01 종설 0017(35-46)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Drug Class Review Beta Adrenergic Blockers
Drug Class Review Beta Adrenergic Blockers Final Report Update 4 July 2009 Update 3: September 2007 Update 2: May 2005 Update 1: September 2004 Original Report: September 2003 The literature on this topic is scanned periodically. The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use, or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Mark Helfand, MD, MPH Kim Peterson, MS Vivian Christensen, PhD Tracy Dana, MLS Sujata Thakurta, MPA:HA Drug Effectiveness Review Project Marian McDonagh, PharmD, Principal Investigator Oregon Evidence-based Practice Center Mark Helfand, MD, MPH, Director Oregon Health & Science University Copyright © 2009 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 4 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION .......................................................................................................................... 6 Purpose and Limitations of Evidence Reports........................................................................................ 8 Scope and Key Questions .................................................................................................................... 10 METHODS................................................................................................................................. -

Inhibitory Effect of Eslicarbazepine Acetate and S-Licarbazepine on 2 Nav1.5 Channels
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.24.059188; this version posted August 14, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Inhibitory effect of eslicarbazepine acetate and S-licarbazepine on 2 Nav1.5 channels 3 Theresa K. Leslie1, Lotte Brückner 1, Sangeeta Chawla1,2, William J. Brackenbury1,2* 4 1Department of Biology, University of York, Heslington, York, YO10 5DD, UK 5 2York Biomedical Research Institute, University of York, Heslington, York, YO10 5DD, UK 6 * Correspondence: Dr William J. Brackenbury, Department of Biology and York Biomedical 7 Research Institute, University of York, Wentworth Way, Heslington, York YO10 5DD, UK. Email: 8 [email protected]. Tel: +44 1904 328284. 9 Keywords: Anticonvulsant, cancer, epilepsy, eslicarbazepine acetate, Nav1.5, S-licarbazepine, 10 voltage-gated Na+ channel. 11 Abstract 12 Eslicarbazepine acetate (ESL) is a dibenzazepine anticonvulsant approved as adjunctive treatment for 13 partial-onset epileptic seizures. Following first pass hydrolysis of ESL, S-licarbazepine (S-Lic) 14 represents around 95 % of circulating active metabolites. S-Lic is the main enantiomer responsible 15 for anticonvulsant activity and this is proposed to be through the blockade of voltage-gated Na+ 16 channels (VGSCs). ESL and S-Lic both have a voltage-dependent inhibitory effect on the Na+ current 17 in N1E-115 neuroblastoma cells expressing neuronal VGSC subtypes including Nav1.1, Nav1.2, 18 Nav1.3, Nav1.6 and Nav1.7. -
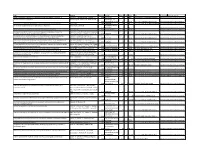
Preventive Report Appendix
Title Authors Published Journal Volume Issue Pages DOI Final Status Exclusion Reason Nasal sumatriptan is effective in treatment of migraine attacks in children: A Ahonen K.; Hamalainen ML.; Rantala H.; 2004 Neurology 62 6 883-7 10.1212/01.wnl.0000115105.05966.a7 Deemed irrelevant in initial screening Seasonal variation in migraine. Alstadhaug KB.; Salvesen R.; Bekkelund SI. Cephalalgia : an 2005 international journal 25 10 811-6 10.1111/j.1468-2982.2005.01018.x Deemed irrelevant in initial screening Flunarizine, a calcium channel blocker: a new prophylactic drug in migraine. Amery WK. 1983 Headache 23 2 70-4 10.1111/j.1526-4610.1983.hed2302070 Deemed irrelevant in initial screening Monoamine oxidase inhibitors in the control of migraine. Anthony M.; Lance JW. Proceedings of the 1970 Australian 7 45-7 Deemed irrelevant in initial screening Prostaglandins and prostaglandin receptor antagonism in migraine. Antonova M. 2013 Danish medical 60 5 B4635 Deemed irrelevant in initial screening Divalproex extended-release in adolescent migraine prophylaxis: results of a Apostol G.; Cady RK.; Laforet GA.; Robieson randomized, double-blind, placebo-controlled study. WZ.; Olson E.; Abi-Saab WM.; Saltarelli M. 2008 Headache 48 7 1012-25 10.1111/j.1526-4610.2008.01081.x Deemed irrelevant in initial screening Divalproex sodium extended-release for the prophylaxis of migraine headache in Apostol G.; Lewis DW.; Laforet GA.; adolescents: results of a stand-alone, long-term open-label safety study. Robieson WZ.; Fugate JM.; Abi-Saab WM.; 2009 Headache 49 1 45-53 10.1111/j.1526-4610.2008.01279.x Deemed irrelevant in initial screening Safety and tolerability of divalproex sodium extended-release in the prophylaxis of Apostol G.; Pakalnis A.; Laforet GA.; migraine headaches: results of an open-label extension trial in adolescents. -

8Th European Congress on Epileptology, Berlin, Germany, 21 – 25 September 2008
Epilepsia, 50(Suppl. 4): 2–262, 2009 doi: 10.1111/j.1528-1167.2009.02063.x 8th ECE PROCEEDINGS 8th European Congress on Epileptology, Berlin, Germany, 21 – 25 September 2008 Sunday 21 September 2008 KV7 channels (KV7.1-5) are encoded by five genes (KCNQ1-5). They have been identified in the last 10–15 years by discovering the caus- 14:30 – 16:00 ative genes for three autosomal dominant diseases: cardiac arrhythmia Hall 1 (long QT syndrome, KCNQ1), congenital deafness (KCNQ1 and KCNQ4), benign familial neonatal seizures (BFNS, KCNQ2 and VALEANT PHARMACEUTICALS SATELLITE SYM- KCNQ3), and peripheral nerve hyperexcitability (PNH, KCNQ2). The fifth member of this gene family (KCNQ5) is not affected in a disease so POSIUM – NEURON-SPECIFIC M-CURRENT K+ CHAN- far. The phenotypic spectrum associated with KCNQ2 mutations is prob- NELS: A NEW TARGET IN MANAGING EPILEPSY ably broader than initially thought (i.e. not only BFNS), as patients with E. Perucca severe epilepsies and developmental delay, or with Rolando epilepsy University of Pavia, Italy have been described. With regard to the underlying molecular pathophys- iology, it has been shown that mutations in KCNQ2 and KCNQ3 Innovations in protein biology, coupled with genetic manipulations, have decrease the resulting K+ current thereby explaining the occurrence of defined the structure and function of many of the voltage- and ligand- epileptic seizures by membrane depolarization and increased neuronal gated ion channels, channel subunits, and receptors that are the underpin- firing. Very subtle changes restricted to subthreshold voltages are suffi- nings of neuronal hyperexcitability and epilepsy. Of the currently cient to cause BFNS which proves in a human disease model that this is available antiepileptic drugs (AEDs), no two act in the same way, but all the relevant voltage range for these channels to modulate the firing rate. -

PR2 2009.Vp:Corelventura
Pharmacological Reports Copyright © 2009 2009, 61, 197216 by Institute of Pharmacology ISSN 1734-1140 Polish Academy of Sciences Review Third-generation antiepileptic drugs: mechanisms of action, pharmacokinetics and interactions Jarogniew J. £uszczki1,2 Department of Pathophysiology, Medical University of Lublin, Jaczewskiego 8, PL 20-090 Lublin, Poland Department of Physiopathology, Institute of Agricultural Medicine, Jaczewskiego 2, PL 20-950 Lublin, Poland Correspondence: Jarogniew J. £uszczki, e-mail: [email protected]; [email protected] Abstract: This review briefly summarizes the information on the molecular mechanisms of action, pharmacokinetic profiles and drug interac- tions of novel (third-generation) antiepileptic drugs, including brivaracetam, carabersat, carisbamate, DP-valproic acid, eslicar- bazepine, fluorofelbamate, fosphenytoin, ganaxolone, lacosamide, losigamone, pregabalin, remacemide, retigabine, rufinamide, safinamide, seletracetam, soretolide, stiripentol, talampanel, and valrocemide. These novel antiepileptic drugs undergo intensive clinical investigations to assess their efficacy and usefulness in the treatment of patients with refractory epilepsy. Key words: antiepileptic drugs, brivaracetam, carabersat, carisbamate, DP-valproic acid, drug interactions, eslicarbazepine, fluorofelbamate, fosphenytoin, ganaxolone, lacosamide, losigamone, pharmacokinetics, pregabalin, remacemide, retigabine, rufinamide, safinamide, seletracetam, soretolide, stiripentol, talampanel, valrocemide Abbreviations: 4-AP -

A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache
University of South Florida Masthead Logo Scholar Commons School of Information Faculty Publications School of Information 7-2015 A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache Authors: Jeffrey L. Jackson, Elizabeth Cogbill, Rafael Santana-Davila, Christina Eldredge, William Collier, Andrew Gradall, Neha Sehgal, and Jessica Kuester OBJECTIVE: To compare the effectiveness and side effects of migraine prophylactic medications. DESIGN: We performed a network meta-analysis. Data were extracted independently in duplicate and quality was assessed using both the JADAD and Cochrane Risk of Bias instruments. Data were pooled and network meta-analysis performed using random effects models. DATA SOURCES: PUBMED, EMBASE, Cochrane Trial Registry, bibliography of retrieved articles through 18 May 2014. ELIGIBILITY CRITERIA FOR SELECTING STUDIES: We included randomized controlled trials of adults with migraine headaches of at least 4 weeks in duration. RESULTS: Placebo controlled trials included alpha blockers (n = 9), angiotensin converting enzyme inhibitors (n = 3), angiotensin receptor blockers (n = 3), anticonvulsants (n = 32), beta-blockers (n = 39), calcium channel blockers (n = 12), flunarizine (n = 7), serotonin reuptake inhibitors (n = 6), serotonin norepinephrine reuptake inhibitors (n = 1) serotonin agonists (n = 9) and tricyclic antidepressants (n = 11). In addition there were 53 trials comparing different drugs. Drugs with at least 3 trials that were more effective than placebo for episodic migraines -

Molecular Mechanisms of Antiseizure Drug Activity at GABAA Receptors
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Seizure 22 (2013) 589–600 Contents lists available at SciVerse ScienceDirect Seizure jou rnal homepage: www.elsevier.com/locate/yseiz Review Molecular mechanisms of antiseizure drug activity at GABAA receptors L. John Greenfield Jr.* Dept. of Neurology, University of Arkansas for Medical Sciences, 4301W. Markham St., Slot 500, Little Rock, AR 72205, United States A R T I C L E I N F O A B S T R A C T Article history: The GABAA receptor (GABAAR) is a major target of antiseizure drugs (ASDs). A variety of agents that act at Received 6 February 2013 GABAARs s are used to terminate or prevent seizures. Many act at distinct receptor sites determined by Received in revised form 16 April 2013 the subunit composition of the holoreceptor. For the benzodiazepines, barbiturates, and loreclezole, Accepted 17 April 2013 actions at the GABAAR are the primary or only known mechanism of antiseizure action. For topiramate, felbamate, retigabine, losigamone and stiripentol, GABAAR modulation is one of several possible Keywords: antiseizure mechanisms. Allopregnanolone, a progesterone metabolite that enhances GABAAR function, Inhibition led to the development of ganaxolone. Other agents modulate GABAergic ‘‘tone’’ by regulating the Epilepsy synthesis, transport or breakdown of GABA. GABAAR efficacy is also affected by the transmembrane Antiepileptic drugs chloride gradient, which changes during development and in chronic epilepsy. This may provide an GABA receptor Seizures additional target for ‘‘GABAergic’’ ASDs. GABAAR subunit changes occur both acutely during status Chloride channel epilepticus and in chronic epilepsy, which alter both intrinsic GABAAR function and the response to GABAAR-acting ASDs. -

Formulation and Evaluation of Ranolazine Extended Release Tablets: Influence of Polymers
Formulation and evaluation of ranolazine extended release tablets: Influence of polymers Murthy TEGK, Bala Vishnu Priya Mukkala, Suresh Babu VV1 Department of Pharmaceutics, Bapatla College of Pharmacy, Bapatla, Guntur, Andhra Pradesh, 1Natco Pharma Limited, Kothur, Hyderabad, Andhra Pradesh, India n extended release tablet provides prolonged periods of drug in plasma levels thereby reduce dosing frequency, Aimprove patient compliance and reduce the dose-related side effects. Ranolazine is indicated for the chronic treatment of angina in patients who have not achieved an adequate response with other anti-anginal agents. The present investigation was undertaken to design extended release tablets of Ranolazine employing hypromellose phthalate grade HP-55, ethocel standard 7FP premium ethyl cellulose, Surelease E-7-19040, Klucel HF pharm and Natrosol Type 250 HHX as matrix forming RESEARCH ARTICLE agents using wet granulation method. Formulated tablets were evaluated for uniformity of weight, assay, water content, in vitro drug release studies and stability studies. The drug release followed first order kinetics with both erosion and diffusion as the release mechanism. It is concluded that the desired drug release pattern can be obtained by using natrosol type 250 HHX compared to other polymers. The similarity factor (f2) was calculated to select best formulation by comparing in vitro dissolution data of the commercial formulation Ranexa®. The formulated tablets fulfilled the compendia requirements. The formulated Ranolazine Extended release tablets were found to be stable. Key words: Ehocel, extended release tablets, hypromellose phthalate, klucel HF pharm and natrosol, ranolazine, surelease INTRODUCTION MATERIALS AND METHODS Extended release drug delivery technology can provide Ranolazine was procured from the Natco Pharma smooth plasma levels of drug over longer periods of Ltd, Hyderabad. -

Rat Animal Models for Screening Medications to Treat Alcohol Use Disorders
ACCEPTED MANUSCRIPT Selectively Bred Rats Page 1 of 75 Rat Animal Models for Screening Medications to Treat Alcohol Use Disorders Richard L. Bell*1, Sheketha R. Hauser1, Tiebing Liang2, Youssef Sari3, Antoinette Maldonado-Devincci4, and Zachary A. Rodd1 1Indiana University School of Medicine, Department of Psychiatry, Indianapolis, IN 46202, USA 2Indiana University School of Medicine, Department of Gastroenterology, Indianapolis, IN 46202, USA 3University of Toledo, Department of Pharmacology, Toledo, OH 43614, USA 4North Carolina A&T University, Department of Psychology, Greensboro, NC 27411, USA *Send correspondence to: Richard L. Bell, Ph.D.; Associate Professor; Department of Psychiatry; Indiana University School of Medicine; Neuroscience Research Building, NB300C; 320 West 15th Street; Indianapolis, IN 46202; e-mail: [email protected] MANUSCRIPT Key Words: alcohol use disorder; alcoholism; genetically predisposed; selectively bred; pharmacotherapy; family history positive; AA; HAD; P; msP; sP; UChB; WHP Chemical compounds studied in this article Ethanol (PubChem CID: 702); Acamprosate (PubChem CID: 71158); Baclofen (PubChem CID: 2284); Ceftriaxone (PubChem CID: 5479530); Fluoxetine (PubChem CID: 3386); Naltrexone (PubChem CID: 5360515); Prazosin (PubChem CID: 4893); Rolipram (PubChem CID: 5092); Topiramate (PubChem CID: 5284627); Varenicline (PubChem CID: 5310966) ACCEPTED _________________________________________________________________________________ This is the author's manuscript of the article published in final edited form as: Bell, R. L., Hauser, S. R., Liang, T., Sari, Y., Maldonado-Devincci, A., & Rodd, Z. A. (2017). Rat animal models for screening medications to treat alcohol use disorders. Neuropharmacology. https://doi.org/10.1016/j.neuropharm.2017.02.004 ACCEPTED MANUSCRIPT Selectively Bred Rats Page 2 of 75 The purpose of this review is to present animal research models that can be used to screen and/or repurpose medications for the treatment of alcohol abuse and dependence. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Ranexa, INN:Ranolazine
European Medicines Agency Doc. Ref.: EMEA/CHMP/643056/2009 EMEA/H/C/805 Ranexa1 ranolazine EPAR summary for the public This document is a summary of the European Public Assessment Report (EPAR). It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the studies performed, to reach their recommendations on how to use the medicine. If you need more information about your medical condition or your treatment, read the Package Leaflet (also part of the EPAR) or contact your doctor or pharmacist. If you want more information on the basis of the CHMP recommendations, read the Scientific Discussion (also part of the EPAR). What is Ranexa? Ranexa is a medicine that contains the active substance ranolazine. It is available as oval prolonged- release tablets (blue: 375 mg; orange: 500 mg; green: 750 mg). ‘Prolonged release’ means that ranolazine is released slowly from the tablet over a few hours. What is Ranexa used for? Ranexa is used to treat the symptoms of stable angina pectoris (chest pain caused by reduced blood flow to the heart). It is used as an add-on to existing treatment in patients whose disease is not adequately controlled by other medicines for angina pectoris, such as beta-blockers or calcium antagonists, or in patients who cannot take these medicines. The medicine can only be obtained with a prescription. How is Ranexa used? The recommended starting dose of Ranexa is 375 mg twice a day. After two to four weeks, the dose should be increased to 500 mg twice a day, and then to 750 mg twice a day, depending on the patient’s response. -

Medcompgx Med List
For more info, go to: MedCompGx.com Medications Conditions / Uses Other Uses CYP2C19 Anticonvulsants Lacosamide (Vimpat) Epilepsy, Seizures Phenobarbital (Luminal) Epilepsy, Seizures Barbituates, Anxiety, Sedation, Withdrawl Primidone (Mysoline) Epilepsy, Seizures Zonisamide (Zonegran) Epilepsy, Seizures Antifungals Voriconazole (Vfend) Yeast Infections, Candidiasis, Aspergillosis, Candida, Aspergillus Antidepressants Escitalopram (Lexapro) SSRI, Depression, Anxiety Citalopram (Celexa) SSRI, Depression, Anxiety OCD Sertraline (Zoloft) SSRI, Depression, Anxiety OCD, PTSD Doxepin (Silenor) Tricyclic Antidepressant, Depression Bipolar, Insomnia Imipramine (Tofranil) Tricyclic Antidepressant, Depression Trimipramine (Surmontil) Tricyclic Antidepressant, Depression Amitriptyline (Elavil) Tricyclic Antidepressant, Depression Clomipramine (Anafranil) Tricyclic Antidepressant, Depression OCD Benzodiazepines Clobazam (Onfi) Seizures Diazepam (Valium) Seizures, Muscle Spasms, Anxiety, Alcohol Withdrawl Beta Blockers Labetalol (Normodyne, Trandate) High Blood Pressure, Hypertension Immunomodulators Leflunomide (Arava) Rheumatoid Arthritis Tofacitinib (Xeljanz) Rheumatoid Arthritis Muscle Relaxants Carisoprodol (Soma) Muscle Pain, Muscle Spasms Opioids Meperidine (Demerol) Pain, Severe Pain, Narcotic, Opiate Proton Pump Inhibitors Dexlansoprazole (Dexilant) GERD, Acid Reflux, Gastric Esophageal Reflux, Ulcers, Heartburn, Zollinger-Ellison Syndrome Esomeprazole (Nexium) GERD, Acid Reflux, Gastric Esophageal Reflux, Ulcers, Heartburn, Zollinger-Ellison