Cardiac Toxidromes Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Report on the National Seminar on Radioimmunoassays Radiation Medicine Centre, B.A.R.C
REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16-20, 1978 RADIATION MEDICINE CENTRE, B.A.R.C. DEPARTMENT OF ATOMIC ENERGY AND WORLD HEALTH ORGANISATION REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16—20, 1978 RADIATION MEDICINE CENTRE, BARC TATA MEMORIAL HOSPITAL ANNEXE JERBAI WADIA ROAD, PAREL BOMBAY 400 012 ORGANISED UNDER THE AUSPICES OF THE DEPARTMENT OF ATOMIC ENERGY & WORLD HEALTH ORGANISATION CONTENTS Page Preface .. .. .. .. .. .. .. 3 Administrative Responsibilities .. .. .. .. 6 List of Participants 7 Programme .. .. .. .. .. .. .. 11 Basic Requirements of RIA in India .. .. .. 14 a. Radioisotopes for RIA's .. .. .. .. .. 15 b. Kits for RIA 17 c. Availability of Antibodies 19 d. National Pituitary Agency .. .. .. .. 20 e. Well-counter for RIA 21 f. Radiation Protection Aspects of RIA 23 Review of Discussion following the Session .. .. 26 State of Art of RIA's in India 28 Trigger Sessions 36 a. Quality Control of RIA's 37 b. Usefulness and limitations of RIA's in clinical diagnosis 39 c. RIA's in tropical diseases •. .. .. .. .. 42 d. Centralised assay services .. .. .. .. 44 Recommendations and Guidelines .. .. .. .. 46 Backword 51 Bibliography . .. .. .. .. .. .. 53 PREFACE This National Seminar on Radioimmunoassays was the second National Seminar jointly sponsored by Department of Atomic Energy and World Health Organisation and organised at Radiation Medicine Centre. The first one on 'Nuclear Medicine in India' was held in December 1976. The present Seminar on Radioimmunoassays was distinguished by the participation of Dr. Rosalyn Yalow, Nobel Laureate in Medicine for 1977. She, along with Dr. Solomon A. Berson, discovered the technique of Radioimmunoassay and nurtured it through the early years with hard and meticulous work to establish its usefulness in medical science. -
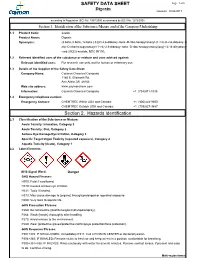
Digoxin SAFETY DATA SHEET Section 2. Hazards Identification
SAFETY DATA SHEET Page: 1 of 6 Digoxin Revision: 08/24/2017 according to Regulation (EC) No. 1907/2006 as amended by (EC) No. 1272/2008 Section 1. Identification of the Substance/Mixture and of the Company/Undertaking 1.1 Product Code: 22266 Product Name: Digoxin Synonyms: (3.beta.,5.beta.,12.beta.)-3-[(O-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl-(1->4)-O-2,6-dideoxy-.b eta.-D-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy- card-20(22)-enolide; NSC 95100; 1.2 Relevant identified uses of the substance or mixture and uses advised against: Relevant identified uses: For research use only, not for human or veterinary use. 1.3 Details of the Supplier of the Safety Data Sheet: Company Name: Cayman Chemical Company 1180 E. Ellsworth Rd. Ann Arbor, MI 48108 Web site address: www.caymanchem.com Information: Cayman Chemical Company +1 (734)971-3335 1.4 Emergency telephone number: Emergency Contact: CHEMTREC Within USA and Canada: +1 (800)424-9300 CHEMTREC Outside USA and Canada: +1 (703)527-3887 Section 2. Hazards Identification 2.1 Classification of the Substance or Mixture: Acute Toxicity: Inhalation, Category 3 Acute Toxicity: Oral, Category 2 Serious Eye Damage/Eye Irritation, Category 2 Specific Target Organ Toxicity (repeated exposure), Category 2 Aquatic Toxicity (Acute), Category 1 2.2 Label Elements: GHS Signal Word: Danger GHS Hazard Phrases: H300: Fatal if swallowed. H319: Causes serious eye irritation. H331: Toxic if inhaled. H373: May cause damage to {organs} through prolonged or repeated exposure. H400: Very toxic to aquatic life. -

Digoxin Toxicity 1
Chronic Digoxin Toxicity Reviewers: Shawn M. Varney, Authors: Matthew Riddle, MD, Mel Otten, MD MD Target Audience: Emergency Medicine Residents (junior and senior level postgraduate learners), Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of digoxin toxicity 2. Order appropriate diagnostic studies for evaluation of digoxin toxicity 3. Appropriately interpret ECG 4. Administer digoxin-specific antibody fragments (DSFab) 5. Recognize acute kidney injury as a precipitating factor of toxicity, and treat acute kidney injury appropriately 6. Select an appropriate disposition for patient with digoxin toxicity Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Develop independent differential diagnosis in setting of leading information from the nurse 2. Describe the mechanism of digoxin toxicity and treatment, DSFab 3. Use appropriate dosing strategy for DSFab administration Critical actions checklist: 1. Order a basic metabolic panel 2. Order a digoxin level 3. Obtain ECG 4. Provide volume resuscitation for acute kidney injury 5. Administer digoxin antibody fragments 6. Consult Poison Center/Toxicologist 7. Admit to the MICU Environment: Emergency Department treatment area 1. Room Set Up – ED critical care area a. Manikin Set Up – Mid or high fidelity simulator b. Props – Standard ED equipment 2. Distractors – ED noise, alarming monitor For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background The setting is an urban emergency department. The patient is a 63-year-old male with a history of atrial fibrillation, HTN, and CHF brought to the emergency department by EMS for nausea and vomiting for the past four days and confusion that began shortly before arrival. PMHx: atrial fibrillation, HTN, and CHF PSHx: None Medications: ASA 81 mg once daily, Digoxin 250 mcg once daily, Amlodipine 10 mg once daily, Lasix 20 mg twice daily, warfarin 5 mg once daily Allergies: NKDA SocHx: smokes ½ ppd for 40 years. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Top Ten Potential Drug Interactions in Small Animal Medicine EJCAP 26(34 Autumn 2016 P 9
Top Ten Potential Drug Interactions in Small Animal Medicine EJCAP 26(34 Autumn 2016 P 9 Fecava lecture* Top Ten Potential Drug Interactions in Small Animal Medicine Jennifer M. Reinhart, Lauren A. Trepanier1 SUMMARY Today, comorbidities are increasingly diagnosed in veterinary patients and multiple drug combinations are common. However, as the number of administered drugs increases, so too does the risk for adverse drug interactions. Much of what is known about drug-drug interactions is taken from the human literature, but a growing body of work in veterinary medicine also exists. The purpose of this review is to summarize the current knowledge of potential drug interactions in humans and dogs for ten ‘at risk’ drugs used in small animal medicine: cimetidine, sucralfate, ketoconazole, fluoroquinolone antibiotics, omeprazole, phenobarbital, clomipramine, furosemide, metoclopramide, and cyclosporine. Increased awareness of these potential drug interactions will enhance therapeutic decision-making and improve the level of care for veterinary patients. Key words: drug-drug interaction, drug metabolism, adverse drug reaction, polypharmacy *This paper is based on the FECAVA lecture Cimetidine delivered at the 22nd EuroCongress in Vienna, Austria in June 2016. Eur J Comp An Pract Cimetidine, a histamine (H2) blocker often used to prevent (Winter 2016) 26(4); p9-p19. Go to http:// and treat gastrointestinal ulcers, is a potent inhibitor of www.ejcap.org for the interactive online presentation of this paper several families of cytochrome P450 enzymes in humans, including CYP2D6 and CYP3A4 [2]. Cimetidine can also inhibit transporter pumps and decrease the renal tubular Introduction secretion of some drugs [3]. Cimetidine decreases the clearance of many drugs to variable degrees in humans, In humans, the risk of adverse drug interactions multiplies including theophylline [4,5], lidocaine [6], midazolam [7,8], as the number of administered drugs increases. -

Position Statement: Multi Dose Activated Charcoal
Journal of Toxicology: Clinical Toxicology ISSN: 0731-3810 (Print) (Online) Journal homepage: http://www.tandfonline.com/loi/ictx19 Position Statement and Practice Guidelines on the Use of Multi-Dose Activated Charcoal in the Treatment of Acute Poisoning American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists To cite this article: American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists (1999) Position Statement and Practice Guidelines on the Use of Multi-Dose Activated Charcoal in the Treatment of Acute Poisoning, Journal of Toxicology: Clinical Toxicology, 37:6, 731-751, DOI: 10.1081/CLT-100102451 To link to this article: http://dx.doi.org/10.1081/CLT-100102451 Published online: 18 Nov 2004. Submit your article to this journal Article views: 389 View related articles Citing articles: 175 View citing articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ictx19 Download by: [UPSTATE Medical University Health Sciences Library] Date: 29 May 2017, At: 09:34 Clinical Toxicology, 37(6), 731±751 (1999) Position Statement and Practice Guidelines on the Use of Multi-Dose Activated Charcoal in the Treatment of Acute Poisoning American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists ABSTRACT In preparing this Position Statement, all relevant scienti®c literature was identi- ®ed and reviewed critically by acknowledged experts using agreed criteria.1±124 Well-conducted clinical and experimental studies were given precedence over anecdotal case reports and abstracts were not usually considered. A draft Posi- tion Statement was then produced and subjected to detailed peer review by an international group of clinical toxicologists chosen by the American Academy of Clinical Toxicology and the European Association of Poisons Centres and Clinical Toxicologists. -

Caution from Using Cardiac Glycosides Digoxin Drug Which Have Properties Therapeutic Index
Omran (2019): Use of cardiac glycosides digoxin November 2019 Vol. 22(8) Caution from using cardiac glycosides digoxin drug which have properties therapeutic index (Ti) narrow compare with the medications wide therapeutic index Salah Abd-Al kader Omran1* 1. Al-Muthanna University, college of Medicine, Iraq *Corresponding authorEmil: [email protected]. Phone: 009647705338787 Abstract Clinical research will be based on the practical application of randomly assigned patients over the age of 25 who numbered 730 at the Academic Teaching Hospital in Iraq - Samawa. We used drugs narrow therapeutic index (NTI), which is used with caution at a specific and calculated dose because it is life-threatening and has high toxicity. Compared to drugs that have wide therapeutic index (WTI) and less serious effects (such as aspirin, acetaminophen (paracetamol), penicillin, etc.), we selected acetaminophen (paracetamol) in patient research (a wide therapeutic index) and the dose and ratio between the toxic dose and the safe therapeutic dose of the drug, the research focuses on dilution To limit the risk of medication to patients (mortality), which is used as a measure of the relative safety of the drug in a particular drug treatment, our main work is limited to digoxin (cardiac glycosides) used in heart disease, discrimination with other drugs and knowledge, and in comparison to drugs. We used acetaminophen (paracetol) which is a broad indicator, so we based on previous knowledge in clinical pharmacy, dosage medications, therapeutic toxic dose, maximum dose, initial dose, maintenance dose, lethal dose, by knowing Therapeutic index for drug identification, therapeutic index, therapeutic ratio, TI can be calculated as a lethal dose of the drug by 50% of the population (LD50) divided by the minimum effective dose for 50% of the population (ED50), that is, TI = LD50 / ED50. -

Antidotes in Poisoning Binila Chacko1, John V Peter2
INVITED ARTICLE Antidotes in Poisoning Binila Chacko1, John V Peter2 ABSTRACT Introduction: Antidotes are agents that negate the effect of a poison or toxin. Antidotes mediate its effect either by preventing the absorption of the toxin, by binding and neutralizing the poison, antagonizing its end-organ effect, or by inhibition of conversion of the toxin to more toxic metabolites. Antidote administration may not only result in the reduction of free or active toxin level, but also in the mitigation of end-organ effects of the toxin by mechanisms that include competitive inhibition, receptor blockade or direct antagonism of the toxin. Mechanism of action of antidotes: Reduction in free toxin level can be achieved by specific and non-specific agents that bind to the toxin. The most commonly used non-specific binding agent is activated charcoal. Specific binders include chelating agents, bioscavenger therapy and immunotherapy. In some situations, enhanced elimination can be achieved by urinary alkalization or hemadsorption. Competitive inhibition of enzymes (e.g. ethanol for methanol poisoning), enhancement of enzyme function (e.g. oximes for organophosphorus poisoning) and competitive receptor blockade (e.g. naloxone, flumazenil) are other mechanisms by which antidotes act. Drugs such as N-acetyl cysteine and sodium thiocyanate reduce the formation of toxic metabolites in paracetamol and cyanide poisoning respectively. Drugs such as atropine and magnesium are used to counteract the end-organ effects in organophosphorus poisoning. Vitamins such as vitamin K, folic acid and pyridoxine are used to antagonise the effects of warfarin, methotrexate and INH respectively in the setting of toxicity or overdose. This review provides an overview of the role of antidotes in poisoning. -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD May 2016 CONTENTS General Toxicology 8 Metals 33 Management 16 Pesticides 35 Drugs 19 Chemical Warfare 37 Chemical Incidents & 28 Plants 37 Pollution Chemicals 29 Animals 38 CURRENT AWARENESS PAPERS OF THE MONTH Efficacy and effectiveness of anti-digoxin antibodies in chronic digoxin poisonings from the DORA study (ATOM-1) Chan BS, Isbister GK, O'Leary M, Chiew A, Buckley NA. Clin Toxicol 2016; online early: doi: 10.1080/15563650.2016.1175620: Context We hypothesized that in chronic digoxin toxicity, anti-digoxin antibodies (Fab) would be efficacious in binding digoxin, but this may not translate into improved clinical outcomes. Objective This study aims to investigate changes in free digoxin concentrations and clinical effects on heart rate and potassium concentrations in chronic digoxin poisoning when anti-digoxin Fab are given. Materials and methods This is a prospective observational study. Patients were recruited if they have been treated with anti-digoxin Fab for chronic digoxin poisoning. Data was entered into a standardised prospective form, supplemented with medical records. Their serum or plasma was collected, analysed for free and bound digoxin and free anti-digoxin Fab concentrations. Results From September 2013 to February 2015, 36 patients (median age, 78 years; 22 females) Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England 2 were recruited from 18 hospitals. -

Poisonous Plants
Plants Poisonous Plants ACMT Board Review Course September 9, 2012 Thomas C. Arnold, M.D. 1 Special Acknowledgement • Thanks to Michelle Ruha and other previous presenters for their efforts on this topic. 2 Plants • Natural Products: 5% of tox boards – Includes food and marine poisonings, herbals, plants, fungi, toxic envenomations • ~ 5% of exposures reported to PCC each year, most in children < 6 years – Often a few deaths per year, but most reported exposures minor 3 1 Plants Plant Poisoning by Organ System • GI toxins • CNS toxins • Cardiovascular toxins • Multiorgan-system toxins • Hepatotoxins • Nephrotoxins • Endocrine toxins • Dermal and mucous membrane irritants 4 Lots of calls / Little threat • Euphorbia pulcherrima – Poinsettia • Ilex spp – Holly • Phoradendron spp – Mistletoe • Lantana spp • Spathiphyllum spp – Peace lily 5 • Ingestion of this plant may produce severe vomiting and diarrhea. Purple stains on fingers and a foamy quality to the diarrhea may provide a clue to the species of plant. Pokeweed AKA Phytolacca americana Toxin: phytolaccatoxin 6 2 Plants Phytolacca americana • Edible if parboiled • Root is the most toxic part, mature berries least toxic • Contains pokeweed mitogen – May see plasmacytosis • Supportive care 7 Wikivisual.com Solanum spp wiki • 1700 species; nightshade, potato • Poisoning usually from ingestion of immature fruit • Solanine glycoalkaloids – Usually produce GI irritant effects – Hallucinations and coma reported 8 Melia azedarach Toxin: meliatoxins Chinaberry9 3 Plants Chinaberry • Tree grows