Guidelines for Testing Drugs Under International Control in Hair, Sweat and Oral Fluid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abnormal Hair Follicle Development and Altered Cell Fate of Follicular
ERRATUM Development 137, 1775 (2010) doi:10.1242/dev.053116 Abnormal hair follicle development and altered cell fate of follicular keratinocytes in transgenic mice expressing Np63 Rose-Anne Romano, Kirsten Smalley, Song Liu and Satrajit Sinha There was a technical problem with the ePress version of Development 137, 1431-1439 published on 24 March 2010. A number of Greek symbols were missing from the text and figure headings in the Results section. A replacement ePress article was published on 31 March 2010. The online issue and print copy are correct. We apologise to authors and readers for this error. DEVELOPMENT AND STEM CELLS RESEARCH ARTICLE 1431 Development 137, 1431-1439 (2010) doi:10.1242/dev.045427 © 2010. Published by The Company of Biologists Ltd Abnormal hair follicle development and altered cell fate of follicular keratinocytes in transgenic mice expressing DNp63a Rose-Anne Romano1, Kirsten Smalley1, Song Liu2,3 and Satrajit Sinha1,* SUMMARY The transcription factor p63 plays an essential role in epidermal morphogenesis. Animals lacking p63 fail to form many ectodermal organs, including the skin and hair follicles. Although the indispensable role of p63 in stratified epithelial skin development is well established, relatively little is known about this transcriptional regulator in directing hair follicle morphogenesis. Here, using specific antibodies, we have established the expression pattern of DNp63 in hair follicle development and cycling. DNp63 is expressed in the developing hair placode, whereas in mature hair its expression is restricted to the outer root sheath (ORS), matrix cells and to the stem cells of the hair follicle bulge. To investigate the role of DNp63 in hair follicle morphogenesis and cycling, we have utilized a Tet-inducible mouse model system with targeted expression of this isoform to the ORS of the hair follicle. -

Anatomy and Physiology of Hair
Chapter 2 Provisional chapter Anatomy and Physiology of Hair Anatomy and Physiology of Hair Bilgen Erdoğan ğ AdditionalBilgen Erdo informationan is available at the end of the chapter Additional information is available at the end of the chapter http://dx.doi.org/10.5772/67269 Abstract Hair is one of the characteristic features of mammals and has various functions such as protection against external factors; producing sebum, apocrine sweat and pheromones; impact on social and sexual interactions; thermoregulation and being a resource for stem cells. Hair is a derivative of the epidermis and consists of two distinct parts: the follicle and the hair shaft. The follicle is the essential unit for the generation of hair. The hair shaft consists of a cortex and cuticle cells, and a medulla for some types of hairs. Hair follicle has a continuous growth and rest sequence named hair cycle. The duration of growth and rest cycles is coordinated by many endocrine, vascular and neural stimuli and depends not only on localization of the hair but also on various factors, like age and nutritional habits. Distinctive anatomy and physiology of hair follicle are presented in this chapter. Extensive knowledge on anatomical and physiological aspects of hair can contribute to understand and heal different hair disorders. Keywords: hair, follicle, anatomy, physiology, shaft 1. Introduction The hair follicle is one of the characteristic features of mammals serves as a unique miniorgan (Figure 1). In humans, hair has various functions such as protection against external factors, sebum, apocrine sweat and pheromones production and thermoregulation. The hair also plays important roles for the individual’s social and sexual interaction [1, 2]. -

Medical Review Officer Manual
Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Substance Abuse Prevention Medical Review Officer Manual for Federal Agency Workplace Drug Testing Programs EFFECTIVE OCTOBER 1, 2010 Note: This manual applies to Federal agency drug testing programs that come under Executive Order 12564 dated September 15, 1986, section 503 of Public Law 100-71, 5 U.S.C. section 7301 note dated July 11, 1987, and the Department of Health and Human Services Mandatory Guidelines for Federal Workplace Drug Testing Programs (73 FR 71858) dated November 25, 2008 (effective October 1, 2010). This manual does not apply to specimens submitted for testing under U.S. Department of Transportation (DOT) Procedures for Transportation Workplace Drug and Alcohol Testing Programs (49 CFR Part 40). The current version of this manual and other information including MRO Case Studies are available on the Drug Testing page under Medical Review Officer (MRO) Resources on the SAMHSA website: http://www.workplace.samhsa.gov Previous Versions of this Manual are Obsolete 3 Table of Contents Chapter 1. The Medical Review Officer (MRO)........................................................................... 6 Chapter 2. The Federal Drug Testing Custody and Control Form ................................................ 7 Chapter 3. Urine Drug Testing ...................................................................................................... 9 A. Federal Workplace Drug Testing Overview.................................................................. -
Quantitative Drug Test Menu Section 2
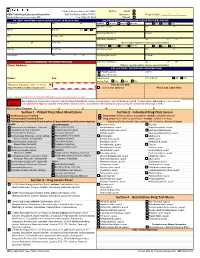
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Substance Abuse in the Workplace Policy
Substance Abuse in the Workplace Policy Rexnord (herein referred to as “Rexnord” or the “Company”) has a strong commitment to its employees to provide a safe work environment and to promote high standards of employee performance. Consistent with the spirit and intent of this commitment, the Company has established a policy regarding substance abuse in the workplace. Further, the Company is committed to maintaining a drug-free workplace as required by “The Drug-Free Workplace Act of 1988.” Therefore, compliance with this Policy is a condition of continued employment with Rexnord. I. PURPOSE To outline the procedures to be followed by each location in order to ensure that the safety and performance of employees is not impaired by alcohol, illegal drugs or other substances. II. APPLICABILITY This policy shall apply to all employees (full-time, part-time, exempt, and non-exempt employees) as well as to all applicants who have received a conditional offer of employment. Personnel who perform their services on Company property or on a third party’s property at the request of the Company (e.g., a Company customer site), as provided under a contract either directly with the Company or through the services of an outside firm, are required to abide by this policy. It is the responsibility of the contracting firm (at its cost and expense) to ensure that its personnel are tested in conformance with this policy prior to working at / on behalf of Rexnord. III. SUBSTANCE ABUSE It is the Company’s policy that the following is prohibited and will result in discipline up to and including termination: A. -

Nestin Expression in Hair Follicle Sheath Progenitor Cells
Nestin expression in hair follicle sheath progenitor cells Lingna Li*, John Mignone†, Meng Yang*, Maja Matic‡, Sheldon Penman§, Grigori Enikolopov†, and Robert M. Hoffman*¶ *AntiCancer, Inc., 7917 Ostrow Street, San Diego, CA 92111; †Cold Spring Harbor Laboratory, 1 Bungtown Road, Cold Spring Harbor, NY 11724; §Department of Biology, Massachusetts Institute of Technology, 77 Massachusetts Avenue, Cambridge, MA 02139-4307; and ‡Stony Brook University, Stony Brook, NY 11794 Contributed by Sheldon Penman, June 25, 2003 The intermediate filament protein, nestin, marks progenitor expression of the neural stem cell protein nestin in hair follicle cells of the CNS. Such CNS stem cells are selectively labeled by stem cells suggests a possible relation. placing GFP under the control of the nestin regulatory se- quences. During early anagen or growth phase of the hair Materials and Methods follicle, nestin-expressing cells, marked by GFP fluorescence in Nestin-GFP Transgenic Mice. Nestin is an intermediate filament nestin-GFP transgenic mice, appear in the permanent upper hair (IF) gene that is a marker for CNS progenitor cells and follicle immediately below the sebaceous glands in the follicle neuroepithelial stem cells (5). Enhanced GFP (EGFP) trans- bulge. This is where stem cells for the hair follicle outer-root genic mice carrying EGFP under the control of the nestin sheath are thought to be located. The relatively small, oval- second-intron enhancer are used for studying and visualizing shaped, nestin-expressing cells in the bulge area surround the the self-renewal and multipotency of CNS stem cells (5–7). hair shaft and are interconnected by short dendrites. The precise Here we report that hair follicle stem cells strongly express locations of the nestin-expressing cells in the hair follicle vary nestin as evidenced by nestin-regulated EGFP expression. -

Long-Lasting Muscle Thinning Induced by Infrared Irradiation Specialized with Wavelengths and Contact Cooling: a Preliminary Report
Long-Lasting Muscle Thinning Induced by Infrared Irradiation Specialized With Wavelengths and Contact Cooling: A Preliminary Report Yohei Tanaka, MD, Kiyoshi Matsuo, MD, PhD, and Shunsuke Yuzuriha, MD, PhD Department of Plastic and Reconstructive Surgery, Shinshu University School of Medicine, Matsumoto, Nagano 390-8621, Japan Correspondence: [email protected] Published May 28, 2010 Objective: Infrared (IR) irradiation specialized with wavelengths and contact cooling increases the amount of water in the dermis to protect the subcutaneous tissues against IR damage; thus, it is applied to smooth forehead wrinkles. However, this treatment consistently induces brow ptosis. Therefore, we investigated whether IR irradiation induces muscle thinning. Methods: Rat central back tissues were irradiated with the specialized IR device. Histological evaluation was performed on sagittal slices that included skin, panniculus carnosus, and deep muscles. Results: Significant reductions in panniculus carnosus thickness were observed between controls and irradiated tissues at postirradiation day 30 (P30), P60, P90, and P180; however, no reduction was observed in nonirradiated controls from days 0 to 180. No significant changes were observed in the trunk muscle over time. From day 0, dermal thickness was significantly reduced at P90 and P180; however, no difference was observed between P180 and nonirradiated controls at day 180. DNA degradation consistent with apoptosis was detected in the panniculus carnosus at P7 and P30. Conclusions: We found that IR irradiation induced long-lasting superficial muscle thinning, probably by a kind of apoptosis. The panniculus carnosus is equivalent to the superficial facial muscles of humans; thus, the changes observed here reflected those in the frontalis muscle that resulted in brow ptosis. -
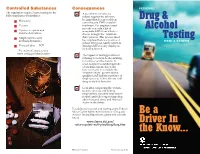
Drug & Alcohol Testing Be a Driver in the Know
Controlled Substances Consequences FEDERAL The regulations require 5-panel testing for the 3 A positive test result or a following classes of substances: refusal requires the driver to be immediately removed from Drug & Marijuana n operating any CMV on public n Cocaine roadways. The employer must provide you with a list of Alcohol n Opiates — opium and acceptable SAPs from which to codeine derivatives choose to begin the “return-to- ” n Amphetamines and duty process. This process must Testing meth amphetamines be completed before a positive or REGULATIONS refusal driver can legally return to n Phencyclidine — PCP driving CMVs for any employer, including himself. For more information, visit www.usdoj.gov/dea/concern 3 The impact of testing positive or refusing to test can be devastating for a driver and his family. It often results in extended periods of unemployment, due to the time necessary to complete the “return-to-duty” process with a qualified SAP and the tendency of employers not to hire drivers with drug or alcohol histories. 3 Even after completing the “return- to-duty” process and finding employment, the additional return- to-duty and follow-up testing often adds increased stress and financial strain on the driver. For additional research and reading on the Federal Motor Carrier Safety Administration’s Drug and Be a Alcohol Testing Regulations, please visit our web site at: www.fmcsa.dot.gov/ Driver In rules-regulations/topics/drug/drug.htm the Know... FMCSA-E-06-003 Revised July 2010 The U.S. Department of Transportation (DOT) whenever they are involved in a fatal accident, or professional (SAP) drug and alcohol testing regulations for receive a traffic citation resulting from an injury or who signs the return- commercial driver licensed (CDL) employees are vehicle-disabling accident. -

Identification of Hair Shaft Progenitors That Create a Niche for Hair Pigmentation
Downloaded from genesdev.cshlp.org on September 27, 2021 - Published by Cold Spring Harbor Laboratory Press Identification of hair shaft progenitors that create a niche for hair pigmentation Chung-Ping Liao,1 Reid C. Booker,1 Sean J. Morrison,2,3,4,5,6 and Lu Q. Le1,4,5 1Department of Dermatology, 2Department of Pediatrics, 3Children’s Research Institute, 4Simmons Comprehensive Cancer Center, 5Hamon Center for Regenerative Science and Medicine, 6Howard Hughes Medical Institute, University of Texas Southwestern Medical Center, Dallas, Texas 75390, USA Hair differentiates from follicle stem cells through progenitor cells in the matrix. In contrast to stem cells in the bulge, the identities of the progenitors and the mechanisms by which they regulate hair shaft components are poorly understood. Hair is also pigmented by melanocytes in the follicle. However, the niche that regulates follicular melanocytes is not well characterized. Here, we report the identification of hair shaft progenitors in the matrix that are differentiated from follicular epithelial cells expressing transcription factor KROX20. Depletion of Krox20 lin- eage cells results in arrest of hair growth, confirming the critical role of KROX20+ cells as antecedents of structural cells found in hair. Expression of stem cell factor (SCF) by these cells is necessary for the maintenance of differen- tiated melanocytes and for hair pigmentation. Our findings reveal the identities of hair matrix progenitors that regulate hair growth and pigmentation, partly by creating an SCF-dependent niche for follicular melanocytes. [Keywords: stem cell factor (SCF); hair pigmentation; hair shaft progenitor cell; hair follicle stem cell; hair matrix; KROX20] Supplemental material is available for this article. -

Considerations for the Use of Saliva As Sample Material for COVID-19 Testing 3 May 2021
[Type here] ECDC TECHNICAL REPORT Considerations for the use of saliva as sample material for COVID-19 testing 3 May 2021 Key messages • Nasopharyngeal specimens remain the gold standard for COVID-19 testing for use with RT-PCR and rapid antigen diagnostic tests. • Studies on the performance of RT-PCR tests have variously reported both higher and lower sensitivity for saliva samples compared with nasopharyngeal swabs. However, meta-analyses of such studies suggest an overall similar or non-statistically significant lower sensitivity associated with the use of saliva samples. • The reported heterogeneity is likely to, in part, reflect differences in sampling techniques, sampling times and the type of population being tested, with evidence that RT-PCR tests with saliva as sample material show similar sensitivity to those using nasopharyngeal swabs for symptomatic patients, if the sample collection is performed within the first five days from onset of symptoms, and when the viral load is high. • Saliva sample collection is easy, non-invasive, more acceptable for repeat testing and can be performed by non-healthcare professionals or individuals themselves who are properly instructed. • Evidence supports the conclusion that saliva can be used as an alternative sample material for RT- PCR testing when nasopharyngeal swabs cannot be collected in the following scenarios: in symptomatic patients and for repeated screening of asymptomatic individuals. • Further clinical studies are warranted on the sensitivity of saliva as sample material for RT-PCR analysis for symptomatic and asymptomatic children, and to standardise the sampling collection methods. • Current limited evidence does not support the use of saliva as an alternative sample material for rapid antigen or antibody tests. -

Hormone Testing
Hormone Testing Saliva Testing The Nutrition and Health Center utilizes the leading salivary-based testing and research laboratory in the United States to measure hormones. This method is called Enzyme Linked Immunosorbent Assay; it measures “free fraction hormone levels,” giving more information than measuring “bound hormone levels.” The commonly used blood and serum hormone tests look only at the level of hormones that are present in a person’s tissues; this is known as “bound hormone levels.” Saliva testing has many advantages over blood testing including: • Saliva specimen collection does not require a blood draw and there are no risks to you • Saliva collections are convenient and can be done at work or at home • When stored properly, saliva samples are stable for several weeks • With an accuracy of 92-96%, saliva testing is more accurate than blood testing • The ability to collect more than one specimen which provides more information than a single collection • Compared to blood testing, saliva testing is also more affordable • Saliva testing looks at the “unbound hormone levels” also known as “free fraction hormone levels” which are the hormone levels that are available to be used by the body’s tissues. This gives a better idea of the levels of hormones that are actually influencing the tissues, rather than just the level of hormones that are present in the tissues Types of Saliva Tests There are various hormones in your body, so there are various corresponding saliva tests that can be administered. The tests that we use are the Female Hormone Panel™ (FHP™) test, Adrenal Stress Index™ (ASI), and the Flexi-Matrix Customized panel. -

Ncaa Drug Policies
MEDICAL EXCEPTIONS APPEALS The NCAA recognizes that some banned substances The NCAA drug-testing program allows an are used for legitimate medical purposes. According- institution to appeal a positive drug test on behalf ly, the NCAA allows exception to be made for those of a student-athlete who has tested positive or who student-athletes with a documented medical history violated NCAA drug-testing protocol. demonstrating the need for regular use of such a drug. Exceptions may be granted for substances • The institution must submit in writing the included in the following classes of banned drugs: grounds for the appeal and a summary of the stimulants (including those used to treat ADHD), institutional drug-education program. beta blockers, beta-2 agonists, diuretics, peptide • At least three members of the drug- hormones, anabolic agents and anti-estrogens. education and drug-testing subcommittee of the • Pre-approval is required for the use of peptide NCAA Committee on Competitive hormones or anabolic agents. The institution Safeguards and Medical Aspects of Sports must submit required documents to the NCAA (CSMAS) hear appeals. ([email protected]) prior to the student-athlete competing while using medications containing • Appeals are conducted by telephone these substances. conference. • For all other drug classes, the institution should • The director of athletics or designee and the maintain documents from the prescribing student-athlete must be on the appeal call. physician in the student-athlete’s medical record on campus that include the diagnosis, course of • The NCAA does not restrict the nature of the treatment and current prescription. appeal, that is to say that the NCAA will not restrict access for any reason to an institution that wishes • In the event that a student-athlete tests positive to appeal and has satisfied the appeal procedures.