Emerging Health Threats Journal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

C 367 Jornal Oficial
Jornal Oficial C 367 da União Europeia 57.º ano Edição em língua portuguesa Comunicações e Informações 16 de outubro de 2014 Índice IV Informações INFORMAÇÕES DAS INSTITUIÇÕES, ÓRGÃOS E ORGANISMOS DA UNIÃO EUROPEIA Parlamento Europeu PERGUNTAS ESCRITAS E SUA RESPOSTA 2014/C 367/01 Perguntas escritas apresentadas por deputados ao Parlamento Europeu e respetiva resposta dada por uma instituição da União Europeia ......................................................................................................................... 1 (Ver nota ao leitor) PT Nota ao leitor A presente publicação contém perguntas escritas apresentadas por deputados ao Parlamento Europeu e a respetiva resposta dada por uma instituição da União Europeia. Para cada pergunta e resposta é apresentada, antes de uma eventual tradução, a versão na língua original. Por vezes, a resposta pode ser dada numa língua que não seja a da pergunta. Isto depende da língua de trabalho da comissão a quem é requerida a resposta. Estas perguntas e respostas são publicadas nos termos dos artigos 117.º e 118.º do Regimento do Parlamento Europeu. Todas as perguntas e respostas são acessíveis através do website do Parlamento Europeu (Europarl) na rubrica «Perguntas parlamentares»: http://www.europarl.europa.eu/plenary/pt/parliamentary-questions.html SIGNIFICADO DAS SIGLAS DOS GRUPOS POLÍTICOS PPE Grupo do Partido Popular Europeu (Democratas-Cristãos) S&D Grupo da Aliança Progressista dos Socialistas e Democratas no Parlamento Europeu ALDE Grupo da Aliança dos Democratas e Liberais pela -
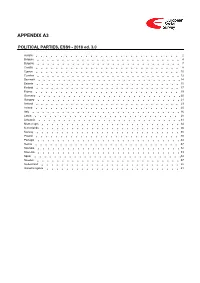
ESS9 Appendix A3 Political Parties Ed
APPENDIX A3 POLITICAL PARTIES, ESS9 - 2018 ed. 3.0 Austria 2 Belgium 4 Bulgaria 7 Croatia 8 Cyprus 10 Czechia 12 Denmark 14 Estonia 15 Finland 17 France 19 Germany 20 Hungary 21 Iceland 23 Ireland 25 Italy 26 Latvia 28 Lithuania 31 Montenegro 34 Netherlands 36 Norway 38 Poland 40 Portugal 44 Serbia 47 Slovakia 52 Slovenia 53 Spain 54 Sweden 57 Switzerland 58 United Kingdom 61 Version Notes, ESS9 Appendix A3 POLITICAL PARTIES ESS9 edition 3.0 (published 10.12.20): Changes from previous edition: Additional countries: Denmark, Iceland. ESS9 edition 2.0 (published 15.06.20): Changes from previous edition: Additional countries: Croatia, Latvia, Lithuania, Montenegro, Portugal, Slovakia, Spain, Sweden. Austria 1. Political parties Language used in data file: German Year of last election: 2017 Official party names, English 1. Sozialdemokratische Partei Österreichs (SPÖ) - Social Democratic Party of Austria - 26.9 % names/translation, and size in last 2. Österreichische Volkspartei (ÖVP) - Austrian People's Party - 31.5 % election: 3. Freiheitliche Partei Österreichs (FPÖ) - Freedom Party of Austria - 26.0 % 4. Liste Peter Pilz (PILZ) - PILZ - 4.4 % 5. Die Grünen – Die Grüne Alternative (Grüne) - The Greens – The Green Alternative - 3.8 % 6. Kommunistische Partei Österreichs (KPÖ) - Communist Party of Austria - 0.8 % 7. NEOS – Das Neue Österreich und Liberales Forum (NEOS) - NEOS – The New Austria and Liberal Forum - 5.3 % 8. G!LT - Verein zur Förderung der Offenen Demokratie (GILT) - My Vote Counts! - 1.0 % Description of political parties listed 1. The Social Democratic Party (Sozialdemokratische Partei Österreichs, or SPÖ) is a social above democratic/center-left political party that was founded in 1888 as the Social Democratic Worker's Party (Sozialdemokratische Arbeiterpartei, or SDAP), when Victor Adler managed to unite the various opposing factions. -

MATCHING SPORTS EVENTS and HOSTS Published April 2013 © 2013 Sportbusiness Group All Rights Reserved
THE BID BOOK MATCHING SPORTS EVENTS AND HOSTS Published April 2013 © 2013 SportBusiness Group All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher. The information contained in this publication is believed to be correct at the time of going to press. While care has been taken to ensure that the information is accurate, the publishers can accept no responsibility for any errors or omissions or for changes to the details given. Readers are cautioned that forward-looking statements including forecasts are not guarantees of future performance or results and involve risks and uncertainties that cannot be predicted or quantified and, consequently, the actual performance of companies mentioned in this report and the industry as a whole may differ materially from those expressed or implied by such forward-looking statements. Author: David Walmsley Publisher: Philip Savage Cover design: Character Design Images: Getty Images Typesetting: Character Design Production: Craig Young Published by SportBusiness Group SportBusiness Group is a trading name of SBG Companies Ltd a wholly- owned subsidiary of Electric Word plc Registered office: 33-41 Dallington Street, London EC1V 0BB Tel. +44 (0)207 954 3515 Fax. +44 (0)207 954 3511 Registered number: 3934419 THE BID BOOK MATCHING SPORTS EVENTS AND HOSTS Author: David Walmsley THE BID BOOK MATCHING SPORTS EVENTS AND HOSTS -

Chronic Multisymptom Illness Affecting Air Force Veterans of the Gulf War
Chronic Multisymptom Illness Affecting Air Force Veterans of the Gulf War Keiji Fukuda, MD, MPH; Rosane Nisenbaum, PhD; Geraldine Stewart, MA; William W. Thompson, PhD; Laura Robin, DO, MPH; Rita M. Washko, MD; Donald L. Noah, DVM, MPH; Drue H. Barrett, PhD, MS; Bonnie Randall, MCP; Barbara L. Herwaldt, MD, MPH; Alison C. Mawle, PhD; William C. Reeves, MD, MSPH Context.—Gulf War (GW) veterans report nonspecific symptoms significantly was much lower than expected.9 No spe- more often than their nondeployed peers. However, no specific disorder has been cific illness is evident among the 18 598 identified, and the etiologic basis and clinical significance of their symptoms remain GW veterans, according to the Depart- unclear. ment of Defense Comprehensive Clini- 6 Objectives.—To organize symptoms reported by US Air Force GW veterans into cal Evaluation Program. Other investi- a case definition, to characterize clinical features, and to evaluate risk factors. gators have found no unusual increases in birth defects,10 unexplained illness,11 Design.—Cross-sectional population survey of individual characteristics and excess hospitalizations,12 or excess mor- symptoms and clinical evaluation (including a structured interview, the Medical tality13 among GW veterans. However, Outcomes Study Short Form 36, psychiatric screening, physical examination, clini- one study reported excess mortality due cal laboratory tests, and serologic assays for antibodies against viruses, rickettsia, to unintentional injuries rather than parasites, and bacteria) conducted in 1995. from disease.14 Evidence of an Iraqi Participants and Setting.—The cross-sectional questionnaire survey included chemical and biological weapons pro- 3723 currently active volunteers, irrespective of health status or GW participation, gram has been documented,15 and al- from 4 air force populations.The cross-sectional clinical evaluation included 158 though use of such weapons during the GW veterans from one unit, irrespective of health status. -

February 27, 2018Ighp
iGHP Special Lecture series "How Does Politics Influence Global Health Policy? Antimicrobial Resistance (AMR) and Pandemic Influenza" Institute for Global Health Policy Research (iGHP), the Bureau of International Health Cooperation, in joint collaboration with the Disease Control and Prevention Center (DCC) of National Center for Global Health and Medicine (NCGM), is pleased to announce the upcoming seminar entitled, "How Does Politics Influence Global Health Policy?: AMR and Pandemic Influenza", which is to be held on February 27, 2018 in Tokyo. The seminar includes a special lecture by Professor Keiji Fukuda, the Director and Clinical Professor at the University of Hong Kong School of Public Health, and a panel discussion with Japanese leading experts in the fields of infectious diseases and epidemiology who have extensive knowledge and experiences in clinical practice, research, education, and domestic and international health policy. 1. Seminar Details Date & Time Tuesday, February 27, 2018, 17:00-19:00 Venue Institute for Global Health Policy Research, Bureau of International Cooperation (Ground floor, Training Center Building), National Center for Global Health and Medicine, Tokyo Access http://kyokuhp.ncgm.go.jp/eng/aboutus/access.html Language English only (No Japanese interpretation will be available) Participation Free of charge and open to general public, and a light meal will be provided. Seating capacity Approximately 80 2. Agenda (tentative) 17:00-17:05 Welcome Remarks (Kenji Shibuya, Director, Institute for Global Health -

Court 8 8 SEZGIN ABDULLATIF 17128 2 4 17851 MAOR ZUKER POLITIS
17. Zagreb Croatia Open 2011 D 19 SENIORI SM-54 court 8 SUBOTA 05. 11. 2011 17053 ANCA GULLA DIEGO VICENTE 8 13 SEZGIN ABDULLATIF 17128 1 3 ARGENTINA ARGENTINA BAYERISCHE TAEKWONDO UNION GERMANY 17053 2417128 17 21 ARGENTINA GERMANY 17851 MAOR ZUKER POLITIS NIKOLAOS 17766 16 13 ISRAEL TEAM OR TEAM -AHI YEHUDA CLUB 2 10 TAEKWONDO UNION OF NORTH GREECE GREECE 17279 7717228 45 47 ISRAEL SPAIN 6 JAKE CONCANNON 17601 11 SPORT TAEKWONDO IRELAND 17707 MUTH IVAN 8 7 17228 12 6 HRVATSKA TAEKWONDO KLUB OSVIT SPAIN PABLO CAROU 17228 19 9 GALICIA TAEKWONDO FEDERATION SPAIN 17279 17228 18 17502 22 ISRAEL 59SERBIA SPAIN 17279 SAHAR BELLO NAIM SOLTANI 17184 8 5 ISRAEL ISRAEL - NATIONAL TEAM 10 2 DANISH TAEKWONDO FEDERATION DENMARK 17502 98 17228 59 60 SERBIA SPAIN 66 17502 GLADOVIC MILOS 13 8 EDI SERBANESCU 17277 10 7 SERBIA SERBIAN NATIONAL TEAM ISRAEL - NATIONAL TEAM ISRAEL 17502 5417277 19 23 SERBIA ISRAEL 17260 MEYSAM KHODADAD KANJOOBE GLUSHENKO DMYTRO 17286 6 9 IRAN IRAN NATIONAL TEAM 7 5 KIEV-KWON UKRAINE 17502 17277 46 48 SERBIA 15 3 ISRAEL 17791 SEFKAME SAMIR 6 7 GUY SHIMON 17850 14 15 CENTRAL AFRICAN REPUBLIC TAIPA TEAM OR TEAM -AHI YEHUDA CLUB ISRAEL 17791 5 1 17850 5 7 CENTRAL AFRICAN REPUBLIC ISRAEL 17880 KAMCI MEHMET TIBO JENSEN 17866 18 17 GERMANY TEAM TSV DACHAU 2 2 TEAM SWEDEN SWEDEN 17791 17088 20 24 CENTRAL A 32POLAND 17162 CLAYTON DOS SANTOS MECMAJER JAROSLAW 17088 4 2 BRAZIL BRAZILIAN NATIONAL TEAM 1 12 AZS OS POZNAN POLAND 17. Zagreb Croatia Open 2011 D 29 SENIORI SM-58 court 3 SUBOTA 05. -

Global Study on Homicide 2011
GLOBAL STUDY ON HOMICIDE 2011 TRENDS / CONTEXTS DATA UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna 2011 GLOBAL STUDY ON HOMICIDE TRENDS, CONTEXTS, DATA Copyright 2011 © United Nations Office on Drugs and Crime (UNODC) Acknowledgements The 2011 Global Study on Homicide was prepared by the Statistics and Surveys Section under the supervision of Sandeep Chawla, Director, Division for Policy Analysis and Public Affairs. Core team Research coordination and study preparation Angela Me, Enrico Bisogno, Steven Malby Research, data analysis and data processing Michael Jandl, Philip Davis, Catherine Pysden, Umidjon Rahmonberdiev, Felix Reiterer, Elizabeth Gurian, Cristina Mesa Vieira, Alberto Aziani and Mariaelena Cenci Editing Jonathan Gibbons Graphic design, layout and mapping support Suzanne Kunnen and Kristina Kuttnig (Studies and Threat Analysis Section) The study benefited from the valuable input of many UNODC staff members (at headquarters and in regional and country offices) as well as from the dedica- tion of the many national experts who have provided UNODC with crime and criminal justice data over the years. The World Health Organization kindly provided the public health data pre- sented in the study. The Organization of American States supported UNODC in the collection of data in the Americas. Many experts in research institutes and international organizations commented on early drafts and provided extremely valuable input. The study was also made possible thanks to the financial contribution of the Small Arms Survey. DISCLAIMERS This study has not been formally edited. The designations employed and the presentation of the material in this publica- tion do not imply the expression of any opinion whatsoever on the part of UNODC or the Secretariat of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimi- tation of its frontiers or boundaries. -

Nutraceutical Support in Heart Failure: a Position Paper of the International Lipid Expert Panel (ILEP)
Nutrition Research Reviews (2020), 33, 155–179 doi:10.1017/S0954422420000049 © The Author(s) 2020. This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http:// creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. Nutraceutical support in heart failure: a position paper of the International Lipid Expert Panel (ILEP) Arrigo F. G. Cicero1*, Alessandro Colletti2, Stephan von Haehling3, Dragos Vinereanu4, Agata Bielecka-Dabrowa5, Amirhossein Sahebkar6,7,8, Peter P. Toth9, Željko Reiner10, Nathan D. Wong11, Dimitri P. Mikhailidis12, Claudio Ferri13 and Maciej Banach14,15,16* on behalf of the International Lipid Expert Panel† 1Department of Medical and Surgical Sciences, University of Bologna, Bologna, Italy 2Department of Science and Drug Technology, University of Turin, Turin, Italy 3Department of Cardiology and Pneumology, University of Goettingen Medical Center, Goettingen, Germany; German Center for Cardiovascular Disorders (DZHK), partner site Goettingen, Germany 4University of Medicine and Pharmacy Carol Davila, University and Emergency Hospital, Bucharest, Romania 5Department of Cardiology and Congenital Diseases of Adults, Polish Mother’s Memorial Hospital Research Institute (PMMHRI), Lodz, Poland 6Halal Research Center of IRI, FDA, Tehran, Iran 7Biotechnology Research Center, Pharmaceutical Technology Institute, Mashhad University of Medical Sciences, Mashhad, Iran 8Neurogenic -
Introduction to the World Health Assembly: a Briefing for New Delegates
Introduction to the World Health Assembly: A Briefing for New Delegates Organised by the Global Health Centre at the Graduate Institute and the United Nations Foundation Biographies of Speakers 22 May 2016 Maison de la paix The Graduate Institute, Geneva | 14:30 – 15:00 | NETWORKING COFFEE | 15:00 – 15:10 | WELCOME JOHN E. LANGE Ambassador; Senior Fellow for Global Health Diplomacy, United Nations Foundation Ambassador (Retired) John E. Lange is the Senior Fellow for Global Health Diplomacy at the United Nations Foundation in Washington, DC. He is one of the leaders of the Global Polio Eradication Initiative in his capacity as co-chair of the Polio Partners Group. Lange worked at the Bill & Melinda Gates Foundation from 2009-2013, where he engaged in high-level advocacy with governments to advance the foundation’s global health goals in Africa. Ambassador Lange had a distinguished 28-year career in the Foreign Service at the U.S. Department of State, where he was a pioneer in the field of global health diplomacy. He served as the Special Representative on Avian and Pandemic Influenza; Deputy U.S. Global AIDS Coordinator at the inception of the President’s Emergency Plan for AIDS Relief; and U.S. Ambassador to Botswana (1999-2002), where HIV/AIDS was his signature issue. Lange headed the U.S. Embassy in Dar es Salaam, Tanzania, as chargé d'affaires during the August 7, 1998, terrorist bombing. Earlier, he served at the U.S. Mission to the UN in Geneva and at U.S. Embassies in Lomé, Paris and Mexico City. Ambassador Lange is the author of a case study on pandemic influenza negotiations in the book “Negotiating and Navigating Global Health: Case Studies in Global Health Diplomacy” (2012). -

Emergent Covid-19 and Sars-Cov-2 in Social Imagery and Social Video: Initial Three Months of Viral Dispersion
PART I PART 1: GLOBAL PUBLIC HEALTH 13 11 EMERGENT COVID-19 AND SARS-COV-2 IN SOCIAL IMAGERY AND SOCIAL VIDEO: INITIAL THREE MONTHS OF VIRAL DISPERSION Shalin Hai-Jew 15 16 EMERGENT COVID-19 AND SARS-COV-2: THREE MONTHS VIRAL DISPERSION Abstract The pandemic potential of emergent SARS-CoV-2, a zoonotic virus which causes COVID-19, has captured the world’s attention, through formal mass media and informal social media (esp. social imagery and social video). This work explores multiple social imagesets (thousands of images) from Google Images (captured from various seeding terms related to the outbreak) and social video transcripts from Google’s YouTube platform to infer focuses of mass human attention in terms of (1) messaging and information sourcing, (2) meta-messaging and subtexts, and (3) invisibilities (what is not expressed). This compares the imageset messaging against mass media articles from the same time frame. This work has implications for a mass-scale social response to an unfolding global biosafety/biosecurity risk based on learning from more organic and emergent social communications. Key Words Novel Coronavirus, 2019-nCoV, COVID-19 disease, SARS- CoV-2, Severe Acute Respiratory Illness, Community Spread, Self-Quarantine, Quarantine, Social Distancing, Chains of Infec- tion, Contact Tracing EMERGENT COVID-19 AND SARS-COV-2: THREE MONTHS VIRAL DISPERSION 17 Introduction “Assume this virus is everywhere. This is a global influenza pan- demic caused by a coronavirus.” — Michael Osterholm in Peter Bergen’s “The disease expert who warned us” in CNN (March 10, 2020) COVID-19, the disease outbreak caused by the novel zoonotic virus termed SARS-CoV-2 (and prior, 2019-nCoV), is a major threat to human health in part because people do not have a natural immunity to this pathogen, which spreads quickly and invisibly. -
Annual Report 2011 1 2 Annual Report 2011
Annual Report 2011 1 2 Annual Report 2011 Sparkasse Bank dd Tran. account: 1990000000000023 Founded in: 1999. IB.: 4200128200006 SWIFT: ABSBBA 22 Figures 2011: Owner: Steiermaerkische Sparkasse Austrija Head office Number of employees: 432 Zmaja od Bosne 7 Number of affiliates: 45 71000 Sarajevo, BiH Number of clients: app. 180.000 Tel: +387 (0)33 28 03 00 Fax: +387 (0)33 28 02 31 E-mail: [email protected] www.sparkasse.ba Key bodies MANAGEMENT BOARD SUPERVISORY BOARD AUDITING BOARD CEO Chairman Chairman Sanel Kusturica, MBA Sava Dalbokov, MBA Samir Omerhodžić Executive director Members Members Zahida Karić, MBA Mag. Franz Kerber Walburga Seidl Hamdija Alagić Guenter Schneider Executive director Mag. Renate Ferlitz Aleksandar Klemenčić (until 01.11.2011.) Nedim Alihodžić Dr. Georg Bucher Slaviša Kojić Manfred Lackner (from 01.11.2011.) Executive director Amir Softić 2.98% Ownership structure Steiermärkische Sparkasse Others 97.02% Annual Report 2011 3 Annual Report 2011 Management on 2011 5 Economy & Banking sector in 2011 8 2011 in numbers 12 Companies of the “S” brand in BiH 14 The most socially responsible company in BiH in 2011 17 Our clients 20 - 26 Financial Statements 27 4 Annual Report 2011 Annual Report 2011 5 Management on 2011 To our shareholders, business partners, clients and employees Sanel Kusturica, Director Retail and Corporate, Legal operations, Human resources It is my great pleasure to have the opportunity to give you a short over- view of the achievements of the Sparkasse Bank in Bosnia and Herze- govina in 2011, which I believe have brought us another step closer to our long-term development strategy and reaching the top of the bank- ing market in Bosnia and Herzegovina. -

GEM 2020/2021 Global Report
2020/2021 Global Report AUTHORS Professor Niels Bosma, PhD, Utrecht University, Netherlands Professor Stephen Hill, DSc, Lead Author Aileen Ionescu-Somers, PhD, GEM Executive Director Professor Donna Kelley, PhD, Babson College, United States Professor Maribel Guerrero, PhD, Universidad del Desarrollo, Chile Professor Thomas Schott, PhD, University of Southern Denmark, Denmark Although GEM data were used in the preparation of this report, their interpretation and use are the sole responsibility of the authors. GEM GLOBAL SPONSOR/FOUNDING INSTITUTION GEM GLOBAL REPORT SPONSOR ACKNOWLEDGEMENTS Special thanks to Francis Carmona, Forrest Wright and Alicia Coduras for the data analysis and preparation of tables and country data, to Laura Freeborn for coordinating report content, to Kevin Anselmo for editing support, writing the entrepreneur profiles and coordinating the communications outreach of the Global Report, and to Dean Bargh of Witchwood Production House and Chris Reed of BBR Design for design, copy-editing, layout and project management. We are particularly grateful to Forrest for writing the Policy Roadmaps in the Economy Profiles section. We would also like to acknowledge the GEM National Teams for overseeing the GEM Adult Population Survey and conducting the National Expert Survey, as well as contributing their local knowledge about entrepreneurship in their economies. We thank the entire GEM central administrative and technical team, the GEM Research & Innovation Projects teams (GRIPs), and the board of directors for their oversight.