CASE REPORT Hypervascularity of the Glans Penis Diagnosed with Cutaneous Temperature Measurements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Reproductive System, Day 2 Grades 4-6, Lesson #12
Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Reproductive System, day 2 Grades 4-6, Lesson #12 Time Needed 40-50 minutes Student Learning Objectives To be able to... 1. Distinguish reproductive system facts from myths. 2. Distinguish among definitions of: ovulation, ejaculation, intercourse, fertilization, implantation, conception, circumcision, genitals, and semen. 3. Explain the process of the menstrual cycle and sperm production/ejaculation. Agenda 1. Explain lesson’s purpose. 2. Use transparencies or your own drawing skills to explain the processes of the male and female reproductive systems and to answer “Anonymous Question Box” questions. 3. Use Reproductive System Worksheets #3 and/or #4 to reinforce new terminology. 4. Use Reproductive System Worksheet #5 as a large group exercise to reinforce understanding of the reproductive process. 5. Use Reproductive System Worksheet #6 to further reinforce Activity #2, above. This lesson was most recently edited August, 2009. Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 1 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Materials Needed Classroom Materials: OPTIONAL: Reproductive System Transparency/Worksheets #1 – 2, as 4 transparencies (if you prefer not to draw) OPTIONAL: Overhead projector Student Materials: (for each student) Reproductive System Worksheets 3-6 (Which to use depends upon your class’ skill level. Each requires slightly higher level thinking.) Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 2 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. -

1 Male Checklist Male Reproductive System Components of the Male
Male Checklist Male Reproductive System Components of the male Testes; accessory glands and ducts; the penis; and reproductive system the scrotum. Functions of the male The male reproductive system produces sperm cells that reproductive system can be transferred to the female, resulting in fertilization and the formation of a new individual. It also produces sex hormones responsible for the normal development of the adult male body and sexual behavior. Penis The penis functions as the common outlet for semen (sperm cells and glandular secretions) and urine. The penis is also the male copulatory organ, containing tissue that can fill with blood resulting in erection of the penis. Prepuce A fold of skin over the distal end of the penis. Circumcision is the surgical removal of the prepuce. Corpus spongiosum A spongy body consisting of erectile tissue. It surrounds the urethra. Sexual excitement can cause erectile tissue to fill with blood. As a result, the penis becomes erect. Glans penis The expanded, distal end of the corpus spongiosum. It is also called the head of the penis. Bulb of the penis The proximal end of the corpus spongiosum. Bulbospongiosus muscle One of two skeletal muscles surrounding the bulb of the penis. At the end of urination, contraction of the bulbospongiosus muscles forces any remaining urine out of the urethra. During ejaculation, contractions of the bulbospongiosus muscles ejects semen from the penis. Contraction of the bulbospongiosus muscles compresses the corpus spongiosum, helping to maintain an erection. Corpus cavernosum One of two spongy bodies consisting of erectile tissue that (pl., corpora cavernosa) form the sides and front of the penis. -

In Brief the Foreskin
in brief In Brief The Foreskin Michael R. Lawless, MD skin and glans results in adhesionlike tion of steroid cream for up to 6 weeks Wake Forest University Health attachment of the foreskin to the glans in combination with gentle attempts to Services from birth throughout most of the first retract the foreskin is an effective non- Winston-Salem, NC postnatal year. This attachment is, in surgical treatment reported to be suc- essence, a physiologic phimosis that cessful in up to 75% to 85% of cases of inhibits retraction of the foreskin. The phimosis. Surgical treatment includes Author Disclosure tissue layer serves as an effective bar- circumcision or preputial plasty (dorsal Drs Lawless and Serwint did not rier against invading pathogens and slit). disclose any financial relationships accumulation of smegma. External Paraphimosis occurs when a some- relevant to this In Brief. cleansing of the penis with mild soap what tight foreskin is retracted and and water is the only genital care cannot be returned to its usual position required in the first year after birth. because of its constricting effect on the Treatment of Phimosis with Topical Forceful retraction of the foreskin prior shaft of the penis. The resulting venous Steroids in 194 Children. Ashfield to natural separation of the epithelial stasis causes painful swelling of the JE, Nickel KR, Siemens DR, et al. layers is painful to the infant. In addi- shaft and glans penis distal to the J Urol. 2003;169:1106–1108 tion to pain, traumatic foreskin retrac- constriction, further impeding replace- Paraphimosis: Current Treatment Op- tion may cause bleeding followed by an ment of the foreskin. -

Paraffin Granuloma Associated with Buried Glans Penis-Induced Sexual and Voiding Dysfunction
pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health 2017 August 35(2): 129-132 https://doi.org/10.5534/wjmh.2017.35.2.129 Case Report Paraffin Granuloma Associated with Buried Glans Penis-Induced Sexual and Voiding Dysfunction Wonhee Chon1, Ja Yun Koo1, Min Jung Park3, Kyung-Un Choi2, Hyun Jun Park1,3, Nam Cheol Park1,3 Departments of 1Urology and 2Pathology, Pusan National University School of Medicine, 3The Korea Institute for Public Sperm Bank, Busan, Korea A paraffinoma is a type of inflammatory lipogranuloma that develops after the injection of an artificial mineral oil, such as paraffin or silicon, into the foreskin or the subcutaneous tissue of the penis for the purpose of penis enlargement, cosmetics, or prosthesis. The authors experienced a case of macro-paraffinoma associated with sexual dysfunction, voiding dysfunction, and pain caused by a buried glans penis after a paraffin injection for penis enlargement that had been performed 35 years previously. Herein, this case is presented with a literature review. Key Words: Granuloma; Oils; Paraffin; Penis A paraffinoma is a type of inflammatory lipogranuloma because of tuberculous epididymitis [1,3]. that develops after the injection of an artificial mineral oil, However, various types of adverse effects were sub- such as paraffin or silicon, into the foreskin or the subcuta- sequently reported by several investigators, and such pro- neous tissue of the penis for the purpose of penis enlarge- cedures gradually became less common [3-6]. Paraffin in- ment, cosmetics, or prosthesis [1]. In particular, as this pro- jections display outcomes consistent with the purpose of cedure is performed illegally by non-medical personnel in the procedure in early stages, but over time, the foreign an unsterilized environment or with non-medical agents, matter migrates from the primary injection site to nearby cases of adverse effects, such as infection, skin necrosis, tissues or even along the inguinal lymphatic vessel. -

Human Glans and Preputial Development
Differentiation xxx (xxxx) xxx–xxx Contents lists available at ScienceDirect Differentiation journal homepage: www.elsevier.com/locate/diff ☆ Human glans and preputial development Xin Liu1, Ge Liu1, Joel Shen, Aaron Yue, Dylan Isaacson, Adriane Sinclair, Mei Cao, Aron Liaw, ⁎ Gerald R. Cunha, Laurence Baskin UCSF, USA ARTICLE INFO ABSTRACT Keywords: The urethra within the human penile shaft develops via (1) an “Opening Zipper” that facilitates distal canali- Development zation of the solid urethral plate to form a wide urethral groove and (2) a “Closing Zipper” that facilitates fusion Penis of the epithelial surfaces of the urethral folds. Herein, we extend our knowledge by describing formation of the Urethra human urethra within the glans penis as well as development of the prepuce. Forty-eight normal human fetal Human penile specimens were examined using scanning electron microscopy and optical projection tomography. Serial Glans histologic sections were evaluated for morphology and immunohistochemical localization for epithelial differ- Prepuce Canalization entiation markers: Cytokeratins 6, 7, 10, FoxA1, uroplakin and the androgen receptor. As the closing zipper completes fusion of the urethral folds within the penile shaft to form a tubular urethra (~ 13 weeks), canali- zation of the urethral plate continues in proximal to distal fashion into the glans penis to directly form the urethra within the glans without forming an open urethral groove. Initially, the urethral plate is attached ventrally to the epidermis via an epithelial seam, which is remodeled and eliminated, thus establishing me- senchymal confluence ventral to the glanular urethra. The morphogenetic remodeling involves the strategic expression of cytokeratin 7, FoxA1 and uroplakin in endodermal epithelial cells as the tubular glanular urethra forms. -

MALE GENITAL ORGANS and ACCESSORY GLANDS of the LESSER MOUSE DEER, TRAGULUS Fa VAN/CUS
MALE GENITAL ORGANS AND ACCESSORY GLANDS OF THE LESSER MOUSE DEER, TRAGULUS fA VAN/CUS M. K. VIDYADARAN, R. S. K. SHARMA, S. SUMITA, I. ZULKIFLI, AND A. RAZEEM-MAZLAN Faculty of Biomedical and Health Science, Universiti Putra Malaysia, 43400 UPM Serdang, Selangor, Malaysia (MKV), Faculty of Veterinary Medicine and Animal Sciences, Universiti Putra Malaysia, 43400 UPM Serdang, Selangor, Malaysia (RSKS, SS, /Z), Downloaded from https://academic.oup.com/jmammal/article/80/1/199/844673 by guest on 01 October 2021 Department of Wildlife and National Parks, Zoo Melaka, 75450 Melaka, Malaysia (ARM) Gross anatomical features of the male genital organs and accessory genital glands of the lesser mouse deer (Tragulus javanicus) are described. The long fibroelastic penis lacks a prominent glans and is coiled at its free end to form two and one-half turns. Near the tight coils of the penis, on the right ventrolateral aspect, lies a V-shaped ventral process. The scrotum is prominent, unpigmented, and devoid of hair and is attached close to the body, high in the perineal region. The ovoid, obliquely oriented testes carry a large cauda and caput epididymis. Accessory genital glands consist of paired, lobulated, club-shaped vesic ular glands, and a pair of ovoid bulbourethral glands. A well-defined prostate gland was not observed on the surface of the pelvic urethra. Many features of the male genital organs of T. javanicus are pleisomorphic, being retained from suiod ancestors of the Artiodactyla. Key words: Tragulus javanicus, male genital organs, accessory genital glands, reproduc tion, anatomy, Malaysia The lesser mouse deer (Tragulus javan gulidae, and Bovidae (Webb and Taylor, icus), although a ruminant, possesses cer 1980). -

The Treatment of Priapismfwhen and How?
International Journal of Impotence Research (2003) 15, Suppl 5, S86–S90 & 2003 Nature Publishing Group All rights reserved 0955-9930/03 $25.00 www.nature.com/ijir The treatment of priapismFwhen and how? DJ Bochinski1*, DY Deng1 and TF Lue1 1Department of Urology, University of California, San Francisco, California, USA Priapism is a condition first described by Tripe in 1845. It has been defined as a pathological condition of penile erection that persists beyond or is unrelated to sexual stimulation. Two variants of priapism have been well described. The ischemic priapism (also known as low-flow priapism) and nonischemic priapism (or high flow priapism) have unique and distinct causes. It is important to distinguish these two conditions as the treatment for each is different. This review will focus on the two types of priapism and the appropriate diagnostic work-up for each. As well, the medical and surgical treatment options for these two conditions will be described in detail. A third entity known as stuttering priapism will also be discussed as will its unique treatment alternatives. International Journal of Impotence Research (2003) 15, Suppl 5, S86–S90. doi:10.1038/sj.ijir.3901078 Keywords: priapism; ischemic; nonischemic; stuttering priapism; cavernosal shunts Introduction Nonsurgical treatment of ischemic priapism Priapism has been defined as a pathological condi- tion where a penile erection persists beyond or is In general, treatment is aimed at the primary cause unrelated to sexual stimulation. Priapism may be of the priapism if it can be identified. The goal of classified as ischemic or nonischemic. In the past, treatment is to relieve pain and abort the erection terms such as low-flow/high-flow priapism have that may cause damage to the corpora. -
Slang for Penis and Testicles
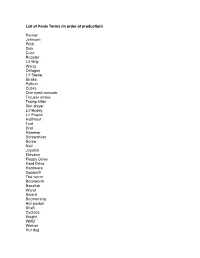
List of Penis Terms (in order of production) Pecker Johnson Prick Dick Cock Rooster Lil' Billy Wang Octagon Lil' Stevie Snake Python Cobra One eyed monster Trouser snake Tramp killer Slut slayer Lil' Buddy Lil' Friend Halfmast Tool Drill Hammer Screwdriver Screw Nail Joystick Elevator Floppy Drive Hard Drive Hardware Gearshift The worm Bookworm Basalisk Wand Sword Boomerang Hot pocket Shaft Cyclops Knight WMD Weiner Hot dog Popsicle Lollipop Kielbalsa Stick Ice Cream Cone Morning Wood The Colonel The Lieutenant The Tank The Battleship The land mine The assault rifle the grenade the machete The water gun Gun Banana Carrot Zuchini Cucumber Pickle The Major The seaman The key My asian buddy The shotgun Water hose Twix Snickers bar Bag of tricks Nuclear missile Hollow point The member Chairman Mao Mallet Pyramid Elephant Fuck Truck The mustang Cane Rod Staff Plug Cigar Nebraska State Capitol Turtle Head Undercover Brother The lightsaber Katana Sniper Rifle The sticky grenade Straw Remote Control The silver bullet Drumstick Bone Mast The machine The goods The hardware Junk Bulge The sequoia Bushwhacker The lawnmower Hoover tower The Washington monument The Lincoln memorial The pocket monster The pocket rocket The mongoose The ground squirrel The trombone Dong Torpedo Sausage Philly Cheesesteak The pendulum Babymaker Toy soldier Antenna The titanic Zeus Ares List of Testicle Terms (in order of production) Balls Stones Family Jewels Meatballs Reece's Pieces Nuts Coconuts Weights Walnuts Gonads Dumbbells Truffles The sperm factory Peanuts Chestnuts Package Grenades Huevos Water Balloons Wheels Itchy and scratchy Beavis and butthead Tweedledee and Tweedledum Easter eggs Fiery Coals Jellybeans Sack The two amigos Maracas. -

Supermicar Data Entry Instructions, 2007 363 Pp. Pdf Icon[PDF
SUPERMICAR TABLE OF CONTENTS Chapter I - Introduction to SuperMICAR ........................................... 1 A. History and Background .............................................. 1 Chapter II – The Death Certificate ..................................................... 3 Exercise 1 – Reading Death Certificate ........................... 7 Chapter III Basic Data Entry Instructions ....................................... 12 A. Creating a SuperMICAR File ....................................... 14 B. Entering and Saving Certificate Data........................... 18 C. Adding Certificates using SuperMICAR....................... 19 1. Opening a file........................................................ 19 2. Certificate.............................................................. 19 3. Sex........................................................................ 20 4. Date of Death........................................................ 20 5. Age: Number of Units ........................................... 20 6. Age: Unit............................................................... 20 7. Part I, Cause of Death .......................................... 21 8. Duration ................................................................ 22 9. Part II, Cause of Death ......................................... 22 10. Was Autopsy Performed....................................... 23 11. Were Autopsy Findings Available ......................... 23 12. Tobacco................................................................ 24 13. Pregnancy............................................................ -

Urethrectomy.Pdf
Information about your procedure from The British Association of Urological Surgeons (BAUS) This leaflet contains evidence-based information about your proposed urological procedure. We have consulted specialist surgeons during its preparation, so that it represents best practice in UK urology. You should use it in addition to any advice already given to you. To view the online version of this leaflet, type the text below into your web browser: http://www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/Urethrectomy.pdf Key Points • This involves removing the male urethra (waterpipe) because of the risk of cancer (or future cancer development) • It is usually done through an incision in your perineum (behind your scrotum) • You will get some temporary bruising around the incision and along your penis • You may get some temporary discharge from the tip of your penis until everything heals What does this procedure involve? Removing the whole of your urethra (waterpipe), from the tip of your penis to your prostate gland, through a small incision in your perineum (the skin beneath your scrotum). Bladder cancer can sometimes re-appear in your urethra after cystectomy (removal of your bladder) and construction of an ileal conduit. Because you no longer pass urine through your urethra after your bladder has been removed, you will not get bleeding in your urine to warn us that your cancer may have recurred in your urethra. Although this is rare, we sometimes advise that it should be removed to prevent the problem presenting later. Your surgeon and team will advise you if you need to have your urethra removed at the same time as your cystectomy. -

Morphology and Histology of the Penis
Morphology and histology of the penis Michelangelo Buonarotti: David, 1501. Ph.D, M.D. Dávid Lendvai Anatomy, Histology and Embryology Institute 2019. "See the problem is, God gave man a brain and another important organ, and only enough blood to run one at a time..." - R. W MALE GENITAL SYSTEM - SUMMERY male genital gland= testis •spermio/spermatogenesis •hormone production male genital tracts: epididymis vas deference (ductus deferens) ejaculatory duct •sperm transport 3 additional genital glands: 4 Penis: •secretion seminal vesicles •copulating organ prostate •male urethra Cowper-glands (bulbourethral gl.) •secretion PENIS Pars fixa (perineal) penis: Attached to the pubic bone Bulb and crura penis Pars libera (pendula) penis: Corpus + glans of penis resting ~ 10 cm Pars liberaPars erection ~ 16 cm Pars fixa penis Radix penis: Bulb of the penis: • pierced by the urethra • covered by the bulbospongiosus m. Crura penis: • fixed on the inf. ramus of the pubic bone inf. ramus of • covered by the ischiocavernosus m. the pubic bone Penis – connective tissue At the fixa p. and libera p. transition fundiforme lig. penis: superficial, to the linea alba, to the spf. abdominal fascia suspensorium lig. penis: deep, triangular, to the symphysis PENIS – ERECTILE BODIES 2 corpora cavernosa penis 1 corpus spongiosum penis (urethrae) → ends with the glans penis Libera partpendula=corpus penis + glans penis PENIS Ostium urethrae ext.: • at the glans penis •Vertical, fissure-like opening foreskin (Preputium): •glans > 2/3 covered during the ejaculation it's a reserve plate •fixed by the frenulum and around the coronal groove of the glans BLOOD SUPPLY OF THE PENIS int. pudendal A.