), University of Cincinnati Medical Center, Cincinnati, OH 45267–0056, USA *Correspondence to: Tel: þ1 513 821 4664; Fax: þ1 513 558 0925; E-mail: [email protected]; [email protected] Date received (in revised form): 22nd September 2010 Abstract Cytokines play a very important role in nearly all aspects of inflammation and immunity. The term ‘interleukin’ (IL) has been used to describe a group of cytokines with complex immunomodulatory functions — including cell proliferation, maturation, migration and adhesion. These cytokines also play an important role in immune cell differentiation and activation. Determining the exact function of a particular cytokine is complicated by the influence of the producing cell type, the responding cell type and the phase of the immune response. ILs can also have pro- and anti-inflammatory effects, further complicating their characterisation. These molecules are under constant pressure to evolve due to continual competition between the host’s immune system and infecting organisms; as such, ILs have undergone significant evolution. This has resulted in little amino acid conservation between orthologous proteins, which further complicates the gene family organisation. Within the literature there are a number of overlapping nomenclature and classification systems derived from biological function, receptor-binding properties and originating cell type. -

Np63 Regulates IL-33 and IL-31 Signaling in Atopic Dermatitis
Cell Death and Differentiation (2016) 23, 1073–1085 OPEN & 2016 Macmillan Publishers Limited All rights reserved 1350-9047/16 www.nature.com/cdd ΔNp63 regulates IL-33 and IL-31 signaling in atopic dermatitis JM Rizzo1,2, A Oyelakin3, S Min3, K Smalley1, J Bard1, W Luo1,7, J Nyquist4, E Guttman-Yassky5, T Yoshida6, A De Benedetto6, LA Beck6, S Sinha*,1 and R-A Romano*,3 Atopic dermatitis (AD) is the most common inflammatory skin disease with no well-delineated cause or effective cure. Here we show that the p53 family member p63, specifically the ΔNp63, isoform has a key role in driving keratinocyte activation in AD. We find that overexpression of ΔNp63 in transgenic mouse epidermis results in a severe skin phenotype that shares many of the key clinical, histological and molecular features associated with human AD. This includes pruritus, epidermal hyperplasia, aberrant keratinocyte differentiation, enhanced expression of selected cytokines and chemokines and the infiltration of large numbers of inflammatory cells including type 2 T-helper cells – features that are highly representative of AD dermatopathology. We further demonstrate several of these mediators to be direct transcriptional targets of ΔNp63 in keratinocytes. Of particular significance are two p63 target genes, IL-31 and IL-33, both of which are key players in the signaling pathways implicated in AD. Importantly, we find these observations to be in good agreement with elevated levels of ΔNp63 in skin lesions of human patients with AD. Our studies reveal an important role for ΔNp63 in the pathogenesis of AD and offer new insights into its etiology and possible therapeutic targets. -

7/23/2021 Human IL-31 Protein, His Tag (MALS Verified) Catalog # IL1-H5247
Human IL-31 Protein, His Tag (MALS verified) Catalog # IL1-H5247 Synonym Formulation IL-31,IL31,Interleukin-31 Lyophilized from 0.22 μm filtered solution in PBS, pH7.4. Normally trehalose is Source added as protectant before lyophilization. Human IL-31, His Tag (IL1-H5247) is expressed from human 293 cells Contact us for customized product form or formulation. (HEK293). It contains AA Ser 24 - Thr 164 (Accession # Q6EBC2-1). Reconstitution Predicted N-terminus: His Molecular Characterization Please see Certificate of Analysis for specific instructions. For best performance, we strongly recommend you to follow the reconstitution protocol provided in the CoA. Storage This protein carries a polyhistidine tag at the N-terminus. For long term storage, the product should be stored at lyophilized state at -20°C The protein has a calculated MW of 17.7 kDa. The protein migrates as 23-33 or lower. kDa under reducing (R) condition (SDS-PAGE) due to glycosylation. Please avoid repeated freeze-thaw cycles. Endotoxin This product is stable after storage at: Less than 1.0 EU per μg by the LAL method. -20°C to -70°C for 12 months in lyophilized state; -70°C for 3 months under sterile conditions after reconstitution. Purity >90% as determined by SDS-PAGE. >90% as determined by SEC-MALS. SDS-PAGE SEC-MALS Human IL-31, His Tag on SDS-PAGE under reducing (R) condition. The gel The purity of Human IL-31, His Tag (Cat. No. IL1-H5247) was more than 90% was stained overnight with Coomassie Blue. The purity of the protein is greater and the molecular weight of this protein is around 15-25 kDa verified by SEC- than 90%. -

Human Cytokine Response Profiles
Comprehensive Understanding of the Human Cytokine Response Profiles A. Background The current project aims to collect datasets profiling gene expression patterns of human cytokine treatment response from the NCBI GEO and EBI ArrayExpress databases. The Framework for Data Curation already hosted a list of candidate datasets. You will read the study design and sample annotations to select the relevant datasets and label the sample conditions to enable automatic analysis. If you want to build a new data collection project for your topic of interest instead of working on our existing cytokine project, please read section D. We will explain the cytokine project’s configurations to give you an example on creating your curation task. A.1. Cytokine Cytokines are a broad category of small proteins mediating cell signaling. Many cell types can release cytokines and receive cytokines from other producers through receptors on the cell surface. Despite some overlap in the literature terminology, we exclude chemokines, hormones, or growth factors, which are also essential cell signaling molecules. Meanwhile, we count two cytokines in the same family as the same if they share the same receptors. In this project, we will focus on the following families and use the member symbols as standard names (Table 1). Family Members (use these symbols as standard cytokine names) Colony-stimulating factor GCSF, GMCSF, MCSF Interferon IFNA, IFNB, IFNG Interleukin IL1, IL1RA, IL2, IL3, IL4, IL5, IL6, IL7, IL9, IL10, IL11, IL12, IL13, IL15, IL16, IL17, IL18, IL19, IL20, IL21, IL22, IL23, IL24, IL25, IL26, IL27, IL28, IL29, IL30, IL31, IL32, IL33, IL34, IL35, IL36, IL36RA, IL37, TSLP, LIF, OSM Tumor necrosis factor TNFA, LTA, LTB, CD40L, FASL, CD27L, CD30L, 41BBL, TRAIL, OPGL, APRIL, LIGHT, TWEAK, BAFF Unassigned TGFB, MIF Table 1. -

IL-31 Expression by Inflammatory Cells Is Preferentially Elevated In
Acta Derm Venereol 2012; 92: 24–28 INVESTIGATIVE REPORT IL-31 Expression by Inflammatory Cells is Preferentially Elevated in Atopic Dermatitis Stephan NOBBE1, Piotr DZIUNYCZ1, Beda MÜHLEISEN1, Janine BILSBOROUGH2, Stacey R. DILLON2, Lars E. FRENCH1 and Günther F. L. HOFBAUER1 1Department of Dermatology, University Hospital Zürich, Switzerland, and 2Department of Immunology, ZymoGenetics, Inc., WA, Seattle, USA Interleukin-31 (IL-31) is a recently discovered cytokine STAT and PI-3 kinase signaling pathways (1, 5, 6). The re- expressed in many human tissues, and predominantly by ceptor components IL-31RA and OSMR are co-expressed activated CD4+ T cells. IL-31 signals through a hetero- on keratinocytes and activated monocytes (1). Besides the dimeric receptor consisting of IL-31 receptor alpha (IL- skin, other tissues, such as testis, thymus, trachea, intestinal 31RA) and oncostatin M receptor beta (OSMR). Earlier epithelial cells and dorsal root ganglia, show mRNA co- studies have shown involvement of IL-31 and its receptor expression for the receptor components (1, 3, 7, 8). components IL-31RA and OSMR in atopic dermatitis, Atopic dermatitis (AD) is a chronic inflammatory skin pruritus and Th2-weighted inflammation at the mRNA disease that is associated with intense pruritus. The me- level. The aim of this study was to investigate IL-31 pro- chanisms underlying dermatitis and pruritus are complex tein expression in skin of such conditions. Immunohisto- and not fully understood (9, 10), but there is emerging chemical staining for IL-31, IL-31RA and OSMR was evidence that IL-31 may play a role. Transgenic mice performed in formalin-fixed paraffin-embedded biopsy that overexpress IL-31 develop severe pruritus and skin specimens. -

Regulation of Skin Barrier Function Via Competition Between AHR Axis
Journal of Clinical Medicine Review Regulation of Skin Barrier Function via Competition between AHR Axis versus IL-13/IL-4-JAK-STAT6/STAT3 Axis: Pathogenic and Therapeutic Implications in Atopic Dermatitis Masutaka Furue 1,2 1 Department of Dermatology, Graduate School of Medical Sciences, Kyushu University, Fukuoka 812-8582, Japan; [email protected]; Tel.: +81-92-642-5581; Fax: +81-92-642-5600 2 Research and Clinical Center for Yusho and Dioxin, Kyushu University Hospital, Fukuoka 812-8582, Japan Received: 4 November 2020; Accepted: 19 November 2020; Published: 20 November 2020 Abstract: Atopic dermatitis (AD) is characterized by skin inflammation, barrier dysfunction, and chronic pruritus. As the anti-interleukin-4 (IL-4) receptor α antibody dupilumab improves all three cardinal features of AD, the type 2 cytokines IL-4 and especially IL-13 have been indicated to have pathogenic significance in AD. Accumulating evidence has shown that the skin barrier function is regulated via competition between the aryl hydrocarbon receptor (AHR) axis (up-regulation of barrier) and the IL-13/IL-4-JAK-STAT6/STAT3 axis (down-regulation of barrier). This latter axis also induces oxidative stress, which exacerbates inflammation. Conventional and recently developed agents for treating AD such as steroid, calcineurin inhibitors, cyclosporine, dupilumab, and JAK inhibitors inhibit the IL-13/IL-4-JAK-STAT6/STAT3 axis, while older remedies such as coal tar and glyteer are antioxidative AHR agonists. In this article, I summarize the pathogenic and therapeutic implications of the IL-13/IL-4-JAK-STAT6/STAT3 axis and the AHR axis in AD. -

List of Figures Viii Vi
Bidirectional IL-31-driven communication between T cells and basophils during atopic skin inflammation Inaugural-Dissertation for the attainment of the title of doctor in the Faculty of Mathematics and Natural Sciences at the Heinrich Heine University Düsseldorf presented by MSc. Angeliki Datsi from Ioannina (GR) Düsseldorf, April 2019 From the University Hospital Düsseldorf – Department of Dermatology, Research Laboratory for Dermato-Immunology and Oncology of the Heinrich-Heine-University Düsseldorf Printed with permission of the Faculty of Mathematics and Natural Sciences at the Heinrich-Heine-University Düsseldorf Supervisor: Univ.-Prof. Dr. med. Bernhard Homey Co-supervisor: Univ.-Prof. Dr. rer. nat. Eckhardt Lammert Date of the oral examination: 16.09.2019 Abstract I. Abstract The novel TH2-derived cytokine interleukin-31 (IL-31) has been implicated in the pathophysiology of atopic skin inflammation. Here for example, IL-31 has been identified to effectively elicit the cardinal AD symptom of pruritus (itch), relying on a synergistic cooperation of dysregulated immune cells and hyper-stimulated sensory neurons. This study aims to systematically characterize the phenotype of IL-31-producing T cells and to elucidate their interaction with basophils in the context of atopic skin inflammation. + Results of the present study could identify the unique characteristics of IL-31 TH2 cells presenting with a CRTH2+ CCR4+ CCR10+ CXCR3- CCR6- phenotype and a distribution among the effector memory (CD62L- CD45RO+) T cell subset. Furthermore, IL-31+ T cells associate with a marked increase of the skin-homing chemokine receptors CCR4, CCR8, and CCR10 in AD patients. Notably, the abundance of IL-31+ T cells but also the overall production of T cell-derived IL-31 was found increased in AD patients while frequencies of circulating basophils were not affected. -

Final Korrekturen 3
The role of IL-31 in skin barrier formation Von der Fakultät für Mathematik, Informatik und Naturwissenschaften der RWTH Aachen University zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaften genehmigte Dissertation vorgelegt von Master of Science Biotechnologie Kai Herbert Hänel aus Neuss Berichter: Universitätsprofessor Dr. rer. nat. Bernd Lüscher apl. Prof. Dr. rer. nat. Dirk Ostareck Tag der mündlichen Prüfung: 26.05.2015 Diese Dissertation ist auf den Internetseiten der Hochschulbibliothek online verfügbar. II No man should escape our universities without knowing how little he knows. J. Robert Oppenheimer Parts of this thesis were prepublished Hänel, K.H., Cornelissen, C., Lüscher, B., and Baron, J.M. (2013). Cytokines and the Skin Barrier. International Journal of Molecular Sciences, 14(4), 6720–6745. Hänel, K.H ., Cornelissen, C., Amann, P.M., Marquardt, Y., Czaja, K., Kim, A., Bickers, D.R., Lüscher, B. and Baron, J.M. Control of the mechanical and antimicrobial skin barrier by an IL-31 – IL-1 axis (manuscript submitted) III Abstract The skin is the largest organ in the human body and its major function is to protect from harmful environmental influences and to prevent dehydration. It forms the first barrier against biological, chemical and physical stress. Atopic dermatitis (AD) is a relapsing inflammatory skin disease. Hallmarks of AD are pruritic, eczematous erythematous plaques resulting in reduced skin barrier function, increasing transepidermal water loss and, affected by this, dry skin. AD commonly begins in early childhood and affects 10-20% of children and 1-3% of adults in industrialized countries. AD patients show significant higher levels of IL-31 in serum and increased IL31 mRNA levels in lesional skin samples. -

Mediators and Receptors of Chronic Itch in Primates and Humans
MEDIATORS AND RECEPTORS OF CHRONIC ITCH IN PRIMATES AND HUMANS A Dissertation Submitted to the Temple University Graduate Board In Partial Fulfillment of the Requirements for the Degree DOCTOR OF PHILOSOPHY by Leigh Ann Nattkemper December 2015 Examining Committee Members: Gil Yosipovitch, MD, Advisory Chair, Department of Dermatology Mary Barbe, PhD, Department of Anatomy and Cell Biology Liselotte Jensen, PhD, Department of Microbiology and Immunology Alan Cowan, PhD, Department of Pharmacology Mark Hoon, PhD, External Member, National Institutes of Health (NIDCR) © Copyright 2015 by Leigh Nattkemper All Rights Reserved ii ABSTRACT Chronic itch has a significant impact on quality of life for millions of patients worldwide, on a level comparable to that of chronic pain. Yet, although there are a host of effective drugs available for pain, there are no therapies that specifically target chronic itch. Current experimental approaches to investigate the pathogenesis of chronic pruritus and to test novel therapeutic agents are largely limited to rodent models. However, rodent models display significant dermatological, neurophysiological, and immunological differences from humans with chronic itch. The disadvantages of the current rodent paradigms call for the design of a valid primate model of chronic itch. For four years, we have monitored scratching behavior in a primate colony (n=35) of Cynomolgus macaques ( Macaca fascicularis ) suffering from idiopathic chronic itch. By comparing molecular and genetic analyses of the primates’ skin to their quantified scratching behavior, we attempted to characterize the underlying mechanisms of chronic itch in this model. Furthermore, the expression of itch-related proteins was examined in both the primate model and in humans with pruritic diseases.