Urethrectomy.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reproductive System, Day 2 Grades 4-6, Lesson #12
Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Reproductive System, day 2 Grades 4-6, Lesson #12 Time Needed 40-50 minutes Student Learning Objectives To be able to... 1. Distinguish reproductive system facts from myths. 2. Distinguish among definitions of: ovulation, ejaculation, intercourse, fertilization, implantation, conception, circumcision, genitals, and semen. 3. Explain the process of the menstrual cycle and sperm production/ejaculation. Agenda 1. Explain lesson’s purpose. 2. Use transparencies or your own drawing skills to explain the processes of the male and female reproductive systems and to answer “Anonymous Question Box” questions. 3. Use Reproductive System Worksheets #3 and/or #4 to reinforce new terminology. 4. Use Reproductive System Worksheet #5 as a large group exercise to reinforce understanding of the reproductive process. 5. Use Reproductive System Worksheet #6 to further reinforce Activity #2, above. This lesson was most recently edited August, 2009. Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 1 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Materials Needed Classroom Materials: OPTIONAL: Reproductive System Transparency/Worksheets #1 – 2, as 4 transparencies (if you prefer not to draw) OPTIONAL: Overhead projector Student Materials: (for each student) Reproductive System Worksheets 3-6 (Which to use depends upon your class’ skill level. Each requires slightly higher level thinking.) Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 2 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. -

Human Glans and Preputial Development
Differentiation xxx (xxxx) xxx–xxx Contents lists available at ScienceDirect Differentiation journal homepage: www.elsevier.com/locate/diff ☆ Human glans and preputial development Xin Liu1, Ge Liu1, Joel Shen, Aaron Yue, Dylan Isaacson, Adriane Sinclair, Mei Cao, Aron Liaw, ⁎ Gerald R. Cunha, Laurence Baskin UCSF, USA ARTICLE INFO ABSTRACT Keywords: The urethra within the human penile shaft develops via (1) an “Opening Zipper” that facilitates distal canali- Development zation of the solid urethral plate to form a wide urethral groove and (2) a “Closing Zipper” that facilitates fusion Penis of the epithelial surfaces of the urethral folds. Herein, we extend our knowledge by describing formation of the Urethra human urethra within the glans penis as well as development of the prepuce. Forty-eight normal human fetal Human penile specimens were examined using scanning electron microscopy and optical projection tomography. Serial Glans histologic sections were evaluated for morphology and immunohistochemical localization for epithelial differ- Prepuce Canalization entiation markers: Cytokeratins 6, 7, 10, FoxA1, uroplakin and the androgen receptor. As the closing zipper completes fusion of the urethral folds within the penile shaft to form a tubular urethra (~ 13 weeks), canali- zation of the urethral plate continues in proximal to distal fashion into the glans penis to directly form the urethra within the glans without forming an open urethral groove. Initially, the urethral plate is attached ventrally to the epidermis via an epithelial seam, which is remodeled and eliminated, thus establishing me- senchymal confluence ventral to the glanular urethra. The morphogenetic remodeling involves the strategic expression of cytokeratin 7, FoxA1 and uroplakin in endodermal epithelial cells as the tubular glanular urethra forms. -
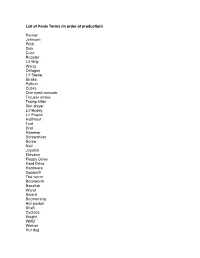
Slang for Penis and Testicles
List of Penis Terms (in order of production) Pecker Johnson Prick Dick Cock Rooster Lil' Billy Wang Octagon Lil' Stevie Snake Python Cobra One eyed monster Trouser snake Tramp killer Slut slayer Lil' Buddy Lil' Friend Halfmast Tool Drill Hammer Screwdriver Screw Nail Joystick Elevator Floppy Drive Hard Drive Hardware Gearshift The worm Bookworm Basalisk Wand Sword Boomerang Hot pocket Shaft Cyclops Knight WMD Weiner Hot dog Popsicle Lollipop Kielbalsa Stick Ice Cream Cone Morning Wood The Colonel The Lieutenant The Tank The Battleship The land mine The assault rifle the grenade the machete The water gun Gun Banana Carrot Zuchini Cucumber Pickle The Major The seaman The key My asian buddy The shotgun Water hose Twix Snickers bar Bag of tricks Nuclear missile Hollow point The member Chairman Mao Mallet Pyramid Elephant Fuck Truck The mustang Cane Rod Staff Plug Cigar Nebraska State Capitol Turtle Head Undercover Brother The lightsaber Katana Sniper Rifle The sticky grenade Straw Remote Control The silver bullet Drumstick Bone Mast The machine The goods The hardware Junk Bulge The sequoia Bushwhacker The lawnmower Hoover tower The Washington monument The Lincoln memorial The pocket monster The pocket rocket The mongoose The ground squirrel The trombone Dong Torpedo Sausage Philly Cheesesteak The pendulum Babymaker Toy soldier Antenna The titanic Zeus Ares List of Testicle Terms (in order of production) Balls Stones Family Jewels Meatballs Reece's Pieces Nuts Coconuts Weights Walnuts Gonads Dumbbells Truffles The sperm factory Peanuts Chestnuts Package Grenades Huevos Water Balloons Wheels Itchy and scratchy Beavis and butthead Tweedledee and Tweedledum Easter eggs Fiery Coals Jellybeans Sack The two amigos Maracas. -

Supermicar Data Entry Instructions, 2007 363 Pp. Pdf Icon[PDF
SUPERMICAR TABLE OF CONTENTS Chapter I - Introduction to SuperMICAR ........................................... 1 A. History and Background .............................................. 1 Chapter II – The Death Certificate ..................................................... 3 Exercise 1 – Reading Death Certificate ........................... 7 Chapter III Basic Data Entry Instructions ....................................... 12 A. Creating a SuperMICAR File ....................................... 14 B. Entering and Saving Certificate Data........................... 18 C. Adding Certificates using SuperMICAR....................... 19 1. Opening a file........................................................ 19 2. Certificate.............................................................. 19 3. Sex........................................................................ 20 4. Date of Death........................................................ 20 5. Age: Number of Units ........................................... 20 6. Age: Unit............................................................... 20 7. Part I, Cause of Death .......................................... 21 8. Duration ................................................................ 22 9. Part II, Cause of Death ......................................... 22 10. Was Autopsy Performed....................................... 23 11. Were Autopsy Findings Available ......................... 23 12. Tobacco................................................................ 24 13. Pregnancy............................................................ -

Undescended Testicles Patient Guide Table of Contents Pediatric Health Committee
PEDIATRIC HEALTH Undescended Testicles Patient Guide Table of Contents Pediatric Health Committee CHAIR Pediatric Health Committee . 2 T. Ernesto Figueroa, MD Kenny's Story . 3 Nemours/Alfred I . DuPont Hospital for Children Introduction: When Your Baby Boy Is Born . 4 Wilmington, DE GET THE FACTS . 5 How Does the Male Reproductive System Form? . 5 What Are Undescended Testicles (Cryptorchidism)? . 5 COMMITTEE MEMBERS What Causes this Problem? . 6 Paul Austin, MD GET DIAGNOSED . 6 Washington University School of Medicine in St . Louis GET TREATED . 7 St. Louis, MO AFTER TREATMENT . 7 GLOSSARY . 8 Ahmad Bani-Hani, MD QUESTIONS TO ASK YOUR DOCTOR . 9 Nemours/Alfred I . DuPont Hospital for Children About the Urology Care Foundation . [back cover] Wilmington, DE Michael Hsieh, MD Children’s National Health System Washington, DC 2 Kenny's Story When our son Kenny K* was born, we were so happy! He was absolutely beautiful . We were in love at first sight . He had all of his fingers and toes and looked like an angel . However, at three months old, we noticed that his genitals didn’t look right . We took him to his doctor and the pediatrician said he had an undescended testicle . Kenny’s pediatrician referred us to a specialist called “a pediatric urologist .” His urologist said an undescended testicle is a common problem and could easily be fixed . Everything else with Kenny was normal . After talking about all of our options, Kenny’s urologist recommended that he have surgery . After the surgery, Kenny didn’t have any other issues . He is growing up fine and doesn’t even know he had an issue . -

The Tanner Stages
Vermont Department of Health Health Screening Recommendations for Children & Adolescents The Tanner Stages Because the onset and progression of puberty are so variable, Tanner has proposed a scale, now uniformly accepted, to describe the onset and progression of pubertal changes (Fig. 9- I Preadolescent 24). Boys and girls are rated on a 5 point scale. Boys are rated for genital development and no sexual hair pubic hair growth, and girls are rated for breast development and pubic hair growth. Pubic hair growth in females is staged as follows (Fig 9-24, B): II Sparse, pigmented, long, straight, • Stage I (Preadolescent) - Vellos hair develops over the pubes in a manner not greater than that over mainly along labia the anterior wall. There is no sexual hair. and at base of penis • Stage II - Sparse, long, pigmented, downy hair, which is straight or only slightly curled, appears. These hairs are seen mainly along the labia. This stage is difficult to quantitate on black and white photographs, particularly when pictures are of fair-haired subjects. III • Stage III - Considerably darker, coarser, and curlier sexual hair appears. The hair has now spread Darker, coarser, curlier sparsely over the junction of the pubes. • Stage IV - The hair distribution is adult in type but decreased in total quantity. There is no spread to the medial surface of the thighs. • Stage V - Hair is adult in quantity and type and appears to have an inverse triangle of the classically IV Adult, but feminine type. There is spread to the medial surface of the thighs but not above the base of the decreased inverse triangle. -

Transurethral Resection of the Prostate (TURP)
Uroformation Prostate Surgery Transurethral Resection of the Prostate (TURP) The Uroformation series is a co-operative venture in patient centered urological information. June 2014 What is the Prostate? The prostate is a gland about the size of a walnut that is only present in men. It is located just below the bladder and surrounds the urethra, the tube through which urine flows from the bladder and out through the penis. The prostate gland contributes to the seminal fluid produced during ejaculation, and has an important function in fertility. 1 What is a TURP? A transurethral resection of the prostate (TURP) is an operation to treat urinary blockage caused by an enlarged prostate. When the prostate tissue enlarges, it squeezes inward on the urethra causing some or all of the following symptoms: The need to urinate often (frequency) The need to urinate in a hurry (urgency) The need to get up at night to urinate (nocturia) Difficulty starting urination (hesitancy) Difficulty stopping urination (terminal dribbling) Weak stream Incomplete emptying of the bladder Urinary retention (complete obstruction of the urethra, presents with severe pain and the inability to pass urine) Retention is tem- porarily managed with the insertion of a catheter to drain the blad- der Why might I need a TURP operation? To improve urine flow and bladder emptying To treat acute retention and complete blockages To prevent kidney damage caused by pressure forcing urine back towards the kidneys To reduce bladder infections and bladder stones caused by poor bladder emptying In some cases, the operation is necessary to prevent complications. -

Growth and Development of Male External Genitalia a Cross-Sectional Study of 6200 Males Aged 0 to 19 Years
ARTICLE Growth and Development of Male External Genitalia A Cross-sectional Study of 6200 Males Aged 0 to 19 Years Analia Tomova, MD, PhD; Fnu Deepinder, MD; Ralitsa Robeva, MD; Hristina Lalabonova, MD, PhD; Philip Kumanov, MD, PhD; Ashok Agarwal, PhD, HCLD Objective: To provide estimates of normal variations and penile circumference (measuring tape) from birth in penile measurements and testicular volumes, and to to 19 years of age. establish reference ranges for clinical use. Results: Testes did not show any increase in size until the onset of puberty at age 11 years, whereas penile growth Design: Cross-sectional, population-based study. was gradual after birth. However, both penile and testicu- lar development demonstrated peak growth from 12 to 16 Setting: Schools, kindergartens, and child care centers in different parts of Bulgaria. years of age, which coincided with the maximal male pu- bertal growth spurt. Data indicate an earlier pubertal de- Participants: A population of 6200 clinically healthy velopment for this study population than that for a simi- white males aged 0 to 19 years. lar population several decades ago. Significant differences betweenurbanandruralpopulationsregardingpenilelength Interventions: The study physician chose schools, were also noticed. kindergartens, and child care centers randomly and Conclusions: Our study provides the contemporary ref- examined children at random until he reached the erence range values for height, weight, testicular volume, required number. Each of the 20 age groups (age and penile length and circumference of males aged 0 to range, 0-19 years) had an equal number of males (ie, 19 years. Our data show that, even by the end of 20th cen- 310). -

BENEFITS of TUCKING Health and Safety Tips
BENEFITS OF TUCKING THINGS TO KNOW ABOUT Tucking involves hiding external genitalia so that they are not visible in tight clothing. Tucking is a do-it-yourself option for changing your appearance so that it matches your gender expression. You might tuck to feel more at ease in your body, TUCKING to feel more comfortable in your clothing, or to help others read your gender correctly. Health and safety tips: • If you are new to tucking, start by tucking for shorter periods of time. Give yourself lots of time to practice. It’s hard to learn a new skill when you feel rushed or stressed. Take a break between attempts. • Try switching between different ways of tucking. • You may find that tucking gets easier with practice or after being on hormones for awhile. • Tucking shouldn’t be overly uncomfortable. If you feel faint, nausea, or pain, take a break and try a different way of tucking. • After untucking, check for irritated skin, sores or rashes. Allow skin to heal before using products on it again. • Whenever reasonable, stay hydrated. Avoiding drinking and peeing can lead to health problems. • Use body powder in warm creases (thighs, buttocks, genital skin, etc.) to prevent skin chaffing and infection. • Tucking regularly can affect fertility. Some people consider banking sperm or limiting how often they tuck gonads inside the body. • See a clinician if you experience: aching, tingling or numbness that continues even when you aren’t tucking; blood in urine or orgasmic fluid; a feeling of inflammation or infection inside the genitals; skin rash or sores; pain with urination; or pain in the bladder or lower back. -

Animal/Dairy Science 434� Learning Objectives
Animal/Dairy Science 434 ! Learning Objectives Male Reproductive Tract Anatomy! • To be able to describe the male reproductive system in the bull. – Structure – Function Testis! Epididymis! Factory! Finishing School! Bull Reproductive Tract! • 1-25 X 109 sperm/day! • Fluid Absorption! • “Plant” must be air • 8-25 X 109 sperm! conditioned! – membrane changes! – nuclear & flagellar stabilization! – motility, fertility! Penis! – cytoplasmic droplet translocation! Delivery System! • Erection! • Protrusion! • Ejaculation! Tail of Epididymis! Warehouse and Delivery! • Storage 10-50 X 109 sperm! • Sperm for 5-10 ejaculates! • Smooth muscle contractions Accessory Sex Glands! upon sexual stimulation! Alterations & Packaging! • Metabolic substrates! • Surface coatings! • Transport for sperm! Reproductive Reproductive Organs of the Organs of the Bull! Bull! Testis! Primary Sex Organ Bull Tract! • Thermosensor! • Radiator! Bull Testis! • Protective sac! Scrotum! Bull Tract! Scrotal Cross Section! Longitudinal Section Cross Section Structure of the Testis! Scrotal Longitudinal" Seminiferous Tubule Section ! Tunica Albuginea Rete Testis (within the mediastinum) Structure of Mediastinum! Rete Testis! the Testis! Seminiferous! Tubule! Seminiferous Tubule Tunica Albuginea Rete Testis (within the mediastinum) The Testis! Structure of Spermatic Cord Structure of Spermatic Cord the Testis! the Testis! Secondary Sex Organs Vas Deferens Vas Deferens Caput Epididymis Caput Epididymis • Vasectomy • Vasectomy Vas Efferentia Vas Efferentia Seminiferous Tubule 6-12 -

Epididymitis N
n Epididymitis n who have had a bladder infection. In boys before puberty, Epididymitis is an infection or inflammation of epididymitis may be associated with abnormalities of the the epididymis, a structure that carries sperm from reproductive system (testicles) or urinary system (bladder the testicles. Epididymitis can be a sexually trans- and kidneys). mitted disease, but not always. The main symp- toms are pain and swelling of the scrotum (the What are some possible sac containing the testicles). It is important to get medical help for this condition. Rest and antibio- complications of epididymitis? tics are the usual treatments. With proper treatment, complications are uncommon. Without treatment, the infection may spread. This can cause damage to the reproductive organs, possibly includ- What is epididymitis? ing infertility. Epididymitis is a painful condition caused by inflamma- What increases the risk of tion of the epididymis, which carries and stores sperm. It is located in the scrotum next to the testicle. Epididymitis epididymitis? is most common in young men. It may be caused by a sex- When epididymitis is from a sexually transmitted dis- ually transmitted infection, although other sources of infec- ease, the main risk factors are having a lot of partners tion are possible. Once epididymitis is recognized, it usually and not using a condom every time you have sex. improves quickly with antibiotics and other simple treat- ments. Bladder infections and other infections of the reproduc- Epididymitis is uncommon in boys before puberty. In this tive organs may also lead to epididymitis. Other abnorm- age group, swelling of the scrotum is more often caused alities or previous surgery of the reproductive or urinary by a condition called testicular torsion. -

Anthropometric Study of Penile Length in Self-Declared Brazilians Regarding the Color of the Skin As White Or Black: the Study of a Myth
International Journal of Impotence Research https://doi.org/10.1038/s41443-017-0009-z ARTICLE Anthropometric study of penile length in self-declared Brazilians regarding the color of the skin as white or black: The study of a Myth 1 1 1 1 Rogério Alves Barboza ● Eloísio Alexsandro da Silva ● Tamiris Ruellas ● Ronaldo Damião Received: 16 November 2016 / Accepted: 31 July 2017 © The Author(s) 2017 Abstract This is an observational transversal cohort study in which we aim to analyze the Brazilian penis length and compare the penis size of the men self-declared as white (SDW) or black (SDB) skin color. Subjects were asked for self-declare according to their skin color, after that they have been invited to participate in a semi-structured interview so as to have their perception evaluated regarding their penis size and their self-esteem as well. Eventually, their penis length was measured with an anthropometric ruler. The men´s mean penis length who declared themselves as black skin color was 16.5 ± 1.7 cm (penis length in real fully-stretched flaccid length) and the men´s mean penis length who declared themselves as white skin color 1234567890 was 15.8 ± 1.6 cm (p < 0.001).The majority of either SDB (94.0%) or SDW (89.4%) are satisfied with their penis size (p = 0.464). We have shown that the man´s mean penis length who identifies himself as black is just a little bit bigger than the one who identifies himself as white. However, there were no significant difference between groups regarding self-assessment of genital body image.