Cloning and Expression of Deoxyhypusine Synthase from Plasmodium Vivax and Theileria Parva As an Approach for Target Evaluation in Anti-Parasitic Chemotherapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Yeast Genome Gazetteer P35-65
gazetteer Metabolism 35 tRNA modification mitochondrial transport amino-acid metabolism other tRNA-transcription activities vesicular transport (Golgi network, etc.) nitrogen and sulphur metabolism mRNA synthesis peroxisomal transport nucleotide metabolism mRNA processing (splicing) vacuolar transport phosphate metabolism mRNA processing (5’-end, 3’-end processing extracellular transport carbohydrate metabolism and mRNA degradation) cellular import lipid, fatty-acid and sterol metabolism other mRNA-transcription activities other intracellular-transport activities biosynthesis of vitamins, cofactors and RNA transport prosthetic groups other transcription activities Cellular organization and biogenesis 54 ionic homeostasis organization and biogenesis of cell wall and Protein synthesis 48 plasma membrane Energy 40 ribosomal proteins organization and biogenesis of glycolysis translation (initiation,elongation and cytoskeleton gluconeogenesis termination) organization and biogenesis of endoplasmic pentose-phosphate pathway translational control reticulum and Golgi tricarboxylic-acid pathway tRNA synthetases organization and biogenesis of chromosome respiration other protein-synthesis activities structure fermentation mitochondrial organization and biogenesis metabolism of energy reserves (glycogen Protein destination 49 peroxisomal organization and biogenesis and trehalose) protein folding and stabilization endosomal organization and biogenesis other energy-generation activities protein targeting, sorting and translocation vacuolar and lysosomal -

Symphytum Officinale) Hairy Roots by Rnai Silencing of Homospermidine Synthase
Published online: 2019-08-26 Original Papers Reduction of Pyrrolizidine Alkaloid Levels in Comfrey (Symphytum officinale) Hairy Roots by RNAi Silencing of Homospermidine Synthase Authors Lars H. Kruse 1, 3, Thomas Stegemann1, Julia Jensen-Kroll 1, Annika Engelhardt 1, Anne-Maria Wesseling 1, Annemarie Lippert 2, Jutta Ludwig-Müller 2,DietrichOber1 Affiliations ABSTRACT 1 Botanisches Institut, Kiel University, Kiel, Germany Comfrey is a medicinal plant, extracts of which are tradition- 2 Institut für Botanik, Technische Universität Dresden, ally used for the treatment of painful inflammatory muscle Dresden, Germany and joint problems, because the plant contains allantoin and 3 Plant Biology Section, School of Integrative Plant Science, rosmarinic acid. However, its medicinal use is limited because Cornell University, USA of its toxic pyrrolizidine alkaloid (PA) content. PAs encompass more than 400 different compounds that have been identified Key words from various plant lineages. To date, only the first pathway- Symphytum officinale, alkaloid extraction, transgenic tissue specific enzyme, homospermidine synthase (HSS), has been culture, transcript quantification, Boraginaceae characterized. HSS catalyzes the formation of homospermi- dine, which is exclusively incorporated into PAs. HSS has been received May 6, 2019 recruited several times independently in various plant line- revised August 5, 2019 ages during evolution by duplication of the gene encoding de- accepted August 15, 2019 oxyhypusine synthase (DHS), an enzyme of primary metabo- Bibliography lism. Here, we describe the establishment of RNAi knockdown DOI https://doi.org/10.1055/a-0998-5125 hairy root mutants of HSS in Symphytum officinale. A knock- – Published online August 26, 2019 | Planta Med 2019; 85: down of HSS by 60 80% resulted in a significant reduction of 1177–1186 © Georg Thieme Verlag KG Stuttgart · New York | homospermidine by ~ 86% and of the major PA components ‑ ‑ ISSN 0032‑0943 7 acetylintermedine N-oxide and 3 acetylmyoscorpine N-ox- ide by approximately 60%. -

Anti-Inflammatory Role of Curcumin in LPS Treated A549 Cells at Global Proteome Level and on Mycobacterial Infection
Anti-inflammatory Role of Curcumin in LPS Treated A549 cells at Global Proteome level and on Mycobacterial infection. Suchita Singh1,+, Rakesh Arya2,3,+, Rhishikesh R Bargaje1, Mrinal Kumar Das2,4, Subia Akram2, Hossain Md. Faruquee2,5, Rajendra Kumar Behera3, Ranjan Kumar Nanda2,*, Anurag Agrawal1 1Center of Excellence for Translational Research in Asthma and Lung Disease, CSIR- Institute of Genomics and Integrative Biology, New Delhi, 110025, India. 2Translational Health Group, International Centre for Genetic Engineering and Biotechnology, New Delhi, 110067, India. 3School of Life Sciences, Sambalpur University, Jyoti Vihar, Sambalpur, Orissa, 768019, India. 4Department of Respiratory Sciences, #211, Maurice Shock Building, University of Leicester, LE1 9HN 5Department of Biotechnology and Genetic Engineering, Islamic University, Kushtia- 7003, Bangladesh. +Contributed equally for this work. S-1 70 G1 S 60 G2/M 50 40 30 % of cells 20 10 0 CURI LPSI LPSCUR Figure S1: Effect of curcumin and/or LPS treatment on A549 cell viability A549 cells were treated with curcumin (10 µM) and/or LPS or 1 µg/ml for the indicated times and after fixation were stained with propidium iodide and Annexin V-FITC. The DNA contents were determined by flow cytometry to calculate percentage of cells present in each phase of the cell cycle (G1, S and G2/M) using Flowing analysis software. S-2 Figure S2: Total proteins identified in all the three experiments and their distribution betwee curcumin and/or LPS treated conditions. The proteins showing differential expressions (log2 fold change≥2) in these experiments were presented in the venn diagram and certain number of proteins are common in all three experiments. -

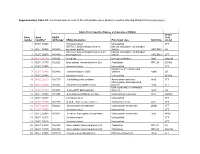
Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Pyrrolizidine Alkaloids: Biosynthesis, Biological Activities and Occurrence in Crop Plants
molecules Review Pyrrolizidine Alkaloids: Biosynthesis, Biological Activities and Occurrence in Crop Plants Sebastian Schramm, Nikolai Köhler and Wilfried Rozhon * Biotechnology of Horticultural Crops, TUM School of Life Sciences Weihenstephan, Technical University of Munich, Liesel-Beckmann-Straße 1, 85354 Freising, Germany; [email protected] (S.S.); [email protected] (N.K.) * Correspondence: [email protected]; Tel.: +49-8161-71-2023 Academic Editor: John C. D’Auria Received: 20 December 2018; Accepted: 29 January 2019; Published: 30 January 2019 Abstract: Pyrrolizidine alkaloids (PAs) are heterocyclic secondary metabolites with a typical pyrrolizidine motif predominantly produced by plants as defense chemicals against herbivores. They display a wide structural diversity and occur in a vast number of species with novel structures and occurrences continuously being discovered. These alkaloids exhibit strong hepatotoxic, genotoxic, cytotoxic, tumorigenic, and neurotoxic activities, and thereby pose a serious threat to the health of humans since they are known contaminants of foods including grain, milk, honey, and eggs, as well as plant derived pharmaceuticals and food supplements. Livestock and fodder can be affected due to PA-containing plants on pastures and fields. Despite their importance as toxic contaminants of agricultural products, there is limited knowledge about their biosynthesis. While the intermediates were well defined by feeding experiments, only one enzyme involved in PA biosynthesis has been characterized so far, the homospermidine synthase catalyzing the first committed step in PA biosynthesis. This review gives an overview about structural diversity of PAs, biosynthetic pathways of necine base, and necic acid formation and how PA accumulation is regulated. Furthermore, we discuss their role in plant ecology and their modes of toxicity towards humans and animals. -

REVIEW ARTICLES Pyrrolizidine Alkaloids
Review articles Pyrrolizidine alkaloids – chemistry, biosynthesis, pathway, toxicity, safety and perspectives of medicinal usage Mariola DREGER, MARZENA Stanisławska, ANNA Krajewska-Patan, SEBASTIAN Mielcarek, Przemysław Łukasz Mikołajczak, WALDEMAR Buchwald The Branch of Medicinal Plants Institute of Natural Fibres and Medicinal Plants Libelta 27 61-707 Poznań, Poland *corresponding author: [email protected] S u m m a r y Pyrrolizidine alkaloids (PAs) are the class of secondary metabolites that evolved as a powerful tool in the plant defensive interactions against herbivores. The occurrence of PAs in the plant world is scattered in several unrelated botanic families with special abun- dance in Asteraceae, Boraginaceae and Fabaceae. Homospermidine synthase (HSS) was recognized as a key enzyme that catalyzes homospermidine formation from polyamines. The studies of HSS kinetic and gene sequence revealed that it is of polyphyletic origin and raised as a result of deoxyhypusine synthase (DHS) gene duplication. The ability of PAs production occurred independently at least four times in course of plant evolution. The PAs biosynthesis is tightly correlated with growth phase and biomass production. It is sup- posed that PAs biosynthesis is individually regulated in different lineages of plants. The PAs with a 1,2 unsaturated necine skeleton show toxic activity (hepatoxicity, carcinogenicity, genotoxicity, teratogenocity and cytotoxicity). It is though that pyrrolic esters formation during the detoxication process in the liver is the main mechanism of PAs toxicity. The pyr- rolic esters are highly reactive and tend to bind rapidly with nucleophilic macromolecules including DNA and DNA-protein inducing hepatotoxicity or tumorigenecity. The problem of PAs toxicity cause the restrictions in the production and sale of herbal products. -

University of Florida Thesis Or Dissertation Formatting Template
METABOLOMIC CHARACTERIZATION OF THE INTESTINAL BACTERIAL OXALOBIOME By CASEY A. CHAMBERLAIN A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2019 © 2019 Casey A. Chamberlain To my wife, Michelle ACKNOWLEDGMENTS Obtaining a PhD may only bestow the title of “Doctor” upon one individual, but the journey to such an achievement is often aided by, and impossible without, the loving support of family, friends, and others along the way. I am thankful for the Lord for His providence and love and for blessing me with the unique interests, talents, and gifts that gave me the opportunity to fulfill this achievement. I am eternally grateful for my wife, Michelle, for providing me with love, support, comfort, and guidance, which propagates confidence, happiness, and fulfillment into all areas of my life. Her guiding and strengthening example has molded me into the man I am today. I am blessed to have my daughter, Maci, who reminds me daily of the purpose of this life and the love the Lord feels for each of His children. I am fortunate to have received love and support from family, both immediate and extended, which helps foster a sense of wholeness in my life. I am uplifted and reinforced by the friends I have made during this season of life, both inside and outside the lab, particularly those whom I have come to know closely on a personal level. I respect, honor, and am indebted to Tim Garrett for providing me the opportunity for this journey. -
Functional Roles of Each of the 400 Putative Gene Products Used for Inferring Bradyrhizobium Phylogeny
Supplementary Table S3: Functional roles of each of the 400 putative gene products used for inferring Bradyrhizobium phylogeny. Kyoto Encyclopedia of Genes and Genomes (KEGG) Amino Gene Gene KEGG Acid number identifiera Orthology KEGG Annotation Functional class Definition model 1 BJ6T_00940 Uncharacterised Unclassified JTT NitT/TauT family transport system Mineral and organic ion transport 2 BJ6T_00960 K02050 permease protein system ABC.SN.P LG NitT/TauT family transport system ATP- Mineral and organic ion transport 3 BJ6T_00970 K02049 binding protein system ABC.SN.A JTT 4 BJ6T_01730 K05524 ferredoxin Energy metabolism fdxA Dayhoff 5 BJ6T_01770 K02902 large subunit ribosomal protein L28 Translation RP-L28 DCMut 6 BJ6T_01900 Uncharacterised Unclassified JTT Metabolism of cofactors and 7 BJ6T_01930 K09882 cobaltochelatase CobS vitamins cobS LG 8 BJ6T_01980 Uncharacterised Unclassified DCMut 9 BJ6T_02010 K01735 3-dehydroquinate synthase Amino acid metabolism aroB JTT Chromosome and associated 10 BJ6T_02040 K04763 integrase/recombinase XerD proteins xerD JTT DNA repair and recombination 11 BJ6T_02180 K03574 8-oxo-dGTP diphosphatase proteins mutT LG 12 BJ6T_02220 K11206 deaminated glutathione amidase Unclassified metabolism NIT1 CpREV 13 BJ6T_02230 Uncharacterised Unclassified JTT 14 BJ6T_02290 K02835 peptide chain release factor 1 Translation factors prfA JTT 15 BJ6T_02440 K00023 acetoacetyl-CoA reductase Carbohydrate metabolism phbB JTT 16 BJ6T_02460 Uncharacterised Unclassified JTT 17 BJ6T_02900 K01087 trehalose 6-phosphate phosphatase -

Bill Ceevee 2014
curriculum vitae, William F. Martin Institutional address: Home address: Institut für Botanik III Rilkestrasse 13 Heinrich Heine-Universität Düsseldorf D-41469 Neuss Universitätsstraße 1 Germany D-40225 Düsseldorf Germany e-mail: [email protected] Tel. +49-211-811-3011 Date of birth : 16.02.57 in Bethesda, Maryland, USA Familial status : Married, four children Nationality : USA University degree : 1981-1985, Technische Universität Hannover, Germany: Biology Diplom thesis : 1985, Institut für Botanik, TU Hannover with Rüdiger Cerff: Botany PhD thesis : 1985-1988, Max-Planck-Institut für Züchtungsforschung, Cologne, with Heinz Saedler; degree conferred by the University of Cologne: Genetics Postdoc : 1988-1989, Max-Planck-Institut für Züchtungsforschung, Cologne Postdoc : 1989-1999, Institut für Genetik, Technische Universität Braunschweig Habilitation : 1992, TU Braunschweig, Germany, venia legendi for the field of Botany Full professor : 1999-2011 for "Ecological Plant Physiology" (C4), Universität Düsseldorf : 2011- for "Molecular Evolution" (C4), Universität Düsseldorf Honours 2013- Visiting Professor, Instituto de Tecnologia Química e Biológica, Oeiras, Portugal 2012 Elected Member of EMBO (European Molecular Biology Organisation) 2010- Science Advisory Committe, Helmholz Alliance Planetry Evoution and Life 2008 Elected Member of the Nordrhein-Westfälische Akademie der Wissenschaften 2007-2012 Selection Committee for the Heinz-Maier-Leibnitz Prize of the DFG 2006 Elected Fellow of the American Academy for Microbiology 2006-2009 Julius von -

A Novel Mouse Model for Inhibition of DOHH-Mediated Hypusine Modification Reveals a Crucial Function in Embryonic Development, P
© 2014. Published by The Company of Biologists Ltd | Disease Models & Mechanisms (2014) 7, 963-976 doi:10.1242/dmm.014449 RESEARCH ARTICLE A novel mouse model for inhibition of DOHH-mediated hypusine modification reveals a crucial function in embryonic development, proliferation and oncogenic transformation Henning Sievert1, Nora Pällmann1,2,*, Katharine K. Miller3,*, Irm Hermans-Borgmeyer3, Simone Venz4, Ataman Sendoel5,6, Michael Preukschas1, Michaela Schweizer3, Steffen Boettcher6, P. Christoph Janiesch3, Thomas Streichert7, Reinhard Walther4, Michael O. Hengartner5, Markus G. Manz6, Tim H. Brümmendorf8, Carsten Bokemeyer1, Melanie Braig1, Joachim Hauber2, Kent E. Duncan3 and Stefan Balabanov1,6,‡ ABSTRACT factor 5A (eIF5A), represents an essential mechanism in the control The central importance of translational control by post-translational of proliferation of eukaryotic cells (Cooper et al., 1982). This modification has spurred major interest in regulatory pathways that modification leads to the activation of eIF5A and is mediated by control translation. One such pathway uniquely adds hypusine to deoxyhypusine synthase (DHS), which catalyses the transfer of a 4- eukaryotic initiation factor 5A (eIF5A), and thereby affects protein aminobutyl moiety of spermidine to the ε-amino group of Lys50 to synthesis and, subsequently, cellular proliferation through an form an intermediate residue, deoxyhypusine (Dhp50) (Park et al., unknown mechanism. Using a novel conditional knockout mouse 1981). Subsequently, deoxyhypusine hydroxylase (DOHH) -

Supplementary Material Toxicological Impacts and Likely Protein Targets Of
Supplementary Material Toxicological impacts and likely protein targets of bisphenol A in Paramecium caudatum Marcus V. X. Senra† & Ana Lúcia Fonseca Instituto de Recursos Naturais, Universidade Federal de Itajubá, 37500-903, Itajubá, Minas Gerais – Brazil †To whom correspondence should be addressed – [email protected]; Orcid - 0000-0002-3866- 8837 Table S1. Annotation data on the P. caudatum 3D modelled proteins and their binding energies to BPA. BINDING ID DESCRIPTION CHROMOSOME NT_START NT_END ENERGIES (kcal/mol) PCAU.43c3d.1.P00010012 Tryptophan synthase beta subunit-like PLP-dependent enzyme scaffold_0001 23197 24853 -7.4 PCAU.43c3d.1.P00010015 Ribosomal protein L32e scaffold_0001 26373 26859 -6.2 PCAU.43c3d.1.P00010044 Catalase, mono-functional, haem-containing scaffold_0001 71821 73367 -6.5 PCAU.43c3d.1.P00010050 Dihydroorotate dehydrogenase, class 1/ 2 scaffold_0001 76614 79650 -6.6 PCAU.43c3d.1.P00010054 Serine/threonine/dual specificity protein kinase, catalytic domain scaffold_0001 83399 84653 -6.7 PCAU.43c3d.1.P00010070 Peptidyl-prolyl cis-trans isomerase, FKBP-type scaffold_0001 104909 105387 -5.9 PCAU.43c3d.1.P00010103 V-ATPase proteolipid subunit C-like domain scaffold_0001 168736 169346 -5.6 PCAU.43c3d.1.P00010112 DNA-directed RNA polymerase, RBP11-like dimerisation domain scaffold_0001 180310 181372 -6.0 PCAU.43c3d.1.P00010165 Vacuolar (H+)-ATPase G subunit scaffold_0001 252653 253112 -5.6 PCAU.43c3d.1.P00010176 Coproporphyrinogen III oxidase, aerobic scaffold_0001 262051 263168 -6.7 PCAU.43c3d.1.P00010205 Metalloenzyme, -

Biosynthesis and Regulation of Polyamines in Higher Plants
Plant Growth Regulation 3:205-226 H985). [3] © 1985 Martinus Ni/hoff/Dr W. Junk Publishers, Dordrecht. Pn'nted in the Netherlands. Biosynthesis and regulation of polyamines in higher plants P.R. ADIGA and G.L. PRASAD Department of Biochemistry, Indian Institute of Science, Bangalore 560 012, India (Received 10 Oct. 1984; accepted 15 Oct. 1984) 1. Introduction The polyamines (PAs), spermidine (SPD) and spermine (SPN) and their diamine precursor, putrescine (PUT) represent a set of evolutionarily highly conserved small molecular weight organic polycations which play vital roles as modulators of a plethora of biological processes from enzyme activation and maintenance of ionic balance, through regulation of growth and development, to mediation of hormone action and progress of cell division cycle. Because of this functional versatility, research on PAs represents one of the most vigorously pursued areas of modern biology. While most of the currently available information on these important classes of bioregulators is derived from microbial and animal systems, interest in their possible participation in various facets of plant biochemistry and physiology is of relatively recent origin. The early pioneering investigations of Smith and others [34, 48, 62, 54, 63] on K+-deficient barley leaves, set the stage for the elucidation of the general metabolic sequences involved in the biogenesis of these amines in plants and pinpointed the important roles PAs play in maintenance of intracellular pH and ionic balance. How- ever, with the recognition that plant systems also offer tremendous potential for unravelling the riddles concerned with the biological functions of PAs, new vistas have been opened in plant PA research.