RESOURCES for OPTIMAL CARE of the INJURED PATIENT 2014 I TABLE of CONTENTS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A BRI H IEF HISTO Howard R. C ORY of TH the Champion, K HE
A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris The Eastern Association for the Surgery of Trauma (EAST) was founded by a group of surgeons each of whom had somewhat established themselves in the field of trauma and surgical critical care by the early 1980s and were in the process of developing these disciplines and mentoring young surgeons. EAST has widely exceeded the original aspirations of that group of then-young surgeons. To understand why EAST was created and why it succeeded, it is necessary to glance back to the mid 1980s. The notion of EAST occurred in 1985 within a context of a growing demand for organized trauma care but no appropriate opportunities for young aspiring trauma surgeons to exchange knowledge, discuss advances in patient care, or develop their careers in this field within the discipline of surgery. No vehicle adequately nurtured young surgeons into the field of trauma. Today, EAST is an established and respected surgical organization reaching its 25-year mark with membership (Figure 1) of 1363 now exceeding that of the premier global trauma organization, the American Association for the Surgery of Trauma (AAST) (1227 members). Then The world of the young trauma surgeon in the early to mid 1980s was a very different place than it is more than 25 years later. -
DACIN SARA Repartitie Aferenta Trimestrului III 2019 Straini TITLU
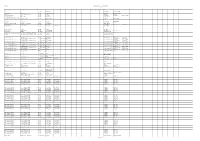
DACIN SARA Repartitie aferenta trimestrului III 2019 Straini TITLU TITLU ORIGINAL AN TARA R1 R2 R3 R4 R5 R6 R7 R8 R9 R10 R11 S1 S2 S3 S4 S5 S6 S7 S8 S9 S10 S11 S12 S13 S14 S15 Greg Pruss - Gregory 13 13 2010 US Gela Babluani Gela Babluani Pruss 1000 post Terra After Earth 2013 US M. Night Shyamalan Gary Whitta M. Night Shyamalan 30 de nopti 30 Days of Night: Dark Days 2010 US Ben Ketai Ben Ketai Steve Niles 300-Eroii de la Termopile 300 2006 US Zack Snyder Kurt Johnstad Zack Snyder Michael B. Gordon 6 moduri de a muri 6 Ways to Die 2015 US Nadeem Soumah Nadeem Soumah 7 prichindei cuceresc Broadway-ul / Sapte The Seven Little Foys 1955 US Melville Shavelson Jack Rose Melville Shavelson prichindei cuceresc Broadway-ul A 25-a ora 25th Hour 2002 US Spike Lee David Benioff Elaine Goldsmith- A doua sansa Second Act 2018 US Peter Segal Justin Zackham Thomas A fost o data in Mexic-Desperado 2 Once Upon a Time in Mexico 2003 US Robert Rodriguez Robert Rodriguez A fost odata Curly Once Upon a Time 1944 US Alexander Hall Lewis Meltzer Oscar Saul Irving Fineman A naibii dragoste Crazy, Stupid, Love. 2011 US Glenn Ficarra John Requa Dan Fogelman Abandon - Puzzle psihologic Abandon 2002 US Stephen Gaghan Stephen Gaghan Acasa la coana mare 2 Big Momma's House 2 2006 US John Whitesell Don Rhymer Actiune de recuperare Extraction 2013 US Tony Giglio Tony Giglio Acum sunt 13 Ocean's Thirteen 2007 US Steven Soderbergh Brian Koppelman David Levien Acvila Legiunii a IX-a The Eagle 2011 GB/US Kevin Macdonald Jeremy Brock - ALCS Les aventures extraordinaires d'Adele Blanc- Adele Blanc Sec - Aventurile extraordinare Luc Besson - Sec - The Extraordinary Adventures of Adele 2010 FR/US Luc Besson - SACD/ALCS ale Adelei SACD/ALCS Blanc - Sec Adevarul despre criza Inside Job 2010 US Charles Ferguson Charles Ferguson Chad Beck Adam Bolt Adevarul gol-golut The Ugly Truth 2009 US Robert Luketic Karen McCullah Kirsten Smith Nicole Eastman Lebt wohl, Genossen - Kollaps (1990-1991) - CZ/DE/FR/HU Andrei Nekrasov - Gyoergy Dalos - VG. -

History of Cardiac Trauma Surgery
History of cardiac trauma surgery A J Nicol, MB ChB, FCS (SA), PhD; P H Navsaria, MB ChB, FCS (SA), MMed (Surg); D Kahn, MB ChB, FCS (SA), ChM Department of Surgery, Groote Schuur Hospital, Cape Town, South Africa Corresponding author: A Nicol ([email protected]) The ancient Egyptians, although realising the diaphragm, of the small intestine, of the coronary artery and that blood in the the anatomical importance of the heart, stomach and of the liver is deadly.’[8,9] Aristotle pericardial sac could compress the heart and were largely responsible for the aura of (384 - 322 BC) wrote that ‘The heart again restrict its movement.[17] mysticism and superstition that enveloped is the only one of the viscera, and indeed the heart for centuries. The Egyptian Book the only part of the body, that is unable to The nihilism surrounding cardiac injuries of the Dead (c. 1567 BC) describes how, on tolerate any serious affection. This is but what continued and in 1804 John Bell published entry to the underworld, the jackal-headed might reasonably be expected. For, if the his Discourses of Nature and Care of Wounds, Anubis weighed the heart of the deceased primary or dominant part be diseased, there declaring that ‘there is so little to be done … against a statue of the goddess of truth and is nothing from which the other parts which and the signs and consequences are so clear, justice.[1,2] If the heart weighed the same, the depend upon it can derive sucour’.[10,11] Celsus that it is a waste of time to speak longer of dead person was admitted ‘to the company (1st century AD) recognised the clinical wounds of the heart’.[5,18] of Osiris and the blessed; if not, if his heart features of shock associated with a cardiac was heavy and laden with sin, it was cast to injury when he wrote in De Medicina that, There is dispute over who should be named the devouring beast Ammit’.[3] ‘When the heart is wounded much blood as the first modern cardiac surgeon. -

Trauma, Surgical Critical Care and Acute Care Surgery Services
Trauma, Surgical Critical Care and Acute Care Surgery Services Region’s most experienced nationally verified Level I trauma center The University of Kansas Hospital is the largest regional resource for trauma and acute care surgery. Our multidisciplinary team provides expert care from the time of injury or illness through the patient’s post-hospitalization rehabilitation. The University of Kansas Hospital focuses this specialty practice on the 3 facets of acute care surgery: emergency surgery, trauma surgery and surgical critical care. Our trauma and acute care specialists are in the hospital 24 hours a day, 7 days a week, providing expert surgical care. We specialize in high-acuity surgical and trauma patients with multisystem injuries and complex surgical conditions. • Because we see a large volume of patients, we excel at providing care to surgical and trauma patients. • Our comprehensive approach to care involves a multidisciplinary team that specifically specializes in caring for acute surgical and trauma patients. • As part of an academic medical center, we are active in surgical research, forging new techniques that lead to improved care and recovery. • We are continually focused on quality improvement for optimal outcomes. PB200320120 Specialized care team Level I trauma care Trauma, critical and acute care Concussion management Trauma and acute care surgery patients The Level I Trauma Center at The University of Our surgeons are board-certified in general Timely and effective concussion treatment receive comprehensive treatment from a Kansas Hospital serves the highest volume of surgery and surgical critical care. They provide is important for recovery. Our concussion multidisciplinary team of professionals, each trauma patients in the region. -

Trauma Surgery (PDF)
Edward Via College of Osteopathic Medicine 4th Year Clinical Rotation: Surgical Critical Care MED 8305: Surgical Selective Clinical Rotation COURSE SYLLABUS Chair Contact Information Michael Breiner, MD Phone: 540-231-0600 Chair of Surgery - VC Email: [email protected] Tom Lindsay, DO Phone: 864-327-9842 Associate Chair of Surgery - CC Email: [email protected] Paul Brisson, MD Phone: 334-442-4023 Chair of Surgery - AC Email: [email protected] I. Rotation Description Students will gain hands-on experience in the diagnosis and management of critically injured and acutely ill general surgery, neurosurgery, and trauma patients. Students function as an integral part of the surgical critical care team. The team is responsible for all aspects of critical care including bedside procedures, ventilatory and post-surgical management. Students will present patients on daily ward rounds and take call. II. Rotation Goals The goal of this rotation is to acquire the knowledge and skills necessary to manage patients with problems unique to the surgical intensive care setting. Additionally, students will appreciate the differences in management strategies between the surgical and medical intensive care units. Bedside teaching and procedure training will occur as part of the daily workrounds. a. Basic knowledge that is needed for the resuscitation, diagnosis and treatment of Surgical Critical Care, including General Surgery, Trauma, and Neurosurgery patients b. Instruction in the basic clinical skills needed to treat Surgical Critical Care, including General Surgery, Trauma, and Neurosurgery patients c. An understanding of the continuum of care involved in the treatment of trauma patients from the resuscitation bay through discharge from the ICU. -

Civilian Killings and Disappearances During Civil War in El Salvador (1980–1992)
DEMOGRAPHIC RESEARCH A peer-reviewed, open-access journal of population sciences DEMOGRAPHIC RESEARCH VOLUME 41, ARTICLE 27, PAGES 781–814 PUBLISHED 1 OCTOBER 2019 http://www.demographic-research.org/Volumes/Vol41/27/ DOI: 10.4054/DemRes.2019.41.27 Research Article Civilian killings and disappearances during civil war in El Salvador (1980–1992) Amelia Hoover Green Patrick Ball c 2019 Amelia Hoover Green & Patrick Ball. This open-access work is published under the terms of the Creative Commons Attribution 3.0 Germany (CC BY 3.0 DE), which permits use, reproduction, and distribution in any medium, provided the original author(s) and source are given credit. See https://creativecommons.org/licenses/by/3.0/de/legalcode Contents 1 Introduction 782 2 Background 783 3 Methods 785 3.1 Methodological overview 785 3.2 Assumptions of the model 786 3.3 Data sources 787 3.4 Matching and merging across datasets 790 3.5 Stratification 792 3.6 Estimation procedure 795 4 Results 799 4.1 Spatial variation 799 4.2 Temporal variation 802 4.3 Global estimates 803 4.3.1 Sums over strata 805 5 Discussion 807 6 Conclusions 808 References 810 Demographic Research: Volume 41, Article 27 Research Article Civilian killings and disappearances during civil war in El Salvador (1980–1992) Amelia Hoover Green1 Patrick Ball2 Abstract BACKGROUND Debate over the civilian toll of El Salvador’s civil war (1980–1992) raged throughout the conflict and its aftermath. Apologists for the Salvadoran regime claimed no more than 20,000 had died, while some activists placed the toll at 100,000 or more. -
World Journal of Critical Care Medicine
World Journal of W J C C M Critical Care Medicine Submit a Manuscript: http://www.wjgnet.com/esps/ World J Crit Care Med 2015 August 4; 4(3): 240-243 Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 2220-3141 (online) DOI: 10.5492/wjccm.v4.i3.240 © 2015 Baishideng Publishing Group Inc. All rights reserved. MINIREVIEWS Intensive care organisation: Should there be a separate intensive care unit for critically injured patients? Tim K Timmers, Michiel HJ Verhofstad, Luke PH Leenen Tim K Timmers, Luke PH Leenen, Department of Surgery, care units with an “open format” setting. However, there University Medical Center Utrecht, 3508 GA Utrecht, The are still questions whether surgical patients benefit from Netherlands a general mixed ICU. Trauma is a significant cause of morbidity and mortality throughout the world. Major or Michiel HJ Verhofstad, Department of Surgery, Erasmus severe trauma requiring immediate surgical intervention Medical Center Rotterdam, 3000 CA Rotterdam, The Netherlands and/or intensive care treatment. The role and type of the ICU has received very little attention in the literature Author contributions: Timmers TK designed the research; Timmers TK and Leenen LPH performed the research; Timmers when analyzing outcomes from critical injuries. Severely TK, Verhofstad MHJ and Leenen LPH wrote the paper. injured patients require the years of experience in complex trauma care that only a surgery/trauma ICU Conflict-of-interest statement: The authors declared that they can provide. Should a trauma center have the capability have no competing interests. of a separate specialized ICU for trauma patients (“closed format”) next to its standard general mixed ICU? Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external Key words: Intensive trauma care; Trauma intensive reviewers. -

Surgical Critical Care Skills
Parkland SICU and Parkland MICU Skills and Assessments The program is designed to give the Fellow in-depth instruction in the many aspects of surgical critical care. The multi-disciplinary nature of the Fellowship with rotations in Burn Surgery, Neurosurgery and Pediatric Surgery allows application of knowledge and skills across multiple disciplines. This is further ensured through the delivery of critical care to a large volume of patients. I. Cardiopulmonary Systems/Monitoring and Medical Instrumentation Knowledge Skills Assessment 1. Understand pathophysiology Insert pulmonary artery, central Faculty observation associated with different causes of venous and arterial lines and obtain during rounds, skills hemodynamic instability. Examples hemodynamic data; interpret data and courses (PA Catheter, include types of shock, cardiac arrest. initiate therapy. Instruct junior ICU Ultrasound) and residents in insertion of invasive resuscitation as monitors and interpretation of data. documented on Resuscitate patients from shock and evaluations. cardiac arrest. 2. Know and apply treatments for Recognize and treat ischemia and Observation during arrhythmias, congestive heart failure, arrhythmia on ECG. Utilize correct rounds, MCCKAP as acute ischemia and pulmonary edema. class of anti-arrhythmic, vasodilators noted on evaluation. and diuretics as they pertain to cardiac disease. Be able to interpret and instruct current ACLS guidelines. 3. Understand factors associated with Ability to assess preoperative risk Observation during assessment of preoperative surgical risk. based on history, physical exam, rounds, MCCKAP as Examples include evaluation of the high laboratory and radiographic data. noted on evaluation. risk cardiac patient undergoing non- Correctly interpret data and optimize cardiac surgery. the high-risk cardiopulmonary patient for surgery. 4.Understand pathophysiology Proficiency and ability to instruct in Direct observation; case associated with respiratory failure. -

The Imaging of Maxillofacial Trauma and Its Pertinence to Surgical Intervention
The Imaging of Maxillofacial Trauma and its Pertinence to Surgical Intervention Nisha Mehta, MDa, Parag Butala, MDb, Mark P. Bernstein, MDa,* KEYWORDS Maxillofacial trauma Surgery Imaging Maxillofacial skeletal injuries account for a large positioning is difficult and potentially dangerous proportion of emergency department visits and for multitrauma patients, in particular patients often result in surgical consultation.1 Although requiring cervical spine clearance. Modern multi- many of the principles of detection and repair are detector CT (MDCT) scanners have revolutionized basic, evolving technology and novel therapeutic trauma imaging and provide a fast, safe, cost- strategies have led to improved patient outcomes. effective, and sensitive means for assessing The goal of imaging studies in the trauma setting is trauma for bone and soft tissue injuries. Further- to define the number and location of facial fractures, more, with the advent of MDCT, facial scans with particular attention toward identifying injuries to can now be performed contemporaneously with functional portions of the face and those with head, thoracic, and abdominal scans, facilitating cosmetic consequence. By understanding common a rapid assessment for trauma patients with fracture patterns and the implications for clinical multiple potential injuries. management, radiologists can better construct clin- MDCT offers excellent spatial resolution, which ically relevant radiology reports and thus facilitate in turn enables exquisite multiplanar reformations, improved communication with referring clinicians. and 3-D reconstructions, allowing enhanced diag- This article aims to provide a review of the imaging nostic accuracy and surgical planning. These aspects involved in maxillofacial trauma and to reconstructions assist in the assessment of frac- delineate its relevance to management. -

Cardiothoracic Trauma
Moheb A. Rashid, M.D. Moheb CARDIOTHORACIC TRAUMA A SCANDINAVIAN PERSPECTIVE Moheb A. Rashid, M.D. CARDIOTHORACIC TRAUMA CARDIOTHORACIC Göteborg, 2007 ISBN: 978-91-628-7171-0 CARDIOTHORACIC TRAUMA A Scandinavian Perspective Moheb A. Rashid, MD Division of Surgery, Institute of Clinical Sciences Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden Göteborg 2007 “..And if any one saved a life it would be as if he/she saved the life of the whole people..” (Quran S. The Table 005:032) “The wards are the greatest of all research laboratories” (Sir Henry Wade, 1877-1955, Surgeon, Royal Infirmary, Edinburgh) The cover depicts the Papyrus of Hunefer from the 19th Dynasty (1307-1196 BC) showing the deceased (Hunefer) led in by Anubis, and his heart weighed against a feather. Anubits checks the balance while the crocodile (eater) stands ready and Toth records the results. It is believed to be the first picture of the heart. Dedicated to: My Parents Om-Hashem & Abdelhay My Sisters & Brothers in Egypt Christina, Magda, Joseph & Jacob CARDIOTHORACIC TRAUMA A Scandinavian Perspective Moheb A. Rashid, MD, Division of Surgery, Institute of Clinical Sciences, Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden. Abstract Background: Trauma in general is a major cause of morbidity and mortality worldwide, and causes more loss of productive years than ischemic heart disease and malignancy together. Cardiothoracic trauma occurs in 60% of multitrauma patients and is 2-3 times more common than intra-abdominal visceral injuries. It constitutes 25% of traumatic deaths and contributes significantly to at least another 25% of these fatalities. Though only about 15% of chest trauma requires operative intervention, a considerable number of preventable deaths occur due to inadequate or delayed treatment of otherwise an easily remediable injury. -

Hippocrates Now
Hippocrates Now 35999.indb 1 11/07/2019 14:48 Bloomsbury Studies in Classical Reception Bloomsbury Studies in Classical Reception presents scholarly monographs offering new and innovative research and debate to students and scholars in the reception of Classical Studies. Each volume will explore the appropriation, reconceptualization and recontextualization of various aspects of the Graeco- Roman world and its culture, looking at the impact of the ancient world on modernity. Research will also cover reception within antiquity, the theory and practice of translation, and reception theory. Also available in the Series: Ancient Magic and the Supernatural in the Modern Visual and Performing Arts, edited by Filippo Carlà & Irene Berti Ancient Greek Myth in World Fiction since 1989, edited by Justine McConnell & Edith Hall Antipodean Antiquities, edited by Marguerite Johnson Classics in Extremis, edited by Edmund Richardson Frankenstein and its Classics, edited by Jesse Weiner, Benjamin Eldon Stevens & Brett M. Rogers Greek and Roman Classics in the British Struggle for Social Reform, edited by Henry Stead & Edith Hall Homer’s Iliad and the Trojan War: Dialogues on Tradition, Jan Haywood & Naoíse Mac Sweeney Imagining Xerxes, Emma Bridges Julius Caesar’s Self-Created Image and Its Dramatic Afterlife, Miryana Dimitrova Once and Future Antiquities in Science Fiction and Fantasy, edited by Brett M. Rogers & Benjamin Eldon Stevens Ovid’s Myth of Pygmalion on Screen, Paula James Reading Poetry, Writing Genre, edited by Silvio Bär & Emily Hauser -

Fostering and Measuring Skills: Improving Cognitive and Non-Cognitive Skills to Promote Lifetime Success
Fostering and Measuring Skills: Improving Cognitive and Non-Cognitive Skills to Promote Lifetime Success Tim Kautz, James J. Heckman, Ron Diris, Bas ter Weel, Lex Borghans Directorate for Education and Skills Centre for Educational Research and Innovation (CERI) Education and Social Progress www.oecd.org/edu/ceri/educationandsocialprogress.htm FOSTERING AND MEASURING SKILLS: IMPROVING COGNITIVE AND NON-COGNITIVE SKILLS TO PROMOTE LIFETIME SUCCESS This work is published under the responsibility of the Secretary-General of the OECD. The opinions expressed and arguments employed herein do not necessarily reflect the official views of OECD member countries. This document and any map included herein are without prejudice to the status of or sovereignty over any territory, to the delimitation of international frontiers and boundaries and to the name of any territory, city or area. Photo credits: © Shutterstock You can copy, download or print OECD content for your own use, and you can include excerpts from OECD publications, databases and multimedia products in your own documents, presentations, blogs, websites and teaching materials, provided that suitable acknowledgment of the source and copyright owner is given. All requests for public or commercial use and translation rights should be submitted to [email protected]. Requests for permission to photocopy portions of this material for public or commercial use shall be addressed directly to the Copyright Clearance Center (CCC) at [email protected] or the Centre français d’exploitation du droit de copie (CFC) at [email protected]. ACKNOWLEDGEMENTS This report was commissioned by the OECD through its project on Education and Social Progress. We thank Linor Kiknadze and Edward Sung for valuable research assistance.