Hydroxocobalamin Hydrochloride: Summary Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IV-23 N. Hydroxocobalamin (Cyanokit®)
N. Hydroxocobalamin (Cyanokit®) I. Classification •Cyanide antidote II. Actions •Binds cyanide ions with more affinity than hemoglobin molecule •Cyanide ion and hydroxocobalamin form cyanocobalamin (Vitamin B12) which is then excreted in the urine. III. Indications •Known or suspected cyanide poisoning - patients at high risk (industrial accidents, fire victims with smoke inhalation, known overdose, etc) with one more more of the following symptoms: - Altered mental status, confusion, seizures, coma - Headache - Chest pain or tightness - Shortness of breath, bradypnea, tachypnea - Hypertension (early), hypotension (late), cardiovascular collapse - Nausea, vomiting - Cardiac arrest - Mydriasis (dilated pupils) IV. Contraindications •Known allergic reaction to hydroxocobalamin or cyanocobalamin V. Adverse effects A. Cardiovascular •Ventricular extrasystoles •Tachycardia •Transient hypertension B. Neurological •Memory impairment •Dizziness •Restlessness C. Respiratory •Dyspnea •Dry Throat •Throat tightness D. Gastrointestinal •Abdominal discomfort •Dysphagia •Vomiting, diarrhea •Hematochezia E. General •Allergic reaction, pruritis, anaphylaxis •Hot flush SUBJECT : PATIENT CARE GUIDELINES AND STANDING ORDERS FOR BLS AND ALS UNITS REFERENCE NO. III-01 PUBLICATION : 1/11/21 IV-23 VI. Administration A. Do not administer hydroxocobalamin through the same IV site/set as the following medications: dopamine, fentanyl, dobutamine, diazepam, nitroglycerin, pentobarbital, propofol, thiopental, sodium thiosulfate, sodium nitrite and ascorbic acid. You must start a second IV to administer hydroxocobalamin in patient’s receiving these medications. B. Adult: •5 grams IV/IO over 15 minutes (Stocked as single 5gm bottle, or two 2.5 gm bottles) -Single 5 gm Bottle - Reconstituted with 200 ml Normal Saline. -Two 2.5 gm Bottles, give over 7.5 minutes each. - Each vial reconstituted with 100 ml Normal Saline. C. Pediatric •100 mg/kg IV/IO of hydroxocobalamin (reconstituted with Normal Saline the same as adults) over 15 minutes. -

University of Colorado Denver Anschutz Medical Campus Msa Capstone Presenations
UNIVERSITY OF COLORADO DENVER ANSCHUTZ MEDICAL CAMPUS ANNUAL STUDENT MSA CAPSTONE PRESENTATIONS MARCH 2, 2017 ANSCHUTZ MEDICAL CAMPUS HEALTH AND SCIENCES LIBRARY UNIVERSITY OF COLORADO DENVER ANSCHUTZ MEDICAL CAMPUS MSA CAPSTONE PRESENATIONS Thursday, March 2, 2017 Poster Sessions Session A: 1:00 pm – 2:00 pm Session B: 2:15 pm – 3:15 pm Session C: 3:30 pm – 4:30 pm ANSCHUTZ MEDICAL CAMPUS Health Sciences Library The MSA Directors to acknowledge, with gratitude, the support for medical student research provided by: The University of Colorado Denver School of Medicine Dean’s Office And Undergraduate Medical Education Office Poster Session Judges The organizing committee wishes to acknowledge their appreciation to the following serving as judges for the MSA Capstone Presentations. Without their generous contribution of time and talent the forum would not be possible. Thank you! Madiha Abdel-Maksoud, MP, MSPH, PhD Rooban Nahomi, PhD David Ammar, PhD Matthew Nalty, BA Ilango Balakrishnan, PhD Kristen Nowak, PhD, MPH Carl Barnes, MD David Orlicky, Ph.D. Adria Boucharel, MD David Orlicky, Ph.D. Joseph Brzezinski, PhD Clare Paterson, PhD William Cornwell. MD Karin Payne, PhD Colleen Dingmann, R.N, Ph.D. Mark Petrash, PhD Michele Doucette, Ph.D. Miriam Post, MD Charles Edelstein, MD, PhD Allan Prochazka, MD, MSc Adit Ginde, MD, MPH Laura Pyle, PhD Jackie Glover, Ph.D Cordelia Robinson Rosenberg, PhD, RN Daniel Goldberg, JD, PhD Joseph Sakai, MD Maryam Guiahi, MD, MSc David Schwartz, MD Pearce Korb, MD Robert Sclafani, PhD Luidmila Kulik, PhD Deb Seymour, PsyD Rita Lee, MD Nicole Tartaglia, MS, MD Steven Lowenstein, MD, MPH Jean Tsai, MD, PhD Wendy Macklin, PhD Catherine Velopulos, MD, MHS Sandy Martin, PhD Laura Wiley, PhD Leana May DO, MPH Seonghwan Yee, PhD Jose Mayordomo, Ph.D. -

Cyanocobalamin-A Case for Withdrawal
686 Journal of the Royal Society of Medicine Volume 85 November 1992 Cyanocobalamin- a case for withdrawal: discussion paper A G Freeman MD FRCP Meadow Rise, 3 Lakeside, Swindon SN3 IQE Keywords: anaemia, pernicious; optic neuropathies; chronic cyanide intoxication; hydroxocobalamin; cyanocobalamin It seems evident that controversy still surrounds the reduced ability to detoxify the cyanide in the tobacco- treatment of pernicious anaemia and other vitamin smoke to which they are exposed'0. B12 deficiency disorders. The long quest for the 'anti- Patients with tobacco amblyopia who have normal pernicious anaemia factor' in the liver seemed to serum vitamin B12 levels need not continue therapy have ended in 1948 when pure cyanocobalamin was with intramuscular hydroxocobalamin once their isolated. This was found to be very active thera- visual acuity and visual fields have returned to peutically when given by intramuscular injection and normal providing they abstain from further smoking. was non-toxic in extremely high doses'. However, those patients who have low serum vitamin Lederle, in a recent commentary2, advocates that B12 levels or evidence of -defective vitamin B12 patients with pernicious anaemia should now be absorption will need to continue-indefinitely with treated with oral cyanocobalamin. He is not without hydroxocobalamin irrespective of their smoking support in that 40% of patients with pernicious habits as will all patients with pernicious anaemia anaemia in Sweden are being similarly treated3. and other vitamin B12 deficiency disorders who are He further states that such!- treatment is cheap at risk of developing- optic neuropathy if they and effective, produces clinical and haematological are smokers. -

Hydroxocobalamin for Injection) for Intravenous Infusion Alternative Therapies, If Available, in Patients with Known Anaphylactic Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------CONTRAINDICATIONS----------------------------- These highlights do not include all the information needed to use None (4) CYANOKIT safely and effectively. See full prescribing information for CYANOKIT. ------------------------WARNINGS AND PRECAUTIONS----------------------- Risk of Anaphylaxis and Other Hypersensitivity Reactions: Consider CYANOKIT® (hydroxocobalamin for injection) for intravenous infusion alternative therapies, if available, in patients with known anaphylactic Initial U.S. Approval: 1975 reactions to hydroxocobalamin or cyanocobalamin. (5.2) Risk of Renal Injury: Acute renal failure with acute tubular necrosis, renal ----------------------------RECENT MAJOR CHANGES-------------------------- impairment and urine calcium oxalate crystals have been reported Warnings and Precautions, Risk of Renal Injury (5.3) 12/2018 following CYANOKIT therapy. Monitor renal function for 7 days Warnings and Precautions, Use of Blood Cyanide Assay (5.7) 12/2018 following CYANOKIT therapy. (5.3) Risk of Increased Blood Pressure: Substantial increases in blood pressure ----------------------------INDICATIONS AND USAGE--------------------------- may occur following CYANOKIT therapy. Monitor blood pressure during CYANOKIT is indicated for the treatment of known or suspected cyanide treatment. (5.4) poisoning. (1) -------------------------------ADVERSE REACTIONS------------------------------ ------------------------DOSAGE AND ADMINISTRATION---------------------- Most common -

Vasoplegic Syndrome After Pediatric Cardiac Surgery
Journal of Anesthesia & Critical Care: Open Access Review Article Open Access Vasoplegic syndrome after pediatric cardiac surgery Abstract Volume 12 Issue 3 - 2020 Vasoplegic syndrome (VS) is a form of vasodilatory shock that occurs in the early period in Pınar Yıldırım Özkan,1 Ahmet Akyol,1 pek patients who undergo cardiac surgery requiring cardiopulmonary bypass (CBP). Vasoplegic 2 1 1 syndrome, reported between 9 and 44%, is characterized by severe hypotension,severe Erus, AhuBaysal Çitil, Ayşe Duygu Kavas, 3 decrease in systemic vascular resistance, decreased arteriolar reactivity, need for increased Ahmet Ero lu İ 1 volume, and decreased response to norepinephrine, despite normal ardiac outflow. The University of Health Sciences, Ümraniye Training and Vasoplegia is associated with high mortality and morbidity, especially in pediatric patients. Research Hospital,ğ Clinic of Anesthesiology and Intensive Care, The pathophysiology of vasoplegic syndrome includes disruption of the arteriolar tone, Turkey 2Koc University, Medical Faculty, Clinic of Anesthesiology and which is regulated by endothelial function and neurohumoral system.Methylene blue is Intensive Care, Turkey safely used when administered at a dose below 2mg/kg while more prospective randomized 3KTU, Medical Faculty, Clinic of Anesthesiology and Intensive controlled trials are needed to determine the effective dose range. Care, Turkey Keywords: vasoplegic syndrome, pediatric, cardiac surgery, methylene blue, Correspondence: Assoc. Prof.Dr.Ahmet AKYOL, The cardiyopulmoner bypass, prostaglandin infusion, pleth variability index, cross clamp University of Health Sciences, Ümraniye Training and Research Hospital, Clinic of Anesthesiology and Intensive Care, ElmalikentMah. AdemYavuz Cad. No: 1. (34764) Ümraniye, stanbul, Turkey, Tel +90 533 6331369, Email İ Received: April 29, 2020 | Published: May 21, 2020 Introduction min), SpO2 was 85%, BP 69/37 mmHg, and pulse 168/min at room temperature. -

Adult BLS Standing Orders • Ensure EMS Provider Safety, Consider HAZMAT Activation
Imperial County Public Health Department Emergency Medical Services Agency Policy/Procedure/Protocol Manual Treatment Protocols Date: 07/01/2021 Poisoning/Intoxication/Envenomation - Adult Policy #9160A Adult BLS Standing Orders • Ensure EMS provider safety, consider HAZMAT activation. Recognize, Notify, Isolate • Universal Patient Protocol • Do not approach patient or location if scene safety is in question • Obtain accurate history of incident: o Name of product or substance o Quantity ingested, and/or duration of exposure o Time elapsed since exposure o If safe and accessible, bring medications or bottles to hospital • Move victim(s) to safe environment • Externally decontaminate - PRN • Continuously monitor ECG, blood pressure, pulse oximetry, and capnography (if ALS present) PRN • Give oxygen and provide airway support per Airway Policy • Contact Poison Control Center as needed 1 (800) 222-1222 Suspected Opioid Overdose with Respirations <12 RPM • If possible, avoid the use of a supraglottic device prior to the administration of naloxone • Administer naloxone 0.1 mg/kg, max of 2 mg IN. May repeat up to three (3) times, q5min • May assist family/friends on-scene with administration of patient’s own naloxone • NOTE - Use with caution in opioid dependent pain management patients • Assess vitals, with specific attention to respiratory rate and respiratory drive • Note pupil exam • Note drug paraphernalia or medication bottles near patient Suspected Stimulant Overdose with Sudden Hypoventilation, Oxygen Desaturation, or Apnea • High flow -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

When Fluids Are Not Enough: Inopressor Therapy Problems in Neonatology
When Fluids are Not Enough: Inopressor Therapy Problems in Neonatology • Neonatal problem: hypoperfusion Severe sepsis Hallmark of septic shock Secondary to neonatal encephalopathy Vasoplegia Syndrome?? • First line therapy Fluid loading – 20 ml/kg boluses • Inopressor therapy Inotropic therapy Pressor therapy Treating Hypoperfusion • GOAL: return of perfusion Not to achieve a given set of blood pressure values • Measure of perfusion Flow is proportional to left ventricular output Flow is inversely proportional to vascular resistance BP is a measure of these • But… High blood pressure ≠ flow Low blood pressure ≠ no flow BP and Capillary Perfusion Clinical Experience • BP does not correlate with microcirculatory flow • Increasing BP with noradrenaline Unpredictable effects on capillary perfusion • Normalizing BP with pure vasoconstrictor Phenylephrine Decrease microcirculatory perfusion • Impaired cardiac function Vasopressor increases afterload Reduce cardiac output with increase BP No benefit global perfusion Perfusion Physiology • Normal foal BP ≠ perfusion (tissue blood flow) • Microcirculation controlled by metabolic demand + • ADP, K, H or NO (shear stress), O2 levels • When decrease BP Sympathetic control • Overrides tissue-driven blood flow regulation • Baroreceptors response Peripheral vasoconstriction to preserve • Preserve heart and brain perfusion • At expense of global tissue hypoperfusion • Shock Hydrostatic Pressure A = arteriolar constriction B = arteriolar dilation Dünser et al. Critical Care 2013, 17:326 Permissive Hypotension -
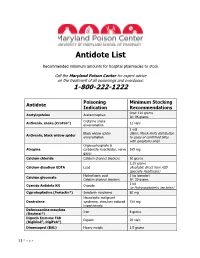
Antidote List
Antidote List Recommended minimum amounts for hospital pharmacies to stock Call the Maryland Poison Center for expert advice on the treatment of all poisonings and overdoses: 1-800-222-1222 Poisoning Minimum Stocking Antidote Indication Recommendations Oral: 120 grams Acetylcysteine Acetaminophen IV: 96 grams Crotaline snake Antivenin, snake (CroFab®) 12 vials envenomation 1 vial Black widow spider (Note: Merck limits distribution Antivenin, black widow spider envenomation to cases of confirmed bites with symptoms only) Organophosphate & Atropine carbamate insecticides, nerve 165 mg gases Calcium chloride Calcium channel blockers 10 grams 2.25 grams Calcium disodium EDTA Lead (Available direct from ASD Specialty Healthcare) Hydrofluoric acid 1 kg (powder) Calcium gluconate Calcium channel blockers IV: 30 grams 1 kit Cyanide Antidote Kit Cyanide (or Hydroxocobalamin, see below) Cyproheptadine (Periactin®) Serotonin syndrome 80 mg Neuroleptic malignant Dantrolene syndrome, stimulant-induced 720 mg hyperthermia Deferoxamine mesylate Iron 8 grams (Desferal®) Digoxin Immune FAB Digoxin 20 vials (Digibind®, DigiFab®) Dimercaprol (BAL) Heavy metals 1.5 grams 1 | P a g e Maryland Poison Center Antidote List – continued Poisoning Minimum Stocking Antidote Indication Recommendations DMSA (Succimer, Chemet®) Heavy metals 2000 mg Folic acid Methanol IV: 150 mg Flumazenil (Romazicon®) Benzodiazepines 10 mg Fomepizole (Antizol®) Ethylene glycol, methanol 12 grams Beta blockers, Glucagon 50 mg calcium channel blockers Hydroxocobalamin (Cyanokit®) Cyanide -

Cyanocobalamin Decision Document
Cyanocobalamin Decision Document Drug Cyanocobalamin (Vitamin B12) Brands Cyanocobalamin (all preparations including Cytacon tablets, Cytamen Injection) Decision West Essex CCG does not commission cyanocobalamin. Date 29th August 2019 Evidence Vitamins were included in the NHS England - Conditions for which over the counter items should not routinely be prescribed in primary care: Guidance for CCGs (29 March 2018) Vitamins and minerals should not be routinely prescribed in primary care due to limited evidence of clinical effectiveness. Exceptions: Medically diagnosed deficiency, including for those patients who may have a lifelong or chronic condition or have undergone surgery that results in malabsorption. Continuing need should however be reviewed on a regular basis. NB maintenance or preventative treatment is not an exception. Calcium and vitamin D for osteoporosis. Malnutrition including alcoholism (see NICE guidance) Patients suitable to receive Healthy start vitamins for pregnancy or children between the ages 6 months to their fourth birthday. (NB this is not on prescription but commissioned separately) British National Formulary Anaemia, megalobastic – overview Most megaloblastic anaemias result from a lack of either vitamin B12 or folate, and it is essential to establish in every case which deficiency is present and the underlying cause. In emergencies, when delay might be dangerous, it is sometimes necessary to administer both substances after the bone marrow test while plasma assay results are awaited. Normally, however, appropriate treatment should not be instituted until the results of tests are available. One cause of megaloblastic anaemia in the UK is pernicious anaemia in which lack of gastric intrinsic factor resulting from an autoimmune gastritis causes malabsorption of vitamin B12. -

2021 ACMT Annual Scientific Meeting Abstracts—Virtual
Journal of Medical Toxicology https://doi.org/10.1007/s13181-021-00832-9 ANNUAL MEETING ABSTRACTS 2021 ACMT Annual Scientific Meeting Abstracts—Virtual Abstract: These are the abstracts of the 2021 American College of 001. Gender-Based Production of N-Acetyl-P-Benzoquinone Imine Medical Toxicology (ACMT) Annual Scientific Meeting. Included here Protein Adduct Formation With Therapeutic Acetaminophen are 178 abstracts that will be presented in April 2021, including research Administration studies from around the globe and the ToxIC collaboration, clinically significant case reports describing toxicologic phenomena, and encore Brandon J Sonn1, Kennon J Heard1,2, Susan M Heard2,Angelo research presentations from other scientific meetings. D'Alessandro1, Kate M Reynolds2, Richard C Dart2, Barry H Rumack1,2,AndrewAMonte1,2 Keywords: Abstracts - Annual Scientific Meeting - Toxicology 1University of Colorado Denver, Aurora, Colorado, USA. 2Rocky Investigators Consortium - Medical Toxicology Foundation Mountain Poison and Drug Center, Denver, Colorado, USA Correspondence: American College of Medical Toxicology (ACMT) Background: Acetaminophen (APAP)-associated transaminase elevation, 10645 N. Tatum Blvd Phoenix, AZ; [email protected] induced by N-acetyl-p-benzoquinone imine (NAPQI) protein adduction, re- mains a global concern. Distinct from known genetic, physiologic, and dos- Introduction: The American College of Medical Toxicology (ACMT) age associations dictating severity of hepatic injury, no known factors predict received 188 eligible research abstracts for consideration for presentation an absence of NAPQI protein adduct formation at therapeutic APAP dosing. at the 2021 Annual Scientific Meeting (ASM), including 85 research Hypothesis: Gender-based physiologies are predictive of APAP-induced studies and 103 case reports. Each abstract was reviewed in a blinded protein adduct formation at therapeutic doses. -

High-Dose Intravenous Hydroxocobalamin for Persistent Vasoplegic Syndrome After Cardiac Surgery Mohamed Ben-Omran, MD1*, Ellen Huang, Pharmd2, Vijay S
ISSN: 2378-3656 Ben-Omran et al. Clin Med Rev Case Rep 2021, 8:335 DOI: 10.23937/2378-3656/1410335 Volume 8 | Issue 1 Clinical Medical Reviews Open Access and Case Reports CASE REPORT High-Dose Intravenous Hydroxocobalamin for Persistent Vasoplegic Syndrome after Cardiac Surgery Mohamed Ben-Omran, MD1*, Ellen Huang, PharmD2, Vijay S. Patel, MD3, Nadine Odo, BA, CCRC4, Taylor Glenn MD5 and Vaibhav Bora, MD6 1Assistant Professor, Anesthesiology and Perioperative Medicine, Augusta University, USA 2Pharmacist, Department of Pharmacy, Augusta University, USA 3 Associate Professor, Cardiothoracic Surgery, Augusta University, USA Check for updates 4Research Associate, Anesthesiology and Perioperative Medicine, Augusta University, USA 5Anesthesiology Resident, Intermountain Healthcare, Murray, Utah, USA 6Assistant Professor, Cleveland Medical Center, Case Western Reserve University, USA *Corresponding author: Mohamed Ben-Omran, MD, Assistant Professor of Anesthesiology and Critical Care Medicine, Department of Anesthesiology and Perioperative Medicine, Augusta University, 1120 15th St. BI-2144, Augusta, GA, 30912, USA, Tel: 6179538493; 7067210091, Fax: 706-721-7763 Abstract Glossary of Terms Vasoplegic syndrome is a vasodilatory shock characterized ACEI: Angiotensin-Converting Enzyme Inhibitors; ARB: by significant hypotension, normal or high cardiac output, Angiotensin II Receptor Blocker; CI: Cardiac Index; ICU: and increased requirement for intravenous fluid resusci- Intensive Care Unit; IL: Interleukin; LAD: Left Anterior De- tation and vasopressors. It is a relatively common compli- scending Coronary Artery; MAP: Mean Arterial Pressure; cation following cardiac surgery. We describe the case of NO: Nitric Oxide; SVG: Saphenous Vein Graft; SVR: Sys- a 77-year-old man who developed prolonged vasoplegic temic Vascular Resistance syndrome which was refractory to high doses of conven- tional vasopressors following coronary artery bypass graft surgery.