Nedd4 Binding Protein 1 (N4BP1) and TNFAIP3 Interacting Protein 1 (TNIP1) Control MHC-1 Display in Neuroblastoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Acute Lymphoblastic Leukemia Patient with Variant ATF7IP
ISSN 1941-5923 © Am J Case Rep, 2017; 18: 1204-1208 DOI: 10.12659/AJCR.906300 Received: 2017.07.20 Accepted: 2017.08.07 Acute Lymphoblastic Leukemia Patient with Published: 2017.11.14 Variant ATF7IP/PDGFRB Fusion and Favorable Response to Tyrosine Kinase Inhibitor Treatment: A Case Report Authors’ Contribution: BCDF 1,2 Ge Zhang* 1 Department of Pediatrics, Key Laboratory of Birth Defects and Related Diseases Study Design A BCD 1 Yanle Zhang* of Women and Children, Ministry of Health, West China Second University Data Collection B Hospital, Sichuan University, Chengdu, Sichuan, P.R. China Statistical Analysis C BD 1 Jianrong Wu 2 Department of Laboratory Medicine, West China Second University Hospital, Data Interpretation D AE 3 Yan Chen Sichuan University, Chengdu, Sichuan, P.R. China Manuscript Preparation E AE 1 Zhigui Ma 3 Department of Pediatrics, Affiliated Hospital of Zunyi Medical College, Zunyi, Literature Search F Guizhou, P.R. China Funds Collection G * Ge Zhang and Yanle Zhang contributed equally to this work Corresponding Authors: Zhigui Ma, e-mail: [email protected]; Yan Chen, e-mail: [email protected] Conflict of interest: None declared Patient: Female, 14-month-old Final Diagnosis: Acute lymphoblastic leukemia Symptoms: Fever Medication: — Clinical Procedure: — Specialty: Hematology Objective: Rare disease Background: Chromosomal translocations involving the PDGFRB gene have been reported in a broad spectrum of hemato- logical malignancies. An ATF7IP/PDGFRB fusion was recently identified in a Philadelphia chromosome-like (Ph- like) B-progenitor acute lymphoblastic leukemia (B-ALL) patient. Here we report on a special case of a Ph-like ALL patient who had a variant ATF7IP/PDGFRB fusion. -

Laboratory Mouse Models for the Human Genome-Wide Associations
Laboratory Mouse Models for the Human Genome-Wide Associations The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Kitsios, Georgios D., Navdeep Tangri, Peter J. Castaldi, and John P. A. Ioannidis. 2010. Laboratory mouse models for the human genome-wide associations. PLoS ONE 5(11): e13782. Published Version doi:10.1371/journal.pone.0013782 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:8592157 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Laboratory Mouse Models for the Human Genome-Wide Associations Georgios D. Kitsios1,4, Navdeep Tangri1,6, Peter J. Castaldi1,2,4,5, John P. A. Ioannidis1,2,3,4,5,7,8* 1 Institute for Clinical Research and Health Policy Studies, Tufts Medical Center, Boston, Massachusetts, United States of America, 2 Tufts University School of Medicine, Boston, Massachusetts, United States of America, 3 Department of Hygiene and Epidemiology, University of Ioannina School of Medicine and Biomedical Research Institute, Foundation for Research and Technology-Hellas, Ioannina, Greece, 4 Tufts Clinical and Translational Science Institute, Tufts Medical Center, Boston, Massachusetts, United States of America, 5 Department of Medicine, Center for Genetic Epidemiology and Modeling, Tufts Medical Center, Tufts University -

Modulation of NF-Κb Signalling by Microbial Pathogens
REVIEWS Modulation of NF‑κB signalling by microbial pathogens Masmudur M. Rahman and Grant McFadden Abstract | The nuclear factor-κB (NF‑κB) family of transcription factors plays a central part in the host response to infection by microbial pathogens, by orchestrating the innate and acquired host immune responses. The NF‑κB proteins are activated by diverse signalling pathways that originate from many different cellular receptors and sensors. Many successful pathogens have acquired sophisticated mechanisms to regulate the NF‑κB signalling pathways by deploying subversive proteins or hijacking the host signalling molecules. Here, we describe the mechanisms by which viruses and bacteria micromanage the host NF‑κB signalling circuitry to favour the continued survival of the pathogen. The nuclear factor-κB (NF-κB) family of transcription Signalling targets upstream of NF‑κB factors regulates the expression of hundreds of genes that NF-κB proteins are tightly regulated in both the cyto- are associated with diverse cellular processes, such as pro- plasm and the nucleus6. Under normal physiological liferation, differentiation and death, as well as innate and conditions, NF‑κB complexes remain inactive in the adaptive immune responses. The mammalian NF‑κB cytoplasm through a direct interaction with proteins proteins are members of the Rel domain-containing pro- of the inhibitor of NF-κB (IκB) family, including IκBα, tein family: RELA (also known as p65), RELB, c‑REL, IκBβ and IκBε (also known as NF-κBIα, NF-κBIβ and the NF-κB p105 subunit (also known as NF‑κB1; which NF-κBIε, respectively); IκB proteins mask the nuclear is cleaved into the p50 subunit) and the NF-κB p100 localization domains in the NF‑κB complex, thus subunit (also known as NF‑κB2; which is cleaved into retaining the transcription complex in the cytoplasm. -

Biological and Prognostic Significance of Chromosome 5Q Deletions in Myeloid Malignancies Aristoteles A.N
Review Biological and Prognostic Significance of Chromosome 5q Deletions in Myeloid Malignancies Aristoteles A.N. Giagounidis,1Ulrich Germing,2 and Carlo Aul1 Abstract The presence of del(5q), either as the sole karyotypic abnormality or as part of a more complex karyotype, has distinct clinical implications for myelodysplastic syndromes (MDS) and acute myeloid leukemia. The 5qÀ syndrome, a subtype of low-riskMDS, is characterized by an isolated 5q deletion and <5% blasts in the bone marrow and can serve as a useful model for studying the role of 5q deletions in the pathogenesis and prognosis of myeloid malignancies. Recent clinical results with lenalidomide, an oral immunomodulatory drug, have shown durable erythroid responses, including transfusion independence and complete cytogenetic remissions in patients with del(5q) MDS with or without additional chromosomal abnormalities. These results indicate that lenalidomide can overcome the pathogenic effect of 5q deletion in MDS and restore bone marrow balance. The data provide important new insights into the pathobiology of 5q chromo- somal deletions in myeloid malignancies. Cytogenetic abnormalities are detected in the bone marrow of preponderance, refractory macrocytic anemia, normal or high over 50% of patients diagnosed with primary myelodysplastic platelet counts, hypolobulated megakaryocytes, and modest syndromes (MDS) or myeloid leukemias, and up to 80% of leukopenia (11, 14, 17). The prognosis is favorable in 5qÀ patients with secondary or therapy-related MDS (1, 2). These syndrome with relatively low risk of transformation to AML abnormalities can be characterized as being balanced or (11, 18). Although the limits of 5q deletions vary among unbalanced (3, 4). Balanced cytogenetic abnormalities include patients with 5qÀ syndrome, the most frequent deletion is reciprocal translocations, inversions, and insertions (3, 5, 6). -

Confirmation of TNIP1 and IL23A As Susceptibility Loci for Psoriatic Arthritis
Concise report Ann Rheum Dis: first published as 10.1136/ard.2011.150102 on 29 May 2011. Downloaded from Confi rmation of TNIP1 and IL23A as susceptibility loci for psoriatic arthritis John Bowes, 1 Gisela Orozco, 1 Edward Flynn, 1 Pauline Ho, 1,2 Rasha Brier, 1 Helena Marzo-Ortega, 3 Laura Coates,3 Ross McManus, 4 Anthony W Ryan, 4 David Kane, 5 Eleanor Korendowych, 6 Neil McHugh,6 Oliver FitzGerald, 7 Jonathan Packham, 8,9 Ann W Morgan, 3 Ian N Bruce, 1,2 Anne Barton 1,2 ▶ Additional data ABSTRACT different aetiologies, some differences in suscep- (supplementary tables) are Objectives To investigate a shared genetic aetiology for tibility loci would be expected. The identifi cation published online only. To view skin involvement in psoriasis and psoriatic arthritis (PsA) of risk loci specifi c to psoriasis would provide these fi les please visit the journal online at http://ard.bmj.com. by genotyping single-nucleotide polymorphisms (SNPs), compelling evidence that the genetic basis of the reported to be associated in genome-wide association skin component of the two diseases was differ- 1 Arthritis Research UK Epidemiology Unit, Manchester studies of psoriasis, in patients with PsA. ent. There has been some evidence reported to Academic Health Science Methods SNPs with reported evidence for association support this possibility. Variants within the LCE Centre, The University of with psoriasis were genotyped in a PsA case and control gene locus were reported to be associated with Manchester, Manchester, UK collection from the UK and Ireland. Genotype and allele psoriasis but not PsA in a German cohort, 10 but a 2 The Kellgren Centre for Rheumatology, Central frequencies were compared between PsA cases and subsequent study in a population from the British Manchester Foundation controls using the Armitage test for trend. -

Confirmation of TNIP1 but Not RHOB and PSORS1C1 As Systemic Sclerosis Risk Factors in a Large Independent Replication Study
Downloaded from ard.bmj.com on August 13, 2013 - Published by group.bmj.com Basic and translational research EXTENDED REPORT Confirmation of TNIP1 but not RHOB and PSORS1C1 as systemic sclerosis risk factors in a large independent replication study Lara Bossini-Castillo,1 Jose Ezequiel Martin,1 Jasper Broen,2 Carmen P Simeon,3 Lorenzo Beretta,4 Olga Y Gorlova,5 Madelon C Vonk,2 Norberto Ortego-Centeno,6 Gerard Espinosa,7 Patricia Carreira,8 Paloma García de la Peña,9 Natividad Oreiro,10 José Andrés Román-Ivorra,11 María Jesús Castillo,12 Miguel A González-Gay,13 Luis Sáez-Comet,14 Ivan Castellví,15 Annemie J Schuerwegh,16 Alexandre E Voskuyl,17 Anna-Maria Hoffmann-Vold,18 Roger Hesselstrand,19 Annika Nordin,20 Claudio Lunardi,21 Raffaella Scorza,4 Jacob M van Laar,22 Paul G Shiels,23 Ariane Herrick,24 Jane Worthington,24 Carmen Fonseca,25 Christopher Denton,25 Filemon K Tan,26 Frank C Arnett,26 Shervin Assassi,26 Bobby P Koeleman,27 Maureen D Mayes,26 Timothy R D J Radstake,2,28 Javier Martin,1 the Spanish Scleroderma Group* ▸ Additional supplementary ABSTRACT different internal organs.1 The contribution of data are published online only. Introduction A recent genome-wide association study fi different genetic factors to the development and To view these les please visit fi 2 the journal online (http://dx.doi. in European systemic sclerosis (SSc) patients identi ed prognosis of the disease is now widely accepted. org/10.1136/annrheumdis- three loci (PSORS1C1, TNIP1 and RHOB)asnovel Over the past few years, genome-wide association 2012-201888.bmj.com). -

Recombinant Human TNIP1 Protein Catalog Number: ATGP0780
Recombinant human TNIP1 protein Catalog Number: ATGP0780 PRODUCT INPORMATION Expression system E.coli Domain 94-530aa UniProt No. Q15025 NCBI Accession No. NP_006049 Alternative Names TNFAIP3 interacting protein 1, ABIN-1, NAF1, VAN, Nip40-1 PRODUCT SPECIFICATION Molecular Weight 51.8 kDa (458aa) confirmed by MALDI-TOF Concentration 0.25mg/ml (determined by Bradford assay) Formulation Liquid in. 20mM Tris-HCl buffer (pH 7.5) containing 20% glycerol, 5mM DTT, 200mM NaCl Purity > 75% by SDS-PAGE Tag His-Tag Application SDS-PAGE Storage Condition Can be stored at +2C to +8C for 1 week. For long term storage, aliquot and store at -20C to -80C. Avoid repeated freezing and thawing cycles. BACKGROUND Description TNIP1 (TNFAIP3-interacting protein 1) has been shown to interacts with zinc finger protein A20/TNFAIP3 and inhibits TNF-induced NF-kappa-B-dependent gene expression by interfering with an RIP- or TRAF2-mediated transactivation signal. In addition, interacts with HIV-1 matrix protein and is packaged into virions and overexpression can inhibit viral replication. It may regulate matrix nuclear localization, both nuclear import of PIC (Preintegration complex) and export of GAG polyprotein and viral genomic RNA during virion production. Recombinant human TNIP1 protein, fused to His-tag at N-terminus, was expressed in E. coli and purified by using 1 Recombinant human TNIP1 protein Catalog Number: ATGP0780 conventional chromatography techniques. Amino acid Sequence MGSSHHHHHH SSGLVPRGSH MSNVTASPTA PACPSDKPAP VQKPPSSGTS SEFEVVTPEE QNSPESSSHA NAMALGPLPR EDGNLMLHLQ RLETTLSVCA EEPDHGQLFT HLGRMALEFN RLASKVHKNE QRTSILQTLC EQLRKENEAL KAKLDKGLEQ RDQAAERLRE ENLELKKLLM SNGNKEGASG RPGSPKMEGT GKKAVAGQQQ ASVTAGKVPE VVALGAAEKK VKMLEQQRSE LLEVNKQWDQ HFRSMKQQYE QKITELRQKL ADLQKQVTDL EAEREQKQRD FDRKLLLAKS KIEMEETDKE QLTAEAKELR QKVKYLQDQL SPLTRQREYQ EKEIQRLNKA LEEALSIQTP PSSPPTAFGS PEGAGALLRK QELVTQNELL KQQVKIFEED FQRERSDRER MNEEKEELKK QVEKLQAQVT LSNAQLKAFK DEEKAREALR QQKRKAKA General References He CF., et al. -

Newly Identified Gon4l/Udu-Interacting Proteins
www.nature.com/scientificreports OPEN Newly identifed Gon4l/ Udu‑interacting proteins implicate novel functions Su‑Mei Tsai1, Kuo‑Chang Chu1 & Yun‑Jin Jiang1,2,3,4,5* Mutations of the Gon4l/udu gene in diferent organisms give rise to diverse phenotypes. Although the efects of Gon4l/Udu in transcriptional regulation have been demonstrated, they cannot solely explain the observed characteristics among species. To further understand the function of Gon4l/Udu, we used yeast two‑hybrid (Y2H) screening to identify interacting proteins in zebrafsh and mouse systems, confrmed the interactions by co‑immunoprecipitation assay, and found four novel Gon4l‑interacting proteins: BRCA1 associated protein‑1 (Bap1), DNA methyltransferase 1 (Dnmt1), Tho complex 1 (Thoc1, also known as Tho1 or HPR1), and Cryptochrome circadian regulator 3a (Cry3a). Furthermore, all known Gon4l/Udu‑interacting proteins—as found in this study, in previous reports, and in online resources—were investigated by Phenotype Enrichment Analysis. The most enriched phenotypes identifed include increased embryonic tissue cell apoptosis, embryonic lethality, increased T cell derived lymphoma incidence, decreased cell proliferation, chromosome instability, and abnormal dopamine level, characteristics that largely resemble those observed in reported Gon4l/udu mutant animals. Similar to the expression pattern of udu, those of bap1, dnmt1, thoc1, and cry3a are also found in the brain region and other tissues. Thus, these fndings indicate novel mechanisms of Gon4l/ Udu in regulating CpG methylation, histone expression/modifcation, DNA repair/genomic stability, and RNA binding/processing/export. Gon4l is a nuclear protein conserved among species. Animal models from invertebrates to vertebrates have shown that the protein Gon4-like (Gon4l) is essential for regulating cell proliferation and diferentiation. -

Cep-2020-00633.Pdf
Clin Exp Pediatr Vol. 64, No. 5, 208–222, 2021 Review article CEP https://doi.org/10.3345/cep.2020.00633 Understanding the genetics of systemic lupus erythematosus using Bayesian statistics and gene network analysis Seoung Wan Nam, MD, PhD1,*, Kwang Seob Lee, MD2,*, Jae Won Yang, MD, PhD3,*, Younhee Ko, PhD4, Michael Eisenhut, MD, FRCP, FRCPCH, DTM&H5, Keum Hwa Lee, MD, MS6,7,8, Jae Il Shin, MD, PhD6,7,8, Andreas Kronbichler, MD, PhD9 1Department of Rheumatology, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea; 2Severance Hospital, Yonsei University College of Medicine, Seoul, Korea; 3Department of Nephrology, Yonsei University Wonju College of Medicine, Wonju, Korea; 4Division of Biomedical Engineering, Hankuk University of Foreign Studies, Yongin, Korea; 5Department of Pediatrics, Luton & Dunstable University Hospital NHS Foundation Trust, Luton, UK; 6Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea; 7Division of Pediatric Nephrology, Severance Children’s Hospital, Seoul, Korea; 8Institute of Kidney Disease Research, Yonsei University College of Medicine, Seoul, Korea; 9Department of Internal Medicine IV (Nephrology and Hypertension), Medical University Innsbruck, Innsbruck, Austria 1,3) The publication of genetic epidemiology meta-analyses has analyses have redundant duplicate topics and many errors. increased rapidly, but it has been suggested that many of the Although there has been an impressive increase in meta-analyses statistically significant results are false positive. In addition, from China, particularly those on genetic associa tions, most most such meta-analyses have been redundant, duplicate, and claimed candidate gene associations are likely false-positives, erroneous, leading to research waste. In addition, since most suggesting an urgent global need to incorporate genome-wide claimed candidate gene associations were false-positives, cor- data and state-of-the art statistical inferences to avoid a flood of rectly interpreting the published results is important. -

Research Article Altered AKT1 and MAPK1 Gene
Hindawi Publishing Corporation Mediators of Inflammation Volume 2012, Article ID 495934, 14 pages doi:10.1155/2012/495934 Research Article Altered AKT1 and MAPK1 Gene Expression on Peripheral Blood Mononuclear Cells and Correlation with T-Helper-Transcription Factors in Systemic Lupus Erythematosus Patients Sonia Garcia-Rodriguez,1 Jose-Luis Callejas-Rubio,2 Norberto Ortego-Centeno,2 Esther Zumaquero,1, 3 Raquel Rıos-Fernandez,´ 2 Salvador Arias-Santiago,4 Pilar Navarro,1 Jaime Sancho,1 and Mercedes Zubiaur1 1 Department of Cellular Biology and Immunology, Instituto de Parasitolog´ıa y Biomedicina Lopez-Neyra,´ (IPBLN-CSIC), Parque Tecnologico´ Ciencias de la Salud, Avenida Conocimiento s/n, Armilla, 18100 Granada, Spain 2 Systemic Autoimmune Diseases Unit, Department of Internal Medicine, San Cecilio University Hospital (SCUH), Avenida Dr. Oloriz, no. 16, Granada 18012, Spain 3 Department of Microbiology, University of Alabama at Birmingham, 1720 2nd Ave South, Birmingham, AL 35294, USA 4 Department of Dermatology, SCUH, Avenida Dr. Oloriz, No. 16, Granada 18012, Spain Correspondence should be addressed to Mercedes Zubiaur, [email protected] Received 9 May 2012; Revised 21 August 2012; Accepted 3 September 2012 Academic Editor: Eric F. Morand Copyright © 2012 Sonia Garcia-Rodriguez et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Kinases have been implicated in the immunopathological mechanisms of Systemic Lupus Erythematosus (SLE). v-akt murine- thymoma viral-oncogene-homolog 1 (AKT1) and mitogen-activated-protein-kinase 1 (MAPK1) gene expressions in peripheral mononuclear cells from thirteen SLE patients with inactive or mild disease were evaluated using quantitative real-time reverse- transcription polymerase-chain-reaction and analyzed whether there was any correlation with T-helper (Th) transcription factors (TF) gene expression, cytokines, and S100A8/S100A9-(Calprotectin). -
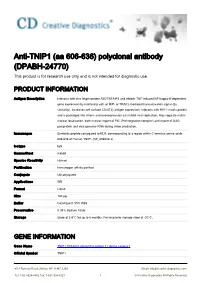
Anti-TNIP1 (Aa 606-636) Polyclonal Antibody (DPABH-24770) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-TNIP1 (aa 606-636) polyclonal antibody (DPABH-24770) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Interacts with zinc finger protein A20/TNFAIP3 and inhibits TNF-induced NF-kappa-B-dependent gene expression by interfering with an RIP- or TRAF2-mediated transactivation signal (By similarity). Increases cell surface CD4(T4) antigen expression. Interacts with HIV-1 matrix protein and is packaged into virions and overexpression can inhibit viral replication. May regulate matrix nuclear localization, both nuclear import of PIC (Preintegration complex) and export of GAG polyprotein and viral genomic RNA during virion production. Immunogen Synthetic peptide conjugated to KLH, corresponding to a region within C terminal amino acids 606-636 of Human TNIP1 (NP_006049.3). Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB Format Liquid Size 100 μg Buffer Constituent: 99% PBS Preservative 0.09% Sodium Azide Storage Store at 2-8°C for up to 6 months. For long term storage store at -20°C. GENE INFORMATION Gene Name TNIP1 TNFAIP3 interacting protein 1 [ Homo sapiens ] Official Symbol TNIP1 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Synonyms TNIP1; TNFAIP3 interacting protein 1; TNFAIP3-interacting protein 1; ABIN 1; KIAA0113; NAF1; Nef associated factor 1 SNP; VAN; virion associated nuclear shuttling protein; Nef-associated factor 1 SNP; HIV-1 Nef-interacting protein; virion-associated nuclear shuttling protein; ABIN-1; nip40-1; Entrez Gene ID 10318 Protein Refseq NP_001239314 UniProt ID B7Z8K2 Chromosome Location 5q32-q33.1 Pathway EGFR1 Signaling Pathway; TNF-alpha/NF-kB Signaling Pathway; Function protein binding; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

Association Between TNIP1, MPHOSPH6 and ZNF208 Genetic Polymorphisms and the Coronary Artery Disease Risk in Chinese Han Population
www.impactjournals.com/oncotarget/ Oncotarget, Advance Publications 2017 Association between TNIP1, MPHOSPH6 and ZNF208 genetic polymorphisms and the coronary artery disease risk in Chinese Han population Yanbin Song1,2,3, Mengdan Yan1,2, Jing Li1,2, Jingjie Li1,2, Tianbo Jin1,2 and Chao Chen1,2 1Key Laboratory of Resource Biology and Biotechnology in Western China (Northwest University), Ministry of Education, Xi’an, Shaanxi 710069, China 2School of Life Sciences, Northwest University, Xi’an, Shaanxi 710069, China 3Department of Cardiovascular, Yanan University Affiliated Hospital, Yanan, Shaanxi 716000, China Correspondence to: Tianbo Jin, email: [email protected] Chao Chen, email: [email protected] Keywords: coronary artery disease (CAD), polymorphisms, ZNF208, TNIP1, MPHOSPH6 Received: May 18, 2017 Accepted: June 24, 2017 Published: August 24, 2017 Copyright: Song et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT Introduction: Coronary artery disease (CAD) is a common disease and among the leading cause of death in the general population. Inherited factors are involved in the pathogenesis of CAD. Aims: Our study examined whether SNPs in TNIP1, MPHOSPH6, ZNF208 to be associated with CAD risk in a Chinese Han population. We recruited 596 CAD patients, 603 controls and genotyping fifteen SNPs using Sequenom MassARRAY. For association analysis between TNIP1, MPHOSPH6 and ZNF208 and CAD was determined by Odds ratios (ORs) with 95% confidence intervals (CIs) using Logistic Regression. Results: The results indicated in allel model, the rs960709 in TNIP1 was associated with CAD risk (OR = 0.78, 95%CI = 0.65-0.94, P=0.010).