Anaesthetic Guideline for the Management of Children with Long QT Syndrome SOP/Protocol Detail Owner: Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Drug Class Review Beta Adrenergic Blockers
Drug Class Review Beta Adrenergic Blockers Final Report Update 4 July 2009 Update 3: September 2007 Update 2: May 2005 Update 1: September 2004 Original Report: September 2003 The literature on this topic is scanned periodically. The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use, or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Mark Helfand, MD, MPH Kim Peterson, MS Vivian Christensen, PhD Tracy Dana, MLS Sujata Thakurta, MPA:HA Drug Effectiveness Review Project Marian McDonagh, PharmD, Principal Investigator Oregon Evidence-based Practice Center Mark Helfand, MD, MPH, Director Oregon Health & Science University Copyright © 2009 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 4 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION .......................................................................................................................... 6 Purpose and Limitations of Evidence Reports........................................................................................ 8 Scope and Key Questions .................................................................................................................... 10 METHODS................................................................................................................................. -

QT Prolongation Due to Roxithromycin
Postgrad Med J 2000;76:651–654 651 Postgrad Med J: first published as 10.1136/pmj.76.900.651 on 1 October 2000. Downloaded from ADVERSE DRUG REACTION QT prolongation due to roxithromycin A Woywodt, U Grommas, W Buth, W RaZenbeul Roxithromycin and other macrolide antimicro- placement of the apex beat, a prominent third bials are widely used for a broad variety of heart sound, coarse rales over both lung fields infections such as upper respiratory tract infec- and pitting oedema of both ankles. The patient tion and community acquired pneumonia. was taken to an intensive care unit. Acute myo- Prolongation of the QT interval, torsade de cardial infarction was ruled out and frusemide pointes polymorphic ventricular tachycardia, was begun intravenously. An electrocardio- and sudden death are well described but little gram (ECG) on admission showed sinus known adverse reactions common to all rhythm and incomplete left bundle branch macrolides. We report the case of a 72 year old block; QT intervals were normal (QT interval patient with congestive heart failure caused by 380 ms, corrected QT interval according to University of ischaemic heart disease who developed severe Bazett’s formula [QTc] 390 ms). Roxithromy- Hannover Medical prolongation of the QT interval after three days cin (Roussel UCLAF, Romainville, France) School, 30623 of treatment with roxithromycin. 150 mg twice a day was initiated for suspected Hannover, Germany: pneumonia. On the third hospital day, he was Department of Nephrology Case report transferred to a general medical ward. A Woywodt A 72 year old man presented with severe On admission there, the patient was gener- W Buth congestive heart failure. -

Inhibitory Effect of Eslicarbazepine Acetate and S-Licarbazepine on 2 Nav1.5 Channels
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.24.059188; this version posted August 14, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Inhibitory effect of eslicarbazepine acetate and S-licarbazepine on 2 Nav1.5 channels 3 Theresa K. Leslie1, Lotte Brückner 1, Sangeeta Chawla1,2, William J. Brackenbury1,2* 4 1Department of Biology, University of York, Heslington, York, YO10 5DD, UK 5 2York Biomedical Research Institute, University of York, Heslington, York, YO10 5DD, UK 6 * Correspondence: Dr William J. Brackenbury, Department of Biology and York Biomedical 7 Research Institute, University of York, Wentworth Way, Heslington, York YO10 5DD, UK. Email: 8 [email protected]. Tel: +44 1904 328284. 9 Keywords: Anticonvulsant, cancer, epilepsy, eslicarbazepine acetate, Nav1.5, S-licarbazepine, 10 voltage-gated Na+ channel. 11 Abstract 12 Eslicarbazepine acetate (ESL) is a dibenzazepine anticonvulsant approved as adjunctive treatment for 13 partial-onset epileptic seizures. Following first pass hydrolysis of ESL, S-licarbazepine (S-Lic) 14 represents around 95 % of circulating active metabolites. S-Lic is the main enantiomer responsible 15 for anticonvulsant activity and this is proposed to be through the blockade of voltage-gated Na+ 16 channels (VGSCs). ESL and S-Lic both have a voltage-dependent inhibitory effect on the Na+ current 17 in N1E-115 neuroblastoma cells expressing neuronal VGSC subtypes including Nav1.1, Nav1.2, 18 Nav1.3, Nav1.6 and Nav1.7. -

Ventricular Arrhythmias Associated with Lidoflazine: Side-Effects Observed in a Randomized Trial •Y
European Heart Journal (1983) 4, 889-893 Ventricular arrhythmias associated with lidoflazine: side-effects observed in a randomized trial •y- S. P. HANLEY AND J. R. HAMPTON Department of Medicine, University Hospital, Queen's Medical Centre, Nottingham NG7 2UH, U.K. Downloaded from https://academic.oup.com/eurheartj/article/4/12/889/503490 by guest on 29 September 2021 KEY WORDS: Angina, exercise testing, lidoflazine, propranolol, ventricular tachycardia. Twenty-four patients received either propranolol, lidoflazine (Clinium), or propranolol/lidoflazine com- binations in a study designed to evaluate the effect of these drugs in angina pectoris. Five patients developed ventricular tachycardia when receiving either lidoflazine or lidoflazine and propranolol in combination; one of these patients died. In addition, one patient died suddenly while being treated with propranolol alone. Lidoflazine therapy was associated with a significant prolongation of the QT interval of the electro- cardiogram. Lidoflazine either alone or in combination with propranolol, appears to induce ventricular tachycardia. Introduction patients already being treated with a beta-blocking, Patients with ischaemic heart disease have an whose symptoms were not adequately controlled; increased risk of death and of developing arrhyth- the second protocol was designed for patients who mias: in any clinical trial of a potential therapeutic were receiving no other treatment other than sub- agent for angina, such events are likely to occur by lingual glyceryl trinitrate. None of thqse patients chance. During a study of lidoflazine we detected was in clinical heart failure. In each of these studies an unacceptable incidence of arrhythmias which exercise tolerance was assessed by treadmill testing led us to discontinue the investigation. -
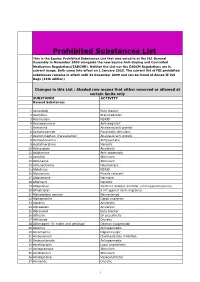
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Studies on the Possible Mechanisms of Lidoflazine Arrhythmogenicity
742 lACC Vol 4, No 4 October 1984 742- 7 Studies on the Possible Mechanisms of Lidoflazine Arrhythmogenicity GAD KEREN, MD, DAVID TEPPER, BA, BRENDA BUTLER, BA, WILLIAM MAGUIRE, MD, PHD, HOWARD WILLENS, MD, DENNIS MIURA, MD, PHD , JOHN C. SaMBERG, MD Bronx. New York Lidoftazine is a calcium channel blocking agent that is Dogsalso underwent programmed electrical stimulation effective and safe in the treatment of angina pectoris, while not receiving medications and then after incre but has been reported to be associated with sudden death mental doses of lidoftazine administered intravenously. when administered for the treatment of supraventricular Lidoflazinedid not cause spontaneous ventricular tachy arrhythmias. Studies were performed in dogs to deter cardia and did not lower the threshold of ventricular mine if lidoflazine caused a rise in serum digoxin con tachycardia induction. Combined administration of Ii centration that could cause arrhythmias or if it was di doflazine and digoxin did not facilitate arrhythmia in rectly arrhythmogenic. Dogsreceived chronic injections duction. These studies do not support a digoxin-lido of digoxin and then digoxin in combination with lido f1azine interaction or a direct arrhythmogenic action of ftazine. No increase in digoxin concentration was found. Iidoflazine. Several clinical studies (1-3) have shown the effectiveness Thus. we undertook studies in dogs to test if a digoxin and safety of lidoflazine in the control of angina pectoris. lidoflazine interaction exists and causes a rise in serum di However, in patients with atrial fibril1ation receiving digi goxin levels . Another series of studies used programmed talis therapy and being treated with Iidoflazine to convert electrical stimulation techniques to determine whether suc the supraventricular arrhythmia. -

Formulation and Evaluation of Ranolazine Extended Release Tablets: Influence of Polymers
Formulation and evaluation of ranolazine extended release tablets: Influence of polymers Murthy TEGK, Bala Vishnu Priya Mukkala, Suresh Babu VV1 Department of Pharmaceutics, Bapatla College of Pharmacy, Bapatla, Guntur, Andhra Pradesh, 1Natco Pharma Limited, Kothur, Hyderabad, Andhra Pradesh, India n extended release tablet provides prolonged periods of drug in plasma levels thereby reduce dosing frequency, Aimprove patient compliance and reduce the dose-related side effects. Ranolazine is indicated for the chronic treatment of angina in patients who have not achieved an adequate response with other anti-anginal agents. The present investigation was undertaken to design extended release tablets of Ranolazine employing hypromellose phthalate grade HP-55, ethocel standard 7FP premium ethyl cellulose, Surelease E-7-19040, Klucel HF pharm and Natrosol Type 250 HHX as matrix forming RESEARCH ARTICLE agents using wet granulation method. Formulated tablets were evaluated for uniformity of weight, assay, water content, in vitro drug release studies and stability studies. The drug release followed first order kinetics with both erosion and diffusion as the release mechanism. It is concluded that the desired drug release pattern can be obtained by using natrosol type 250 HHX compared to other polymers. The similarity factor (f2) was calculated to select best formulation by comparing in vitro dissolution data of the commercial formulation Ranexa®. The formulated tablets fulfilled the compendia requirements. The formulated Ranolazine Extended release tablets were found to be stable. Key words: Ehocel, extended release tablets, hypromellose phthalate, klucel HF pharm and natrosol, ranolazine, surelease INTRODUCTION MATERIALS AND METHODS Extended release drug delivery technology can provide Ranolazine was procured from the Natco Pharma smooth plasma levels of drug over longer periods of Ltd, Hyderabad. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Drug Induced Long QT Syndromes: Lethal Reactions to ‘Benign Drugs’ - May/2005 Dr
Drug Induced Long QT Syndromes: Lethal Reactions to ‘Benign Drugs’ - May/2005 Dr. R.G.Williams Long QT syndrome (LQTS) ¾ A disorder of myocardial repolarization characterized by a prolonged QT interval on ECG. ¾ ↑ risk of a characteristic life-threatening cardiac arrhythmia, known as torsade de pointes (TdP) VT. ¾ Drug induced usually with bradycardia ¾ Short-long cycles 2o VPBs ¾ Present with: z Palpitations z Syncope z Seizures z Sudden cardiac death (SCD) ¾ Congenital – 2 phenotypes z Romano – Ward: more common, purely cardiac • Autosomal dominant z Jervell + Lange-Nielsen: sensorineural deafness • Autosomal recessive ¾ At least 7 genes described LQTS 1 - 7 ¾ Affect Na and K channels ¾ Acquired LQTS may be a ‘forme fruste’ Acquired LQTS ¾ Commonest causes z Medications z Electrolyte disorders ¾ Others z Structural heart disease z Stroke + brain injury z HIV z Eating disorders May, 2005 1 Talk edited into handout by RAS Long QT of Hypocalcemia May, 2005 2 Talk edited into handout by RAS Drug Induced LQTS ¾ First recognized in 1920s – quinidine syncope ¾ Monitoring identified typical sequences in TdP in 1960s ¾ In the past decade, the single most common cause of the withdrawal or restriction of the use of drugs that have already been marketed has been the prolongation of the QT interval associated with polymorphic ventricular tachycardia, or torsade de pointes. ¾ Nine structurally unrelated drugs removed or severely restricted due to QT ↑ + TdP. Risk Factors for TdP ¾ Drug regimen: z Not usually an idiosyncratic event z ↑drug dose or -

Drugs for Primary Prevention of Atherosclerotic Cardiovascular Disease: an Overview of Systematic Reviews
Supplementary Online Content Karmali KN, Lloyd-Jones DM, Berendsen MA, et al. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. Published online April 27, 2016. doi:10.1001/jamacardio.2016.0218. eAppendix 1. Search Documentation Details eAppendix 2. Background, Methods, and Results of Systematic Review of Combination Drug Therapy to Evaluate for Potential Interaction of Effects eAppendix 3. PRISMA Flow Charts for Each Drug Class and Detailed Systematic Review Characteristics and Summary of Included Systematic Reviews and Meta-analyses eAppendix 4. List of Excluded Studies and Reasons for Exclusion This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. 1 Downloaded From: https://jamanetwork.com/ on 09/28/2021 eAppendix 1. Search Documentation Details. Database Organizing body Purpose Pros Cons Cochrane Cochrane Library in Database of all available -Curated by the Cochrane -Content is limited to Database of the United Kingdom systematic reviews and Collaboration reviews completed Systematic (UK) protocols published by by the Cochrane Reviews the Cochrane -Only systematic reviews Collaboration Collaboration and systematic review protocols Database of National Health Collection of structured -Curated by Centre for -Only provides Abstracts of Services (NHS) abstracts and Reviews and Dissemination structured abstracts Reviews of Centre for Reviews bibliographic -

Ranexa, INN:Ranolazine
European Medicines Agency Doc. Ref.: EMEA/CHMP/643056/2009 EMEA/H/C/805 Ranexa1 ranolazine EPAR summary for the public This document is a summary of the European Public Assessment Report (EPAR). It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the studies performed, to reach their recommendations on how to use the medicine. If you need more information about your medical condition or your treatment, read the Package Leaflet (also part of the EPAR) or contact your doctor or pharmacist. If you want more information on the basis of the CHMP recommendations, read the Scientific Discussion (also part of the EPAR). What is Ranexa? Ranexa is a medicine that contains the active substance ranolazine. It is available as oval prolonged- release tablets (blue: 375 mg; orange: 500 mg; green: 750 mg). ‘Prolonged release’ means that ranolazine is released slowly from the tablet over a few hours. What is Ranexa used for? Ranexa is used to treat the symptoms of stable angina pectoris (chest pain caused by reduced blood flow to the heart). It is used as an add-on to existing treatment in patients whose disease is not adequately controlled by other medicines for angina pectoris, such as beta-blockers or calcium antagonists, or in patients who cannot take these medicines. The medicine can only be obtained with a prescription. How is Ranexa used? The recommended starting dose of Ranexa is 375 mg twice a day. After two to four weeks, the dose should be increased to 500 mg twice a day, and then to 750 mg twice a day, depending on the patient’s response. -

Medcompgx Med List
For more info, go to: MedCompGx.com Medications Conditions / Uses Other Uses CYP2C19 Anticonvulsants Lacosamide (Vimpat) Epilepsy, Seizures Phenobarbital (Luminal) Epilepsy, Seizures Barbituates, Anxiety, Sedation, Withdrawl Primidone (Mysoline) Epilepsy, Seizures Zonisamide (Zonegran) Epilepsy, Seizures Antifungals Voriconazole (Vfend) Yeast Infections, Candidiasis, Aspergillosis, Candida, Aspergillus Antidepressants Escitalopram (Lexapro) SSRI, Depression, Anxiety Citalopram (Celexa) SSRI, Depression, Anxiety OCD Sertraline (Zoloft) SSRI, Depression, Anxiety OCD, PTSD Doxepin (Silenor) Tricyclic Antidepressant, Depression Bipolar, Insomnia Imipramine (Tofranil) Tricyclic Antidepressant, Depression Trimipramine (Surmontil) Tricyclic Antidepressant, Depression Amitriptyline (Elavil) Tricyclic Antidepressant, Depression Clomipramine (Anafranil) Tricyclic Antidepressant, Depression OCD Benzodiazepines Clobazam (Onfi) Seizures Diazepam (Valium) Seizures, Muscle Spasms, Anxiety, Alcohol Withdrawl Beta Blockers Labetalol (Normodyne, Trandate) High Blood Pressure, Hypertension Immunomodulators Leflunomide (Arava) Rheumatoid Arthritis Tofacitinib (Xeljanz) Rheumatoid Arthritis Muscle Relaxants Carisoprodol (Soma) Muscle Pain, Muscle Spasms Opioids Meperidine (Demerol) Pain, Severe Pain, Narcotic, Opiate Proton Pump Inhibitors Dexlansoprazole (Dexilant) GERD, Acid Reflux, Gastric Esophageal Reflux, Ulcers, Heartburn, Zollinger-Ellison Syndrome Esomeprazole (Nexium) GERD, Acid Reflux, Gastric Esophageal Reflux, Ulcers, Heartburn, Zollinger-Ellison