MODULE 2 Types of Vaccine and Adverse Reactions MODULE 2: Types of Vaccine and Adverse Reactions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Introduction of Inactivated Poliovirus Vaccine and Impact on Vaccine- Associated Paralytic Poliomyelitis — Beijing, China, 2014–2016
Morbidity and Mortality Weekly Report Introduction of Inactivated Poliovirus Vaccine and Impact on Vaccine- Associated Paralytic Poliomyelitis — Beijing, China, 2014–2016 Dan Zhao, MD1; Rui Ma, MD1; Tao Zhou, MD1; Fan Yang, MD1; Jin Wu, MD2; Hao Sun3; Fang Liu, MD4; Li Lu, MD1; Xiaomei Li1; Shuyan Zuo, MD5; Wei Yao6; JianYin6 When included in a sequential polio vaccination schedule, the risk for VAPP associated with subsequent OPV doses. inactivated polio vaccine (IPV) reduces the risk for vaccine- Countries that have previously introduced at least 1 IPV dose associated paralytic poliomyelitis (VAPP), a rare adverse event before vaccination with OPV have rapidly eliminated VAPP associated with receipt of oral poliovirus vaccine (OPV). (1). IPV has been available in China’s private sector since During January 2014, the World Health Organization (WHO) 2009. After completion of immunogenicity studies (3–5), recommended introduction of at least 1 IPV dose into routine Beijing introduced IPV into the public sector EPI program in immunization schedules in OPV-using countries (1). The December 2014 as part of a sequential schedule that included Polio Eradication and Endgame Strategic Plan 2013–2018 1 dose of IPV at age 2 months, followed by 3 doses of trivalent recommended completion of IPV introduction in 2015 and OPV at ages 3, 4, and 48 months. After the global synchronized globally synchronized withdrawal of OPV type 2 in 2016 (2). withdrawal of all Sabin type 2 vaccines in April 2016, trivalent Introduction of 1 dose of IPV into Beijing’s Expanded Program OPV was replaced with bivalent OPV, which contains types 1 on Immunization (EPI) on December 5, 2014 represented and 3 oral polio vaccine viruses. -
Valuing the Cost of Improving Chilean Primary Vaccination: a Cost Minimization Analysis of a Hexavalent Vaccine
Olivera et al. BMC Health Services Research (2020) 20:295 https://doi.org/10.1186/s12913-020-05115-7 RESEARCH ARTICLE Open Access Valuing the cost of improving Chilean primary vaccination: a cost minimization analysis of a hexavalent vaccine Ignacio Olivera1, Carlos Grau1, Hugo Dibarboure2, Juan Pablo Torres3, Gustavo Mieres1, Luis Lazarov1, Fabián P. Alvarez4 and Juan Guillermo López Yescas5* Abstract Background: The phased withdrawal of oral polio vaccine (OPV) and the introduction of inactivated poliovirus vaccine (IPV) is central to the polio ‘end-game’ strategy. Methods: We analyzed the cost implications in Chile of a switch from the vaccination scheme consisting of a pentavalent vaccine with whole-cell pertussis component (wP) plus IPV/OPV vaccines to a scheme with a hexavalent vaccine with acellular pertussis component (aP) and IPV (Hexaxim®) from a societal perspective. Cost data were collected from a variety of sources including national estimates and previous vaccine studies. All costs were expressed in 2017 prices (US$ 1.00 = $Ch 666.26). Results: The overall costs associated with the vaccination scheme (4 doses of pentavalent vaccine plus 1 dose IPV and 3 doses OPV) from a societal perspective was estimated to be US$ 12.70 million, of which US$ 8.84 million were associated with the management of adverse events related to wP. In comparison, the cost associated with the 4-dose scheme with a hexavalent vaccine (based upon the PAHO reference price) was US$ 19.76 million. The cost of switching to the hexavalent vaccine would be an additional US$ 6.45 million. Overall, depending on the scenario, the costs of switching to the hexavalent scheme would range from an additional US$ 2.62 million to US$ 6.45 million compared with the current vaccination scheme. -

(ACIP) General Best Guidance for Immunization
9. Special Situations Updates Major revisions to this section of the best practices guidance include the timing of intramuscular administration and the timing of clotting factor deficiency replacement. Concurrent Administration of Antimicrobial Agents and Vaccines With a few exceptions, use of an antimicrobial agent does not interfere with the effectiveness of vaccination. Antibacterial agents have no effect on inactivated, recombinant subunit, or polysaccharide vaccines or toxoids. They also have no effect on response to live, attenuated vaccines, except BCG vaccines. Antimicrobial or immunosuppressive agents may interfere with the immune response to BCG and should only be used under medical supervision (for additional information, see www.merck.com/product/usa/pi_circulars/b/bcg/bcg_pi.pdf). Antiviral drugs used for treatment or prophylaxis of influenza virus infections have no effect on the response to inactivated influenza vaccine (2). However, live, attenuated influenza vaccine should not be administered until 48 hours after cessation of therapy with antiviral influenza drugs. If feasible, to avoid possible reduction in vaccine effectiveness, antiviral medication should not be administered for 14 days after LAIV administration (2). If influenza antiviral medications are administered within 2 weeks after receipt of LAIV, the LAIV dose should be repeated 48 or more hours after the last dose of zanamavir or oseltamivir. The LAIV dose should be repeated 5 days after peramivir and 17 days after baloxavir. Alternatively, persons receiving antiviral drugs within the period 2 days before to 14 days after vaccination with LAIV may be revaccinated with another approved vaccine formulation (e.g., IIV or recombinant influenza vaccine). Antiviral drugs active against herpesviruses (e.g., acyclovir or valacyclovir) might reduce the efficacy of vaccines containing live, attenuated varicella zoster virus (i.e., Varivax and ProQuad) (3,4). -

SARS-Cov-2 RBD219-N1C1 Was Diluted in 20 Mm Tris, 150 Mm Nacl, Ph 7.5 (TBS Buffer) Before
bioRxiv preprint doi: https://doi.org/10.1101/2020.11.04.367359; this version posted November 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Title Page SARS‑CoV-2 RBD219-N1C1: A Yeast-Expressed SARS-CoV-2 Recombinant Receptor-Binding Domain Candidate Vaccine Stimulates Virus Neutralizing Antibodies and T-cell Immunity in Mice 1 2 3 Jeroen Pollet1,2, Wen-Hsiang Chen1,2, Leroy Versteeg1, Brian Keegan1, Bin Zhan1,2, Junfei 4 Wei1, Zhuyun Liu1, Jungsoon Lee1, Rahki Kundu1, Rakesh Adhikari1, Cristina Poveda1, 5 Maria-Jose Villar Mondragon1, Ana Carolina de Araujo Leao1, Joanne Altieri Rivera1, Portia 6 M. Gillespie1, Ulrich Strych1,2, Peter J. Hotez1,2,3,4,*, Maria Elena Bottazzi1,2,3* 7 1 Texas Children’s Hospital Center for Vaccine Development, Houston, TX, USA 8 2 Departments of Pediatrics and Molecular Virology & Microbiology, National School of Tropical 9 Medicine, Baylor College of Medicine, Houston, TX, USA 10 3 Department of Biology, Baylor University, Waco, TX, USA 11 4 James A. Baker III Institute for Public Policy, Rice University, Houston, TX, USA 12 * Correspondence: 13 Corresponding Authors 14 [email protected]; [email protected] 15 16 bioRxiv preprint doi: https://doi.org/10.1101/2020.11.04.367359; this version posted November 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Yeast-expressed SARS-CoV-2 RBD 17 Abstract 18 There is an urgent need for an accessible and low-cost COVID-19 vaccine suitable for low- and 19 middle-income countries. -

For Schools and Parents: K-12 Immunization Requirements
FOR SCHOOLS AND PARENTS: K-12 IMMUNIZATION REQUIREMENTS NJ Department of Health (NJDOH) Vaccine Preventable Disease Program Summary of NJ School Immunization Requirements Listed in the chart below are the minimum required number of doses your child must have to attend a NJ school.* This is strictly a summary document. Exceptions to these requirements (i.e. provisional admission, grace periods, and exemptions) are specified in the Immunization of Pupils in School rules, New Jersey Administrative Code (N.J.A.C. 8:57-4). Please reference the administrative rules for more details https://www.nj.gov/health/cd/imm_requirements/acode/. Additional vaccines are recommended by Advisory Committee on Immunization Practices (ACIP) for optimal protection. For the complete ACIP Recommended Immunization Schedule, please visit http://www.cdc.gov/vaccines/schedules/index.html. Minimum Number of Doses for Each Vaccine Grade/level child DTaP Polio MMR Varicella Hepatitis Meningococcal Tdap enters school: Diphtheria, Tetanus, acellular Pertussis Inactivated (Measles, (Chickenpox) B (Tetanus, Polio Vaccine Mumps, diphtheria, (IPV) Rubella) acellular pertussis) § | Kindergarten – A total of 4 doses with one of these doses A total of 3 2 doses 1 dose 3 doses None None 1st grade on or after the 4th birthday doses with one OR any 5 doses† of these doses given on or after the 4th birthday ‡ OR any 4 doses nd th † 2 – 5 grade 3 doses 3 doses 2 doses 1 dose 3 doses None See footnote NOTE: Children 7 years of age and older, who have not been previously vaccinated with the primary DTaP series, should receive 3 doses of Td. -

Gamma-Irradiated SARS-Cov-2 Vaccine Candidate, OZG-38.61.3, Confers Protection from SARS-Cov-2 Challenge in Human ACEII-Transgen
www.nature.com/scientificreports OPEN Gamma‑irradiated SARS‑CoV‑2 vaccine candidate, OZG‑38.61.3, confers protection from SARS‑CoV‑2 challenge in human ACEII‑transgenic mice Raife Dilek Turan1,2,19, Cihan Tastan1,3,4,19*, Derya Dilek Kancagi1,19, Bulut Yurtsever1,19, Gozde Sir Karakus1,19, Samed Ozer5, Selen Abanuz1,6, Didem Cakirsoy1,8, Gamze Tumentemur7, Sevda Demir2, Utku Seyis1, Recai Kuzay1, Muhammer Elek1,2, Miyase Ezgi Kocaoglu1, Gurcan Ertop7, Serap Arbak9, Merve Acikel Elmas9, Cansu Hemsinlioglu1, Ozden Hatirnaz Ng10, Sezer Akyoney10,11, Ilayda Sahin8,12, Cavit Kerem Kayhan13, Fatma Tokat14, Gurler Akpinar15, Murat Kasap15, Ayse Sesin Kocagoz16, Ugur Ozbek12, Dilek Telci2, Fikrettin Sahin2, Koray Yalcin1,17, Siret Ratip18, Umit Ince14 & Ercument Ovali1 The SARS‑CoV‑2 virus caused the most severe pandemic around the world, and vaccine development for urgent use became a crucial issue. Inactivated virus formulated vaccines such as Hepatitis A and smallpox proved to be reliable approaches for immunization for prolonged periods. In this study, a gamma‑irradiated inactivated virus vaccine does not require an extra purifcation process, unlike the chemically inactivated vaccines. Hence, the novelty of our vaccine candidate (OZG‑38.61.3) is that it is a non‑adjuvant added, gamma‑irradiated, and intradermally applied inactive viral vaccine. Efciency and safety dose (either 1013 or 1014 viral RNA copy per dose) of OZG‑38.61.3 was initially determined in BALB/c mice. This was followed by testing the immunogenicity and protective efcacy of the vaccine. Human ACE2‑encoding transgenic mice were immunized and then infected with the SARS‑CoV‑2 virus for the challenge test. -

Frequently Asked Questions About Measles Immunizations
Immunization Unit Assessment, Compliance, and Evaluation Group Measles FAQs Q: When did the vaccine for measles become available? A: The first measles vaccines were available in 1963, and were replaced with a much better vaccine in 1968. Q: Do people who received MMR in the 1960s need to have their dose repeated? A: Not necessarily. People who have documentation of receiving a live measles vaccine in the 1960s do not need to be revaccinated. People who were vaccinated with a killed or inactivated measles vaccine, or vaccine of unknown type, should be revaccinated with at least 1 dose of MMR. Q: What kind of vaccine is it? A: The vaccines available in the United States that protect against measles are the MMR and MMRV, which protects against measles, mumps, and rubella or measles, mumps, rubella, and varicella (chickenpox). They are both live attenuated, or weakened, vaccines. Q: Which vaccine can I get, the MMR or the MMRV? A: The MMRV is only approved for people aged 12 months – 12 years. The MMR is approved for anyone 6 months of age and older, but it is routinely recommended for use in people 12 months of age and older. Any dose of MMR received before 12 months of age is not considered valid and should be repeated in 4 weeks or at age 12 months, whichever is later. Q: How is the vaccine given? A: The vaccine is administered in the fatty layer of tissue underneath the skin. Q: Is the measles shot just a one-time dose? A: The measles vaccine is very effective. -

The Hepatitis B Vaccine Is the Most Widely Used Vaccine in the World, with Over 1 Billion Doses Given
Hepatitis B Vaccine Protect Yourself and Those You Love What is Hepatitis B? Hepatitis B is the most common serious liver infection in the world. It is caused by the hepatitis B virus (HBV), which attacks liver cells and can lead to liver failure, cirrhosis (scarring), or liver cancer later in life. The virus is transmitted through direct contact with infected blood and bodily fluids, and from an infected woman to her newborn at birth. Is there a safe vaccine for hepatitis B? YES! The good news is that there is a safe and effective vaccine for hepatitis B. The vaccine is a series, typically given as three shots over a six-month period that will provide a lifetime of protection. You cannot get hepatitis B from the vaccine – there is no human blood or live virus in the vaccine. The hepatitis B vaccine is the most widely used vaccine in the world, with over 1 billion doses given. The hepatitis B vaccine is the first "anti-cancer" vaccine because it can help prevent liver cancer! Who should be vaccinated against hepatitis B? The World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) recommend the hepatitis B vaccine for all newborns and children up to 18 years of age, and all high-risk adults. All infants should receive the first dose of the vaccine in the delivery room or in the first 24 hours of life, preferably within 12 hours. (CDC recommends the first dose within 12 hours vs. the WHO recommendation of 24 hours.) The HBV vaccine is recommended to anyone who is at high risk of infection. -

(ACIP) General Best Guidance for Immunization
8. Altered Immunocompetence Updates This section incorporates general content from the Infectious Diseases Society of America policy statement, 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host (1), to which CDC provided input in November 2011. The evidence supporting this guidance is based on expert opinion and arrived at by consensus. General Principles Altered immunocompetence, a term often used synonymously with immunosuppression, immunodeficiency, and immunocompromise, can be classified as primary or secondary. Primary immunodeficiencies generally are inherited and include conditions defined by an inherent absence or quantitative deficiency of cellular, humoral, or both components that provide immunity. Examples include congenital immunodeficiency diseases such as X- linked agammaglobulinemia, SCID, and chronic granulomatous disease. Secondary immunodeficiency is acquired and is defined by loss or qualitative deficiency in cellular or humoral immune components that occurs as a result of a disease process or its therapy. Examples of secondary immunodeficiency include HIV infection, hematopoietic malignancies, treatment with radiation, and treatment with immunosuppressive drugs. The degree to which immunosuppressive drugs cause clinically significant immunodeficiency generally is dose related and varies by drug. Primary and secondary immunodeficiencies might include a combination of deficits in both cellular and humoral immunity. Certain conditions like asplenia and chronic renal disease also can cause altered immunocompetence. Determination of altered immunocompetence is important to the vaccine provider because incidence or severity of some vaccine-preventable diseases is higher in persons with altered immunocompetence; therefore, certain vaccines (e.g., inactivated influenza vaccine, pneumococcal vaccines) are recommended specifically for persons with these diseases (2,3). Administration of live vaccines might need to be deferred until immune function has improved. -
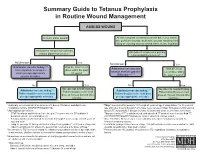
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -
Information and Communication Guide on Vaccines
Module 2 EUROPEAN NURSE Information and Communication Guide ON VACCINES The European Specialist Nurses Organisation (ESNO) is a non-profit organisation with the goal to facilitate and provide an effective framework for communication and co-operation between the European Specialist Nurses Organisations and its constituent members. ESNO represents the mutual interests and benefits of these organisations to the wider European community in the interest of the public health. Members of ESNO consist of individual European specialist nurses member organizations and associates, both institutional and individual. The organisation focusses on enhancing the capacity and capability of specialists nurses to deliver hight quality healthcare by raising and harmonise specialist nursing education standards and actively contribute to health themes and threats, providing the best possible expertise, both national and in European cross border context. A publication from the European Specialist Nurses Organisation April 2021 - www.esno.org Copyright: ©2021 European Specialist Nurses Organisation. All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. CONTENTS Vaccination 1 Introduction 5 2 Principles of vaccination 6 2.1 Principle -

Vaccines 101 the Very Last Day That I Was a Pediatric Resident. Um, Many
Vaccines 101 The very last day that I was a pediatric resident. Um, many years ago, a toddler walked into the emergency room and uh, and progressively got sicker and sicker. That's Dr. Katherine Edwards, a world expert in pediatric infectious disease in vaccinology. She's also a professor of pediatrics at Vanderbilt university and she's been working on vaccines for 40 years. I did a spinal tap on her and realized that she had Haemophilus influenza, typ e B meningitis, Haemophilus influenza, type B or HIB is it bacteria normally found in our nose and throat that can lead to very serious life threatening infections and no matter what I did in that day and into the night in terms of prompt antibiotics and she'd just been sick a few hours and, and fluids and all the, you know, ventilators and all the best things that modern medicine, she died, the vaccine for hip was not available until the 1990s. And until it did become available, hip disease affected approximately 25,000 children each year with things like meningitis, pneumonia, and bloodstream infections. And at that time in the hospital that I was practicing at any one time, there were generally five or six patients that had Haemophilus meningitis or invasive disease or some complication of this particular infection. And we knew that from the basic science that if you had antibody to the capsule or to the coat of the organism, that you were protected from disease. But we really didn't know how to make little kids make antibody.