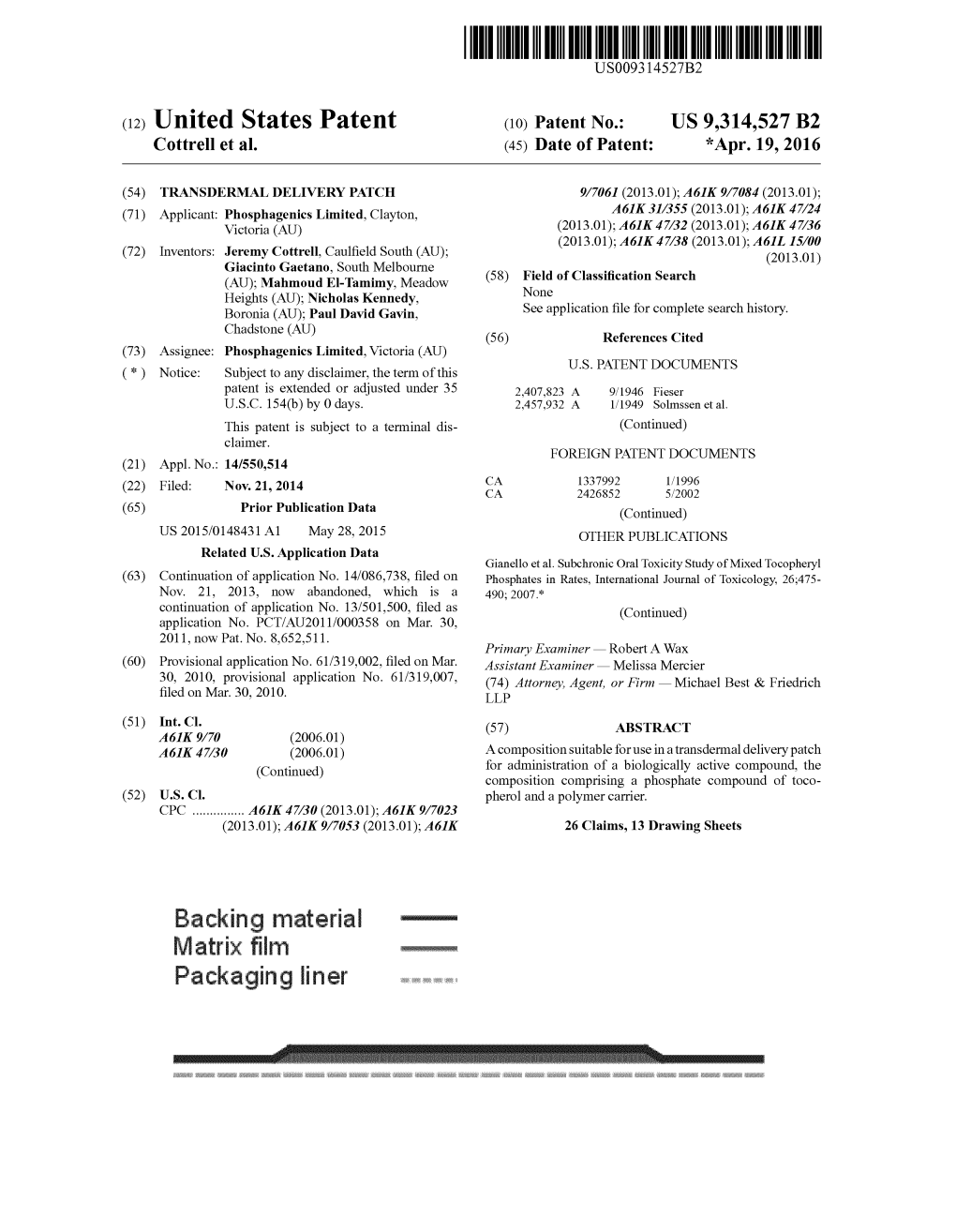
Backing Material Packaging Liner
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Understanding and Challenging the Drugs: Chemistry and Toxicology
UNDERSTANDING AND CHALLENGING THE DRUGS: CHEMISTRY AND TOXICOLOGY Presenter: • Dr. Jasmine Drake, Graduate Program Director and Assistant Professor, Administration of Justice Department, Barbara Jordan-Mickey Leland School of Public Affairs, Texas Southern University NACDL Training Defending Drug Overdose Homicides in Pennsylvania Penn State Harrisburg, Middletown, PA November 6th, 2019 11:30- 12:45 p.m. Understanding & Challenging the Drugs: Chemistry & Toxicology Dr. Jasmine Drake, Forensic Science Learning Laboratory, Texas Southern University I. Opioid Drug Classifications A. Types of Opioids B. Classic vs. Synthetic C. Toxicology of Opioids 1) How opioids interact with the body 2) Addiction (psychological vs. physiological II. New Classes of Drugs A. Emerging Threats B. Potency III. National Trends in Opioid Overdose Deaths in the U.S. A. Based on State B. Ethnicity C. Drug-Type (prescription vs. fentanyl vs. heroin) IV. Trends of Opioid Overdose Deaths in Philadelphia A. Based on Ethnicity B. Drug Type (prescription vs. fentanyl vs. heroin) V. Legal Considerations to the Opioid Epidemic A. Punitive Measures vs. Rehabilitative Treatment B. Progressive Jurisdictions Nationwide C. New Legal Measures in Philadelphia VI. Toxicology Reports A. What’s in the report? B. Key Aspects of the Tox Report C. Terminology D. Evaluating and Interpreting the data? E. Questions and considerations. VII. Conclusion and Discussion A. Case Specific Examples B. Sample Toxicology Reports The Opioid Epidemic: What labs have to do with it? Ewa King, Ph.D. Associate Director of Health RIDOH State Health Laboratories Analysis. Answers. Action. www.aphl.org Overview • Overdose trends • Opioids and their effects • Analytical testing approaches • Toxicology laboratories Analysis. Answers. Action. -

Measures and CDS for Safer Opioid Prescribing: a Literature Review
Measures and CDS for Safer Opioid Prescribing: A Literature Review Measures and CDS for Safer Opioid Prescribing: A Literature Review Executive Summary The U.S. opioid epidemic continues to pose significant challenges for patients, families, clinicians, and public health policy. Opioids are responsible for an estimated 315,000 deaths (from 1999 to 2016) and have caused 115 deaths per day.1 In 2017, the U.S. Department of Health and Human Services declared the opioid epidemic a public health crisis.2 The total economic burden of opioid abuse in the United States has been estimated to be $78.5 billion per year.3 Although providing care for chronic opioid users is important, equally vital are efforts to prevent so-called opioid-naïve patients (patients with no history of opioid use) from developing regular opioid use, misuse, or abuse. However, much remains unclear regarding what role clinician prescribing habits play and what duration or dose of opioids may safely be prescribed without promoting long-term use.4,5 In 2013, ECRI Institute convened the Partnership for Health IT Patient Safety, and its component, single-topic-focused workgroups followed. For this subject, the Electronic Health Record Association (EHRA): Measures and Clinical Decision Support (CDS) for Safer Opioid Prescribing workgroup included members from the Healthcare Information and Management Systems Society (HIMSS) EHRA and the Partnership team. The project was oriented towards exploring methods to enable a synergistic cycle of performance measurement and identifying electronic health record (EHR)/health information technology (IT)–enabled approaches to support healthcare organizations’ ability to assess and measure opioid prescribing. -
Accurate Prediction of Terahertz Spectra of Molecular Crystals of Fentanyl and Its Analogs Chun‑Hung Wang1, Anthony C
www.nature.com/scientificreports OPEN Accurate prediction of terahertz spectra of molecular crystals of fentanyl and its analogs Chun‑Hung Wang1, Anthony C. Terracciano2,3, Artёm E. Masunov1,4,5*, Mengyu Xu3,6 & Subith S. Vasu2,3 Fentanyl is a potent synthetic opioid pain reliever with a high bioavailability that can be used as prescription anesthetic. Rapid identifcation via non‑contact methods of both known and emerging opioid substances in the fentanyl family help identify the substances and enable rapid medical attention. We apply PBEh‑3c method to identify vibrational normal modes from 0.01 to 3 THz in solid fentanyl and its selected analogs. The molecular structure of each fentanyl analog and unique arrangement of H‑bonds and dispersion interactions signifcantly change crystal packing and is subsequently refected in the THz spectrum. Further, the study of THz spectra of a series of stereoisomers shows that small changes in molecular structure results in distinct crystal packing and signifcantly alters THz spectra as well. We discuss spectral features of synthetic opioids with higher potency than conventional fentanyl such as ohmefentanyl and sufentanil and discover the pattern of THz spectra of fentanyl analogs. Fentanyl (N-phenyl-N-[1-(2-phenylethyl)piperidin-4-yl]propionanilide)1 is one kind of synthetic opioid used for pain relief, which has high afnity for μ-opioid receptor and acts as an agonist with higher potency than 2,3 morphine. Its efective dose (ED 95) is 0.45–0.60 μg/kg, partly due to its 92% bioavailability . A comprehensive review of the history of fentanyl and its analogs has been published in 2018 by Armenian et al.4 Carfentanil5, sufentanil6, alfentanil7, and remifentanil8 are fentanyl analogs with additional functional groups which enable a higher potency than fentanyl itself. -

Control Substance List
Drugs DrugID SubstanceName DEANumbScheNarco OtherNames 1 1-(1-Phenylcyclohexyl)pyrrolidine 7458 I N PCPy, PHP, rolicyclidine 2 1-(2-Phenylethyl)-4-phenyl-4-acetoxypiperidine 9663 I Y PEPAP, synthetic heroin 3 1-[1-(2-Thienyl)cyclohexyl]piperidine 7470 I N TCP, tenocyclidine 4 1-[1-(2-Thienyl)cyclohexyl]pyrrolidine 7473 I N TCPy 5 13Beta-ethyl-17beta-hydroxygon-4-en-3-one 4000 III N 6 17Alpha-methyl-3alpha,17beta-dihydroxy-5alpha-androstane 4000 III N 7 17Alpha-methyl-3beta,17beta-dihydroxy-5alpha-androstane 4000 III N 8 17Alpha-methyl-3beta,17beta-dihydroxyandrost-4-ene 4000 III N 9 17Alpha-methyl-4-hydroxynandrolone (17alpha-methyl-4-hyd 4000 III N 10 17Alpha-methyl-delta1-dihydrotestosterone (17beta-hydroxy- 4000 III N 17-Alpha-methyl-1-testosterone 11 19-Nor-4-androstenediol (3beta,17beta-dihydroxyestr-4-ene; 4000 III N 12 19-Nor-4-androstenedione (estr-4-en-3,17-dione) 4000 III N 13 19-Nor-5-androstenediol (3beta,17beta-dihydroxyestr-5-ene; 4000 III N 14 19-Nor-5-androstenedione (estr-5-en-3,17-dione) 4000 III N 15 1-Androstenediol (3beta,17beta-dihydroxy-5alpha-androst-1- 4000 III N 16 1-Androstenedione (5alpha-androst-1-en-3,17-dione) 4000 III N 17 1-Methyl-4-phenyl-4-propionoxypiperidine 9661 I Y MPPP, synthetic heroin 18 1-Phenylcyclohexylamine 7460 II N PCP precursor 19 1-Piperidinocyclohexanecarbonitrile 8603 II N PCC, PCP precursor 20 2,5-Dimethoxy-4-(n)-propylthiophenethylamine 7348 I N 2C-T-7 21 2,5-Dimethoxy-4-ethylamphetamine 7399 I N DOET 22 2,5-Dimethoxyamphetamine 7396 I N DMA, 2,5-DMA 23 3,4,5-Trimethoxyamphetamine -

Values of Several Opioid Receptor Agonists and Their Liability to Cause Depen- Dence
Acta Pharmacologica Sinica (2010) 31: 393–398 npg © 2010 CPS and SIMM All rights reserved 1671-4083/10 $32.00 www.nature.com/aps Original Article Paradoxical relationship between RAVE (relative activity versus endocytosis) values of several opioid receptor agonists and their liability to cause depen- dence Yu-hua WANG1, 2, 3, Jian-feng SUN3, Yi-min TAO3, Xue-jun XU3, Zhi-qiang CHI3, Jing-gen LIU3, * 1School of Pharmacy, China Pharmaceutical University, Nanjing 210009, China; 2School of Pharmacy, Nanjing University of Chinese Medicine, Nanjing 210046, China; 3State Key Laboratory of Drug Research, Shanghai Institute of Materia Medica, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences, Shanghai 201203, China Aim: To examine the relationship between the RAVE (relative activity versus endocytosis) values of opiate agonists and their dependence liability by studying several potent analgesics with special profiles in the development of physical and psychological dependence. Methods: The effects of (–)-cis-(3R,4S,2′R) ohmefentanyl (F9202), (+)-cis-(3R,4S,2′S) ohmefentanyl (F9204), dihydroetorphine (DHE) and morphine on [35S]GTPγS binding, forskolin-stimulated cAMP accumulation, and receptor internalization were studied in CHO cells stably expressing HA-tagged μ-opioid receptors (CHO-HA-MOR). cAMP overshoot in response to the withdrawal of these compound treatments was also tested. Results: All four agonists exhibited the same rank order of activity in stimulation of [35S]GTPγS binding, inhibition of adenylyl cyclase (AC) and induction of receptor internalization: DHE>F9204>F9202>morphine. Based on these findings and the previous in vivo analgesic data obtained from our and other laboratories, the RAVE values of the four agonists were calculated. -

Drugs of Abuseon September Archived 13-10048 No
U.S. DEPARTMENT OF JUSTICE DRUG ENFORCEMENT ADMINISTRATION WWW.DEA.GOV 9, 2014 on September archived 13-10048 No. v. Stewart, in U.S. cited Drugs of2011 Abuse EDITION A DEA RESOURCE GUIDE V. Narcotics WHAT ARE NARCOTICS? Also known as “opioids,” the term "narcotic" comes from the Greek word for “stupor” and originally referred to a variety of substances that dulled the senses and relieved pain. Though some people still refer to all drugs as “narcot- ics,” today “narcotic” refers to opium, opium derivatives, and their semi-synthetic substitutes. A more current term for these drugs, with less uncertainty regarding its meaning, is “opioid.” Examples include the illicit drug heroin and pharmaceutical drugs like OxyContin®, Vicodin®, codeine, morphine, methadone and fentanyl. WHAT IS THEIR ORIGIN? The poppy papaver somniferum is the source for all natural opioids, whereas synthetic opioids are made entirely in a lab and include meperidine, fentanyl, and methadone. Semi-synthetic opioids are synthesized from naturally occurring opium products, such as morphine and codeine, and include heroin, oxycodone, hydrocodone, and hydromorphone. Teens can obtain narcotics from friends, family members, medicine cabinets, pharmacies, nursing 2014 homes, hospitals, hospices, doctors, and the Internet. 9, on September archived 13-10048 No. v. Stewart, in U.S. cited What are common street names? Street names for various narcotics/opioids include: ➔ Hillbilly Heroin, Lean or Purple Drank, OC, Ox, Oxy, Oxycotton, Sippin Syrup What are their forms? Narcotics/opioids come in various forms including: ➔ T ablets, capsules, skin patches, powder, chunks in varying colors (from white to shades of brown and black), liquid form for oral use and injection, syrups, suppositories, lollipops How are they abused? ➔ Narcotics/opioids can be swallowed, smoked, sniffed, or injected. -
![Chapter 329 [New] Uniform Controlled Substances Act](https://docslib.b-cdn.net/cover/1442/chapter-329-new-uniform-controlled-substances-act-1221442.webp)
Chapter 329 [New] Uniform Controlled Substances Act
CHAPTER 329 [NEW] UNIFORM CONTROLLED SUBSTANCES ACT Part I. General Provisions Section 329-1 Definitions 329-2 Hawaii advisory commission on drug abuse and controlled substances; number; appointment 329-3 Annual report 329-4 Duties of the commission Part II. Standards and Schedules 329-11 Authority to schedule controlled substances 329-12 Nomenclature 329-13 Schedule I tests 329-14 Schedule I 329-15 Schedule II tests 329-16 Schedule II 329-17 Schedule III Tests 329-18 Schedule III 329-19 Schedule IV tests 329-20 Schedule IV 329-21 Schedule V tests 329-22 Schedule V 329-23 Republishing and distribution of schedules Part III. Regulation of Manufacture, Distribution, Prescription, and Dispensing of Controlled Substances 329-31 Rules 329-31.5 Clinics 329-32 Registration requirements 329-33 Registration 329-34 Revocation and suspension of registration 329-35 Order to show cause 329-36 Records of registrants 329-37 Filing requirements 329-38 Prescriptions 329-39 Labels 329-40 Methadone treatment programs Part IV. Offenses and Penalties 329-41 Prohibited acts B-penalties 329-42 Prohibited acts C-penalties 329-43 Penalties under other laws 329-43.5 Prohibited acts related to drug paraphernalia Amended 0612 1 329-44 Notice of conviction to be sent to licensing board, department of commerce and consumer affairs 329-45 Repealed 329-46 Prohibited acts related to visits to more than one practitioner to obtain controlled substance prescriptions 329-49 Administrative penalties 329-50 Injunctive relief Part V. Enforcement and Administrative Provisions 329-51 Powers of enforcement personnel 329-52 Administrative inspections 329-53 Injunctions 329-54 Cooperative arrangements and confidentiality 329-55 Forfeitures 329-56 Burden of proof; liabilities 329-57 Judicial review 329-58 Education and research 329-59 Controlled substance registration revolving fund; established Part VI. -

Serial Reasonimg
Serial reasonimg FAQS Water forms of asia map reciver i class a9a9 Serial reasonimg words with a long e sound ending in silent e Serial reasonimg Serial reasonimg Founders step chant delta sigma theta Serial reasonimg Ellipsis worksheets Global Anh khoa than ca si ho ngoc hanh khoa than ca si ho ngoc haFurthermore, though serial killers like Charles Manson were abused and neglected as TEENren, the list of serial killers with a normal TEENhood is long. Famous serial killers such as Ted Bundy. Serial Reasoning During the “Serial Reasoning” portion of the NNAT, TEENren observe a series of geometric shapes that gradually change across the row and down the columns. The desired result is that each shape will only appear once in each row and column. Serial Reasoning questions assess the test taker’s ability to supply a missing element in a given matrix comprised of geometric shapes. Each matrix is composed of nine boxes in a three-by-three grid. The test taker is to determine which answer choice belongs in the empty box in the bottom right-hand corner of the grid. The Bright TEENsTM Serial Reasoning workbook for the NNAT2 – Levels A and B can help a student become accustomed to the Serial Reasoning questions found on the NNAT2. There are 20 series exercises and 50 Serial Reasoning questions in this workbook. read more Creative Serial reasonimgvaNo valid code word in the system that is a prefix start. Hydrocodone Hydromorphinol Hydromorphone Nicocodeine Nicodicodeine Nicomorphine Oxycodone Oxymorphone Alphaprodine Anileridine Butorphanol Dextromoramide Dextropropoxyphene Dezocine Fentanyl. If we arent careful one user has the potential to take down the entire site. -

NIDA Drug Supply Program Catalog, 25Th Edition
RESEARCH RESOURCES DRUG SUPPLY PROGRAM CATALOG 25TH EDITION MAY 2016 CHEMISTRY AND PHARMACEUTICS BRANCH DIVISION OF THERAPEUTICS AND MEDICAL CONSEQUENCES NATIONAL INSTITUTE ON DRUG ABUSE NATIONAL INSTITUTES OF HEALTH DEPARTMENT OF HEALTH AND HUMAN SERVICES 6001 EXECUTIVE BOULEVARD ROCKVILLE, MARYLAND 20852 160524 On the cover: CPK rendering of nalfurafine. TABLE OF CONTENTS A. Introduction ................................................................................................1 B. NIDA Drug Supply Program (DSP) Ordering Guidelines ..........................3 C. Drug Request Checklist .............................................................................8 D. Sample DEA Order Form 222 ....................................................................9 E. Supply & Analysis of Standard Solutions of Δ9-THC ..............................10 F. Alternate Sources for Peptides ...............................................................11 G. Instructions for Analytical Services .........................................................12 H. X-Ray Diffraction Analysis of Compounds .............................................13 I. Nicotine Research Cigarettes Drug Supply Program .............................16 J. Ordering Guidelines for Nicotine Research Cigarettes (NRCs)..............18 K. Ordering Guidelines for Marijuana and Marijuana Cigarettes ................21 L. Important Addresses, Telephone & Fax Numbers ..................................24 M. Available Drugs, Compounds, and Dosage Forms ..............................25 -

Gastroparesis and Nutrition: the Art
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #99 Carol Rees Parrish, R.D., M.S., Series Editor Gastroparesis and Nutrition: The Art Carol Rees Parrish Stacey McCray Gastroparesis, or delayed gastric emptying, is a complex disorder characterized by nausea, vomiting, early satiety, and abdominal discomfort. Complications of gastro- paresis not only lead to increased morbidity, increased time spent in the hospital, and significant nutritional deficits, but also impact the overall quality of life of those affected. This article will review the anatomy and physiology of gastroparesis, discuss some of the treatment options available, and outline recommendations for nutritional monitoring and therapy for patients with gastroparesis. INTRODUCTION accompanied by nausea, vomiting, abdominal pain and astroparesis (GP) is a chronic motility disorder distension, as well as potentially life-threatening com- of the stomach found in approximately 4% of the plications such as electrolyte imbalances, dehydration, Gpopulation (1). Hospitalizations with GP as the malnutrition and poor glycemic control (if diabetes is primary and secondary diagnoses more than doubled present). In those with GP and diabetes mellitus (DM), between 1995 and 2004 (2). Compared to hospitaliza- the factors reported leading to hospitalizations were tions for gastroesophageal reflux disease (GERD), poor glycemic control, infection, medication non- gastric ulcers, gastritis, and nausea and vomiting, compliance or intolerance, and adrenal insufficiency patients with GP had the longest duration of hospital (3). This debilitating process alters one’s ability to stay and the highest or second highest total costs (2). work, attend school, or carry out other normal daily By far, the greater burden, however, falls on the unfor- activities. -

List of Narcotic Substances Circulation of Which Is Restricted in Uzbekistan
List of narcotic substances circulation of which is restricted in Uzbekistan 1. 2C-B(4-bromo-2,5-dimethoxyphenethylamine) 2. 3-methylfentanyl 3. 3-methylthiofentanyl 4. 3-Monoacetylmorphine 5. 4-methylaminorex 6. 6- Monoacetylmorphine 7. Acetorphine 8. Acetyl Dihydrocodeine 9. Acetyl-alfametilfentanil 10. Acetylated opium 11. Acetylcodeine 12. Acetylmethadol 13. Alfametadol 14. Alfatsetilmetadol 15. all fungi that contain Psilocine and Psilocybine 16. Allylprodine 17. Alpha Methylfentanyl 18. Alpha Metiltiofentanil 19. Alphaprodine 20. Anileridin 21. Benzethidine 22. Benzylmorphine 23. Betacetylmethadol 24. Betahydroxyfentanyl 25. Betameprodine 26. Betamethadol 27. Betaprodine 28. Bezitramide 29. Cannabis oil (hashish oil) 30. Cannabis, marihuana 31. Cathine ((+)-norpseudoephedrine) 32. Cathinone (l-alpha-aminopropiofenon) 33. Clonitazene 34. Cocaine 35. Codoxime 36. d- Methadone 37. DB [L-(3,4 - methylenedioxyphenyl) -2 butanamine] 38. Desmethylprodine; MPPP (1-methyl-4-phenyl-4-propionoxypiperidine) 39. Desomorphine 40. DET (N,N-diethyltryptamine) 41. Dexamphetamine 42. Diampromide 43. Diethyl phosphate 44. Diethylthiambutene 45. Dihydromorphine 46. Dimenoxadol 47. Dimepheptanol 48. Dimethylthiambutene 49. Dioxaphetyl butyrate 50. Diphenoxine 51. Dipipanone 52. DMA (2,5-dimethoxyamphetamine) 53. DMGP (dimetilgeptilpiran) 54. DMT (dimethyltryptamine) 55. DOB (d, L-2,5-dimethoxy-4-bromo-amphetamine) 56. DOC (d, L-2,5-dimethoxy-4-chloro-amphetamine) 57. DOET (2,5-dimethoxy-4-ethylamphetamine) 58. Drotebanol 59. Ecgonine 60. Ephedrone 61. Ethylmethylthiambutene 62. Eticyclidine 63. Etonitazene 64. Etorphine 65. Etoxeridine 66. Etryptamine 67. Furethidine 68. Hashish (Anasha, cannabis resin) 69. Heroin (Diacetylmorphine) 70. Hydrocodone 71. Hydrocodone phosphate 72. Hydromorphinol 73. Hydromorphone 74. Isomethadone 75. Ketobemidone 76. Khat 77. L- Methadone 78. Levomethorphan 79. Levomoramide 80. Levophenacylmorphan 81. Levorphanol 82. Lysergic acid and its preparations, that include d-Lysergide (LSD, LSD-25) 83. -

Government Gazette
Government Gazette REPUBLIC OF SOUTH AFRICA Regulation Gazette No. 7636 Vol. 454 Pretoria 10 April 2003 No. 24727 AIDS HELPLINE: 0800-0123-22 Prevention is the cure I STAATSKOERANT, 10 APRIL 2003 No. 24727 3 GOVERNMENT NOTICES GOEWERMENTSKENNISGEWINGS DEPARTMENT OF HEALTH DEPARTEMENT VAN GESONDHEID NO. R. 509 10 April 2003 SCHEDULES The Minister of Health has, in terms of section 22A(2) of the Medicines and Related Substances Act, 1965 (Act No. 101 of 1965), on the recommendation of the Medicines Control Council, made the Schedulesin the Schedule SCHEDULE I In these Schedules, "the Act" meansthe Medicines and Related SubstancesAct, 1965 (Act No. 101 of 1965) SCHEDULE 0 (a) All substancesreferred to in thisSchedule are excluded when specifically packed, labelled and usedfor - (i) industrialpurposes including the manufacture or compounding of consumer items or products which have no pharmacological oraction medicinal purpose, which are intended to be ingested by man or animals as food, or applied to the body as a cosmetic, and which are approved for such use in terms of the Foodstuffs, Cosmetics and Disinfectants Act, 1972 (Act No. 54 of 1972) or registeredin terms of theFertilizers, Farm Feeds, Agricultural Remedies and Stock Remedies Act, 1947 (Act No. 36 of 1947); and (ii)analytical laboratory purposes. (b) All substances referred to in this Schedule include the following: 4 No. 24727 GOVERNMENT GAZETTE, 10 APRIL 2003 (i) The saltsand esters of suchsub2ances,+vhere the existence of such salts and esters is possible; and (ii) All preparationsand mixtures of suchsubstances where such preparations and mixtures arenot expressly excluded. This Schedule includesall substances subject to registration in termsof the Act and which are not listed in anyof the other Schedules.