Vaccines 101 the Very Last Day That I Was a Pediatric Resident. Um, Many
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
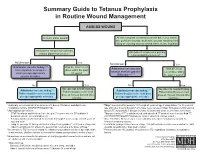
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -
Information and Communication Guide on Vaccines
Module 2 EUROPEAN NURSE Information and Communication Guide ON VACCINES The European Specialist Nurses Organisation (ESNO) is a non-profit organisation with the goal to facilitate and provide an effective framework for communication and co-operation between the European Specialist Nurses Organisations and its constituent members. ESNO represents the mutual interests and benefits of these organisations to the wider European community in the interest of the public health. Members of ESNO consist of individual European specialist nurses member organizations and associates, both institutional and individual. The organisation focusses on enhancing the capacity and capability of specialists nurses to deliver hight quality healthcare by raising and harmonise specialist nursing education standards and actively contribute to health themes and threats, providing the best possible expertise, both national and in European cross border context. A publication from the European Specialist Nurses Organisation April 2021 - www.esno.org Copyright: ©2021 European Specialist Nurses Organisation. All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. CONTENTS Vaccination 1 Introduction 5 2 Principles of vaccination 6 2.1 Principle -

Bcch 2019-20 Flu Vaccine – Oncology Clinic
BCCH 2019-20 FLU VACCINE – ONCOLOGY CLINIC We are providing influenza vaccines for patients who are on therapy and have platelets > 50,000 and ANC over 0.5 (and expected to stay above 0.5 for the next 48 hours, in order to minimize risk of admission in case of fever). Please do not schedule appointments for flu shots only. Please advise the family that immunization of all family members is recommended. The Oncology Outpatient Clinic is not providing immunizations for family members or for those patients who are OFF therapy. Flu shots can be given by family doctors to patients and their families, or they can get a flu shot at the BCCH drop-in Family Immunization clinic in the Ambulatory Care Building, across from the Ambulatory Care Pharmacy on week days in the fall months. Pediatric oncology patients can also get a flu shot at almost any community pharmacy at no cost as they are considered “at risk.” Age Dose** Doses required 6 months – 9 years 0.5 mL IM 1 or 2* > 9 years 0.5 mL IM 1 Less than 6 months Not recommended *Two doses administered at least 4 weeks apart are recommended for children under 9 years of age who are receiving influenza vaccine for the first time. **The recommended site of vaccination is the deltoid muscle for adults and older children. The preferred site for infants and young children is the anterolateral aspect of the thigh. Contraindications: • Febrile illness • Thimerosal sensitivity Special considerations: • Egg allergic individuals (including those who have experienced anaphylaxis following egg ingestion) can be immunized with inactivated influenza vaccine (such as Flulaval tetra) • Thimerosal allergic patients should be vaccinated using Agriflu which can be obtained from local public health units, (but not in the oncology clinic). -

Vaccine Hesitancy
Vaccine Hesitancy Dr Brenda Corcoran National Immunisation Office Presentation Outline An understanding of the following principles: • Overview of immunity • Different types of vaccines and vaccine contents • Vaccine failures • Time intervals between vaccine doses • Vaccine overload • Adverse reactions • Herd immunity Immunity Immunity • The ability of the human body to protect itself from infectious disease The immune system • Cells with a protective function in the – bone marrow – thymus – lymphatic system of ducts and nodes – spleen –blood Types of immunity Source: http://en.wikipedia.org/wiki/Immunological_memory Natural (innate) immunity Non-specific mechanisms – Physical barriers • skin and mucous membranes – Chemical barriers • gastric and digestive enzymes – Cellular and protein secretions • phagocytes, macrophages, complement system ** No “memory” of protection exists afterwards ** Passive immunity – adaptive mechanisms Natural • maternal transfer of antibodies to infant via placenta Artificial • administration of pre- formed substance to provide immediate but short-term protection (antitoxin, antibodies) Protection is temporary and wanes with time (usually few months) Active immunity – adaptive mechanisms Natural • following contact with organism Artificial • administration of agent to stimulate immune response (immunisation) Acquired through contact with an micro-organism Protection produced by individual’s own immune system Protection often life-long but may need boosting How vaccines work • Induce active immunity – Immunity and immunologic memory similar to natural infection but without risk of disease • Immunological memory allows – Rapid recognition and response to pathogen – Prevent or modify effect of disease Live attenuated vaccines Weakened viruses /bacteria – Achieved by growing numerous generations in laboratory – Produces long lasting immune response after one or two doses – Stimulates immune system to react as it does to natural infection – Can cause mild form of the disease (e.g. -

HIV Vaccine Development Dr. Patricia Fast 1
HIV Vaccine Development Dr. Patricia Fast HIV Vaccine Development Dr. Patricia Fast (MD, PhD) Senior Technical Advisor, International AIDS Vaccine Initiative Adjunct Clinical Associate Professor, Infectious Disease, Pediatrics Stanford University School of Medicine How It Began 1984 • Human Immunodeficiency Virus (HIV-1) discovered as the cause of AIDS • Prediction: a vaccine will soon be developed! Non-Human Primate Models Focusing on this dominant model • Simian Immunodeficiency Virus (SIV) lead to a bias – SIV Mac 239 causes AIDS-like disease in Macaques almost impossible to neutralize • SHIV hybrid (with HIV Envelope) allows research into neutralizing antibodies in macaques • Chimpanzees can be infected by HIV, but seldom get AIDS False starts • Traditional vaccine approaches fail in NHP model . Killed SIV does not really protect against SIV o Initial positive result was an artifact . Live attenuated SIV protects, but is not safe o Attenuated vaccine was shown to regain virulence The screen versions of these slides have full details of copyright and acknowledgements 1 HIV Vaccine Development Dr. Patricia Fast How would an AIDS vaccine work? A note about virus biology • HIV has many mechanisms to escape immune recognition e.g. : . Rapid formation of variation . Structural aspects How would an AIDS vaccine work? Immune Mechanisms • T cells . Kill virus-infected cells . Slow down or stop replication of viruses within cells . Can directly kill virus infected cells . Secrete substances that block viral replication Can neutralize virus when they prevent entry; by binding viral envelope protein or the cellular receptors HIV is extremely variable Europe and North America East Africa Southern Africa, India and China Part of an HIV phylogenetic tree The screen versions of these slides have full details of copyright and acknowledgements 2 HIV Vaccine Development Dr. -

The Challenge of Achieving Universal Access to Vaccines
Keynote Address: The Challenge of Achieving Universal Access to Vaccines WIPO & AMF Seth Berkley M.D, CEO 8 November 2017 www.gavi.org 1 Vaccine landscape WIPO 8 November 2017 The world before vaccines Examples of major disease outbreaks Polio Cholera New York pandemic 1916 Europe 6,000 deaths 1829-1851 >200,000 deaths Yellow fever Philadelphia Smallpox 1793 epidemic >5,000 India deaths 1974 15,000 deaths Flu pandemic 1918-1920 > 50-100 million deaths worldwide WIPO 8 November 2017 History of vaccine development Source: Delaney et.al. 2014 WIPO 8 November 2017 Cumulative number of vaccines developed licensed 50+ vaccines Lyme OspA, protein (1998) Tuberculosis (Bacille Calmette-Guérin) Pneumococcal conjugate, heptavalent* (2000) 1927 Typhus Varicella (1995) Meningococcal quadrivalent conjugates* (2005) Japanese encephalitis (Vera-cell) (2009) 1938 Cholera (recombinant Toxin B) # (1993) Cholera (WC only) (2009) Tetanus toxoid Cholera (WC-rBC) (1991) Human papillomavirus recombinant bivalent (2009) Influenza H. influenzaeconjugate* (1987) Quadrivalent influenza vaccines (2012) Typhoid Cholera Pertussis 1936 Meningococcal C and Y and 1886 1896 1926 H. influenza type B polysaccharide (1985) Haemophilusinfluenza type b (2012) Adenovirus (1980) Meningococcal B (2013) Smallpox Diphtheria Yellow Rabies, cell culture (1980) Influenza vaccine (baculovirus) (2013) 1798 toxoid Fever Typhoid conjugate vaccine (2013) Rabies Plague Meningococcal polysaccharides (1974) 1923 1935 Human papillomavirus, 9-valent (2014) 1885 Rubella, live (1969) 1897 vaccines -

Package Inserts
Individuals using assistive technology may not be able to fully access the information contained in this file. For assistance, please send an e-mail to: [email protected] and include 508 Accommodation and the title of the document in the subject line of your e-mail. HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use • Carefully consider benefits and risks before administering VAXELIS to VAXELIS safely and effectively. See full prescribing information for persons with a history of: VAXELIS. - fever ≥40.5°C (≥105°F), hypotonic-hyporesponsive episode (HHE) or VAXELISTM (Diphtheria and Tetanus Toxoids and Acellular Pertussis, persistent, inconsolable crying lasting ≥3 hours within 48 hours after a Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B previous pertussis-containing vaccine. (5.2) Vaccine) - seizures within 3 days after a previous pertussis-containing vaccine. (5.2) Suspension for Intramuscular Injection Initial U.S. Approval: 2018 • If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome ----------------------------RECENT MAJOR CHANGES ------------------------ may be increased following VAXELIS. (5.3) Dosage and Administration (2.2) 09/2020 • Apnea following intramuscular vaccination has been observed in some ----------------------------INDICATIONS AND USAGE--------------------------- infants born prematurely. The decision about when to administer an VAXELIS is a vaccine indicated for active immunization to prevent intramuscular vaccine, including VAXELIS, to an infant born prematurely diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease should be based on consideration of the individual infant’s medical status due to Haemophilus influenzae type b. -

Evaluation of the First Five Years of GAVI Immunization Services Support Funding
Cambridge, MA Lexington, MA Evaluation of the Hadley, MA First Five Years of Bethesda, MD Chicago, IL GAVI Immunization Services Support Funding Prepared for The GAVI Alliance Grace Chee Abt Associates Inc. Natasha Hsi Abt Associates Inc. Kenneth Carlson Abt Associates Inc. Slavea Chankova Abt Associates Inc. Patricia Taylor John Snow, Inc. September 2007 Evaluation of the First Five Years’ of GAVI Immunization Services Support Funding is a publication of Abt Associates, commissioned by the GAVI Alliance. The opinions expressed herein are those of the authors and do not necessarily reflect the views of Abt Associates, the GAVI Alliance or any of its alliance partners. September 2007 Recommended Citation Grace Chee, Natasha Hsi, Kenneth Carlson, Slavea Chankova, Patricia Taylor. September 2007. Evaluation of the First Five Years’ of GAVI Immunization Services Support Funding. Bethesda, MD: Abt Associates Inc. CONTENTS Acronyms....................................................................................................................................... v Acknowledgements...................................................................................................................... vii Executive Summary ...................................................................................................................... ix 1. Background to the Study........................................................................................................ 1 2. Approach and Methods ......................................................................................................... -

Humanized Mice for Live-Attenuated Vaccine Research: from Unmet Potential to New Promises
Review Humanized Mice for Live-Attenuated Vaccine Research: From Unmet Potential to New Promises Aoife K. O’Connell and Florian Douam * Department of Microbiology, National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, Boston, MA 02118, USA; [email protected] * Correspondence: [email protected] Received: 21 December 2019; Accepted: 13 January 2020; Published: 21 January 2020 Abstract: Live-attenuated vaccines (LAV) represent one of the most important medical innovations in human history. In the past three centuries, LAV have saved hundreds of millions of lives, and will continue to do so for many decades to come. Interestingly, the most successful LAVs, such as the smallpox vaccine, the measles vaccine, and the yellow fever vaccine, have been isolated and/or developed in a purely empirical manner without any understanding of the immunological mechanisms they trigger. Today, the mechanisms governing potent LAV immunogenicity and long-term induced protective immunity continue to be elusive, and therefore hamper the rational design of innovative vaccine strategies. A serious roadblock to understanding LAV-induced immunity has been the lack of suitable and cost-effective animal models that can accurately mimic human immune responses. In the last two decades, human-immune system mice (HIS mice), i.e., mice engrafted with components of the human immune system, have been instrumental in investigating the life-cycle and immune responses to multiple human-tropic pathogens. However, their use in LAV research has remained limited. Here, we discuss the strong potential of LAVs as tools to enhance our understanding of human immunity and review the past, current and future contributions of HIS mice to this endeavor. -

Influenza Whoinsert Generic Name As on 080710
capacity. Healthcare providers need to assess the benefit and potential risks of administering the vaccine to pregnant women. It is not known whether Influenza Vaccine(Human,Live Attenuated) is excreted in human milk. Therefore, as some viruses are Influenza Vaccine excreted in human milk and additionally, because of the possibility of shedding of vaccine virus and the close proximity of a nursing infant and mother, caution should be exercised if Influenza Vaccine(Human,Live Attenuated) is administered to nursing Sii mothers. (Human, Live Attenuated) Effects on ability to drive and use machines The vaccine is unlikely to produce an effect on the ability to drive and use machines. Pandemic (H1N1) (Freeze-Dried) ADVERSE REACTIONS In clinical trials a few local and systemic reaction were observed. They were mild to moderate in severity and resolved without DESCRIPTION any sequelae. Influenza Vaccine(Human,Live Attenuated) Pandemic (H1N1), freeze dried is a live monovalent vaccine for administration by Local : Nasal discomfort, stuffy nose, sneezing, runny nose, loss of smell red eyes, lacrimation, facial swelling. intranasal spray. The influenza vaccine contains Influenza virus cultivated on embryonated eggs. Systemic : Headache, fatigue, myalgia, arthralgia, irritability, loss of appetite, sore throat, cough, diarrhoea. The incidence was similar in both the study groups. COMPOSITION There were a few unsolicited event reported in both the groups and none of them were causally related to study vaccines. [Propagated in Embryonated hen eggs (SPF)] Each single dose of 0.5 ml contains: 7 OVERDOSE A/17/California/2009/38 > 10 EID50 No case of overdose has been reported. Gelatin (Partially hydrolyzed) 2.5%, Sorbitol 5%, L-Alanine 0.1% L-Histidine 0.21%, Tricine 0.3%, L-Arginine hydrochloride 1.6% Lactalbumin hydrolysate 0.35%, Phosphate buffer saline Base PHARMACOLOGICAL PROPERTIES Reconstitute with Sterile Water for Inhalation USP. -

An Oral Live Attenuated Vaccine Strategy Against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Cov-2/2019-Ncov)
Research Ideas and Outcomes 6: e53767 doi: 10.3897/rio.6.e53767 Research Idea An oral live attenuated vaccine strategy against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2/2019-nCoV) Madhusudana Girija Sanal‡, Ravi Chandra Dubey§ ‡ Institute of Liver and Biliary Sciences, New Delhi, India § South Asian University, New Delhi, India Corresponding author: Madhusudana Girija Sanal ([email protected]) Reviewed v1 Received: 29 Apr 2020 | Published: 13 May 2020 Citation: Sanal MG, Dubey RC (2020) An oral live attenuated vaccine strategy against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2/2019-nCoV). Research Ideas and Outcomes 6: e53767. https://doi.org/10.3897/rio.6.e53767 Abstract Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2/2019-nCoV) infection has become a pandemic called COVID-19. The virus binds to angiotensin converting enzyme 2 (ACE2) and TMPRSS2 which are abundantly expressed on various human cells including lung epithelial cells and intestinal cells and the virus can infect these cells. Currently no specific treatments or vaccines are available for this disease. A per oral live attenuated vaccine can be a good strategy in SARS-CoV-2 infection because the attenuated virus initially infects the gut, stimulates the mucosa associated immune system sparing the respiratory system during the initial immune response. The live virus can also spread in the community boosting herd immunity. Keywords Oral Live Attenuated Vaccine, Severe Acute Respiratory Syndrome Coronavirus 2/SARS- CoV-2/2019-nCoV, Angiotensin Converting Enzyme-2 (ACE2), Gut Infection, Proximal and Distal Enterocytes, Herd Immunity © Sanal M, Dubey R. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -

Guidelines for Vaccination of Adult Solid Organ Transplant Candidates and Recipients
Stanford Healthcare Vaccination Subcommittee Issue Date: 7/2018 Guidelines for Vaccination of Adult Solid Organ Transplant Candidates and Recipients A. General considerations regarding vaccination 1. Adult solid organ transplant (SOT) candidates and recipients should receive all vaccines indicated based on their ages, medical conditions, and other factors that apply to non- SOT candidates or recipients (see http://www.cdc.gov/vaccines/schedules/hcp/adult.html, Appendix A, and Appendix B) except for the below-listed exceptions or additions. • All SOT candidates and recipients should be vaccinated against pneumococcus with PCV13 and PPSV23. • All SOT candidates and recipients should receive a HepB vaccine series with post-vaccination titers unless they have a documented anti-HBs titer of ≥ 10 mIU/mL after a properly-timed HepB series or unless they have known hepatitis B virus infection. • All SOT candidates and recipients should receive a HepA vaccine series unless previously administered or unless they have a positive hepatitis A virus immunoglobulin G assay. • Live-attenuated vaccines1 should not be administered to SOT recipients, SOT candidates on immunosuppression, or SOT candidates who may undergo SOT within 4 weeks. The timing of inactivated, subunit, or toxoid vaccines is discussed below. Vaccine Notes Influenza Can be given pre- and/or post-SOT (see Appendix C) Tdap or Td Can be given pre- and/or post-SOT Live-attenuated vaccine to be given pre-SOT only; generally those born MMR before 1957 (among others) are considered immune