Vaccination and Multiple Sclerosis in the Era of the COVID-19 Pandemic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SARS-Cov-2 RBD219-N1C1 Was Diluted in 20 Mm Tris, 150 Mm Nacl, Ph 7.5 (TBS Buffer) Before
bioRxiv preprint doi: https://doi.org/10.1101/2020.11.04.367359; this version posted November 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Title Page SARS‑CoV-2 RBD219-N1C1: A Yeast-Expressed SARS-CoV-2 Recombinant Receptor-Binding Domain Candidate Vaccine Stimulates Virus Neutralizing Antibodies and T-cell Immunity in Mice 1 2 3 Jeroen Pollet1,2, Wen-Hsiang Chen1,2, Leroy Versteeg1, Brian Keegan1, Bin Zhan1,2, Junfei 4 Wei1, Zhuyun Liu1, Jungsoon Lee1, Rahki Kundu1, Rakesh Adhikari1, Cristina Poveda1, 5 Maria-Jose Villar Mondragon1, Ana Carolina de Araujo Leao1, Joanne Altieri Rivera1, Portia 6 M. Gillespie1, Ulrich Strych1,2, Peter J. Hotez1,2,3,4,*, Maria Elena Bottazzi1,2,3* 7 1 Texas Children’s Hospital Center for Vaccine Development, Houston, TX, USA 8 2 Departments of Pediatrics and Molecular Virology & Microbiology, National School of Tropical 9 Medicine, Baylor College of Medicine, Houston, TX, USA 10 3 Department of Biology, Baylor University, Waco, TX, USA 11 4 James A. Baker III Institute for Public Policy, Rice University, Houston, TX, USA 12 * Correspondence: 13 Corresponding Authors 14 [email protected]; [email protected] 15 16 bioRxiv preprint doi: https://doi.org/10.1101/2020.11.04.367359; this version posted November 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Yeast-expressed SARS-CoV-2 RBD 17 Abstract 18 There is an urgent need for an accessible and low-cost COVID-19 vaccine suitable for low- and 19 middle-income countries. -

Clinical Trial Protocol
PROTOCOL Dok.#: 129K-PMS-MR Page 1 of 55 Reactogenicity and Protectivity Following Measles- Rubella (MR) Routine Immunization in Indonesian Infants and Children Phase IV PMS-MR-0417 CLINICAL TRIAL PROTOCOL Sponsor PT BIO FARMA (PERSERO) Jl. Pasteur No. 28 Bandung – 40161 Indonesia August 2017 The information contained in this document is the property of Bio Farma and is confidential. It may be submitted to a Regulatory Authority, an Institutional Review Board/Ethics Committee, or an Investigator or a Pharmacist for the purpose of assessment in relation to registration of the product or initiation of a clinical trial. Reproduction or disclosure of the information in whole or in part is forbidden without the written consent of Bio Farma. This document must be returned to Bio Farma Versionupon request. 1.0 August 2017 PT Bio Farma PROTOCOL Dok.#: 129K-PMS-MR Page 2 of 55 Reactogenicity and Protectivity Following Measles-Rubella (MR) Routine Immunization in Indonesian Infants and Children PMS-MR-0417 CLINICAL TRIAL PHASE IV (POST MARKETING SURVEILLANCE) Sponsor PT. BIO FARMA (PERSERO) Jl. Pasteur No. 28 Bandung – 40161 INDONESIA Investigational Product Measles-Rubella (MR) Vaccine Manufacturing Sites Serum Institute of India PVT.LTD. 212/2, Hadapsar, Pune 411028, India Principal Investigator Dr. dr. Dominicus Husada, SpA(K) Sub-Investigators dr. Dwiyanti Puspitasari, SpA(K) dr. Leny Kartina, SpA(K) Medical Advisor Prof. Dr.dr. Ismoedijanto, SpA(K) Prof. dr. Parwati S. Basuki, SpA(K) Biometry Dr. dr. Windhu Purnomo, MS Monitors Dr. Novilia Sjafri Bachtiar, dr., M.Kes. Rini Mulia Sari, dr. Julianita Fahmi, dr. Asep Irham Fattahul Qur'an, dr Biological Laboratory Rini Mulia Sari, dr. -
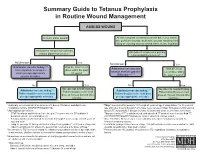
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -

Vaccines 101 the Very Last Day That I Was a Pediatric Resident. Um, Many
Vaccines 101 The very last day that I was a pediatric resident. Um, many years ago, a toddler walked into the emergency room and uh, and progressively got sicker and sicker. That's Dr. Katherine Edwards, a world expert in pediatric infectious disease in vaccinology. She's also a professor of pediatrics at Vanderbilt university and she's been working on vaccines for 40 years. I did a spinal tap on her and realized that she had Haemophilus influenza, typ e B meningitis, Haemophilus influenza, type B or HIB is it bacteria normally found in our nose and throat that can lead to very serious life threatening infections and no matter what I did in that day and into the night in terms of prompt antibiotics and she'd just been sick a few hours and, and fluids and all the, you know, ventilators and all the best things that modern medicine, she died, the vaccine for hip was not available until the 1990s. And until it did become available, hip disease affected approximately 25,000 children each year with things like meningitis, pneumonia, and bloodstream infections. And at that time in the hospital that I was practicing at any one time, there were generally five or six patients that had Haemophilus meningitis or invasive disease or some complication of this particular infection. And we knew that from the basic science that if you had antibody to the capsule or to the coat of the organism, that you were protected from disease. But we really didn't know how to make little kids make antibody. -

Considerations for Causality Assessment of Neurological And
Occasional essay J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2021-326924 on 6 August 2021. Downloaded from Considerations for causality assessment of neurological and neuropsychiatric complications of SARS- CoV-2 vaccines: from cerebral venous sinus thrombosis to functional neurological disorder Matt Butler ,1 Arina Tamborska,2,3 Greta K Wood,2,3 Mark Ellul,4 Rhys H Thomas,5,6 Ian Galea ,7 Sarah Pett,8 Bhagteshwar Singh,3 Tom Solomon,4 Thomas Arthur Pollak,9 Benedict D Michael,2,3 Timothy R Nicholson10 For numbered affiliations see INTRODUCTION More severe potential adverse effects in the open- end of article. The scientific community rapidly responded to label phase of vaccine roll- outs are being collected the COVID-19 pandemic by developing novel through national surveillance systems. In the USA, Correspondence to SARS- CoV-2 vaccines (table 1). As of early June Dr Timothy R Nicholson, King’s roughly 372 adverse events have been reported per College London, London WC2R 2021, an estimated 2 billion doses have been million doses, which is a lower rate than expected 1 2LS, UK; timothy. nicholson@ administered worldwide. Neurological adverse based on the clinical trials.6 kcl. ac. uk events following immunisation (AEFI), such as In the UK, adverse events are reported via the cerebral venous sinus thrombosis and demyelin- MB and AT are joint first Coronavirus Yellow Card reporting website. As of ating episodes, have been reported. In some coun- authors. early June 2021, approximately 250 000 Yellow tries, these have led to the temporary halting of BDM and TRN are joint senior Cards have been submitted, equating to around authors. -

Vaccine Hesitancy
Vaccine Hesitancy Dr Brenda Corcoran National Immunisation Office Presentation Outline An understanding of the following principles: • Overview of immunity • Different types of vaccines and vaccine contents • Vaccine failures • Time intervals between vaccine doses • Vaccine overload • Adverse reactions • Herd immunity Immunity Immunity • The ability of the human body to protect itself from infectious disease The immune system • Cells with a protective function in the – bone marrow – thymus – lymphatic system of ducts and nodes – spleen –blood Types of immunity Source: http://en.wikipedia.org/wiki/Immunological_memory Natural (innate) immunity Non-specific mechanisms – Physical barriers • skin and mucous membranes – Chemical barriers • gastric and digestive enzymes – Cellular and protein secretions • phagocytes, macrophages, complement system ** No “memory” of protection exists afterwards ** Passive immunity – adaptive mechanisms Natural • maternal transfer of antibodies to infant via placenta Artificial • administration of pre- formed substance to provide immediate but short-term protection (antitoxin, antibodies) Protection is temporary and wanes with time (usually few months) Active immunity – adaptive mechanisms Natural • following contact with organism Artificial • administration of agent to stimulate immune response (immunisation) Acquired through contact with an micro-organism Protection produced by individual’s own immune system Protection often life-long but may need boosting How vaccines work • Induce active immunity – Immunity and immunologic memory similar to natural infection but without risk of disease • Immunological memory allows – Rapid recognition and response to pathogen – Prevent or modify effect of disease Live attenuated vaccines Weakened viruses /bacteria – Achieved by growing numerous generations in laboratory – Produces long lasting immune response after one or two doses – Stimulates immune system to react as it does to natural infection – Can cause mild form of the disease (e.g. -

Different Types of COVID-19 Vaccines
Pfizer-BioNTech Help stop the pandemic Type of vaccine: Messenger RNA, or mRNA, a genetic Different Types material that tells your body how to make proteins that by getting vaccinated triggers an immune response inside our bodies of COVID-19 Effectiveness: 95% based on clinical trials Even if you are undocumented Common side effects: Pain and/or swelling in the arm and/or don’t have insurance, you and tiredness, headache, muscle pain, chills, fever, or can get the vaccine—for free. Vaccines: nausea in the body that may last two days Recommended Ages: 16 and older (currently testing the vaccine in kids ages 12-15) Understanding How Dosage: Two shots, 21 days apart They Work Visit VaccinateALL58.com Moderna for the newest information about when and where the vaccine Type of vaccine: Messenger RNA, or mRNA, a genetic will be available to you. material that tells your body how to make proteins that triggers an immune response inside our bodies Sign up at myturn.ca.gov or Effectiveness: 94.1% based on clinical trials call 1-833-422-4255 to find out Common side effects: Pain and/or swelling in the arm if it’s your turn to get vaccinated and and tiredness, headache, muscle pain, chills, fever, or schedule vaccination appointments. nausea in the body that may last two days Recommended Ages: 18 years and older (currently testing the vaccine in kids ages 12-17) Dosage: Two shots, 28 days apart Johnson & Johnson Follow us on social media for more COVID-19 tips and information. Type of vaccine: A viral vector, it uses a harmless version of a different -

Understanding How Vaccines Work
➤ For more information on vaccines, Understanding vaccine-preventable diseases, and vaccine safety: How Vaccines Work http://www.cdc.gov/vaccines/conversations Last reviewed Februar y 2013 Diseases that vaccines prevent can be The body keeps a few T-lymphocytes, called memory cells that go dangerous, or even deadly. Vaccines greatly into action quickly if the body encounters the same germ again. When the familiar antigens are detected, B-lymphocytes produce reduce the risk of infection by working with antibodies to attack them. the body’s natural defenses to safely develop immunity to disease. This fact sheet explains How Vaccines Work how the body fights infection and how Vaccines help develop immunity by imitating an infection. This type of infection, however, does not cause illness, but it does cause vaccines work to protect people by the immune system to produce T-lymphocytes and antibodies. producing immunity. Sometimes, after getting a vaccine, the imitation infection can cause minor symptoms, such as fever. Such minor symptoms are normal and should be expected as the body builds immunity. Once the imitation infection goes away, the body is left with a The Immune System— supply of “memory” T-lymphocytes, as well as B-lymphocytes that The Body’s Defense Against Infection will remember how to fight that disease in the future. However, it To understand how vaccines work, it is helpful to first look at how typically takes a few weeks for the body to produce T-lymphocytes the body fights illness. When germs, such as bacteria or viruses, and B-lymphocytes after vaccination. Therefore, it is possible that invade the body, they attack and multiply. -

The Challenge of Achieving Universal Access to Vaccines
Keynote Address: The Challenge of Achieving Universal Access to Vaccines WIPO & AMF Seth Berkley M.D, CEO 8 November 2017 www.gavi.org 1 Vaccine landscape WIPO 8 November 2017 The world before vaccines Examples of major disease outbreaks Polio Cholera New York pandemic 1916 Europe 6,000 deaths 1829-1851 >200,000 deaths Yellow fever Philadelphia Smallpox 1793 epidemic >5,000 India deaths 1974 15,000 deaths Flu pandemic 1918-1920 > 50-100 million deaths worldwide WIPO 8 November 2017 History of vaccine development Source: Delaney et.al. 2014 WIPO 8 November 2017 Cumulative number of vaccines developed licensed 50+ vaccines Lyme OspA, protein (1998) Tuberculosis (Bacille Calmette-Guérin) Pneumococcal conjugate, heptavalent* (2000) 1927 Typhus Varicella (1995) Meningococcal quadrivalent conjugates* (2005) Japanese encephalitis (Vera-cell) (2009) 1938 Cholera (recombinant Toxin B) # (1993) Cholera (WC only) (2009) Tetanus toxoid Cholera (WC-rBC) (1991) Human papillomavirus recombinant bivalent (2009) Influenza H. influenzaeconjugate* (1987) Quadrivalent influenza vaccines (2012) Typhoid Cholera Pertussis 1936 Meningococcal C and Y and 1886 1896 1926 H. influenza type B polysaccharide (1985) Haemophilusinfluenza type b (2012) Adenovirus (1980) Meningococcal B (2013) Smallpox Diphtheria Yellow Rabies, cell culture (1980) Influenza vaccine (baculovirus) (2013) 1798 toxoid Fever Typhoid conjugate vaccine (2013) Rabies Plague Meningococcal polysaccharides (1974) 1923 1935 Human papillomavirus, 9-valent (2014) 1885 Rubella, live (1969) 1897 vaccines -

Package Inserts
Individuals using assistive technology may not be able to fully access the information contained in this file. For assistance, please send an e-mail to: [email protected] and include 508 Accommodation and the title of the document in the subject line of your e-mail. HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use • Carefully consider benefits and risks before administering VAXELIS to VAXELIS safely and effectively. See full prescribing information for persons with a history of: VAXELIS. - fever ≥40.5°C (≥105°F), hypotonic-hyporesponsive episode (HHE) or VAXELISTM (Diphtheria and Tetanus Toxoids and Acellular Pertussis, persistent, inconsolable crying lasting ≥3 hours within 48 hours after a Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B previous pertussis-containing vaccine. (5.2) Vaccine) - seizures within 3 days after a previous pertussis-containing vaccine. (5.2) Suspension for Intramuscular Injection Initial U.S. Approval: 2018 • If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome ----------------------------RECENT MAJOR CHANGES ------------------------ may be increased following VAXELIS. (5.3) Dosage and Administration (2.2) 09/2020 • Apnea following intramuscular vaccination has been observed in some ----------------------------INDICATIONS AND USAGE--------------------------- infants born prematurely. The decision about when to administer an VAXELIS is a vaccine indicated for active immunization to prevent intramuscular vaccine, including VAXELIS, to an infant born prematurely diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease should be based on consideration of the individual infant’s medical status due to Haemophilus influenzae type b. -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -
Plant-Based COVID-19 Vaccines: Current Status, Design, and Development Strategies of Candidate Vaccines
Review Plant-Based COVID-19 Vaccines: Current Status, Design, and Development Strategies of Candidate Vaccines Puna Maya Maharjan 1 and Sunghwa Choe 2,3,* 1 G+FLAS Life Sciences, 123 Uiryodanji-gil, Osong-eup, Heungdeok-gu, Cheongju-si 28161, Korea; punamaya.maharjan@gflas.com 2 G+FLAS Life Sciences, 38 Nakseongdae-ro, Gwanak-gu, Seoul 08790, Korea 3 School of Biological Sciences, College of Natural Sciences, Seoul National University, Gwanak-gu, Seoul 08826, Korea * Correspondence: [email protected] Abstract: The prevalence of the coronavirus disease 2019 (COVID-19) pandemic in its second year has led to massive global human and economic losses. The high transmission rate and the emergence of diverse SARS-CoV-2 variants demand rapid and effective approaches to preventing the spread, diagnosing on time, and treating affected people. Several COVID-19 vaccines are being developed using different production systems, including plants, which promises the production of cheap, safe, stable, and effective vaccines. The potential of a plant-based system for rapid production at a commercial scale and for a quick response to an infectious disease outbreak has been demonstrated by the marketing of carrot-cell-produced taliglucerase alfa (Elelyso) for Gaucher disease and tobacco- produced monoclonal antibodies (ZMapp) for the 2014 Ebola outbreak. Currently, two plant-based COVID-19 vaccine candidates, coronavirus virus-like particle (CoVLP) and Kentucky Bioprocessing (KBP)-201, are in clinical trials, and many more are in the preclinical stage. Interim phase 2 clinical Citation: Maharjan, P.M.; Choe, S. trial results have revealed the high safety and efficacy of the CoVLP vaccine, with 10 times more Plant-Based COVID-19 Vaccines: neutralizing antibody responses compared to those present in a convalescent patient’s plasma.