Poisonous Plants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Nightshade”—A Hierarchical Classification Approach to T Identification of Hallucinogenic Solanaceae Spp
Talanta 204 (2019) 739–746 Contents lists available at ScienceDirect Talanta journal homepage: www.elsevier.com/locate/talanta Call it a “nightshade”—A hierarchical classification approach to T identification of hallucinogenic Solanaceae spp. using DART-HRMS-derived chemical signatures ∗ Samira Beyramysoltan, Nana-Hawwa Abdul-Rahman, Rabi A. Musah Department of Chemistry, State University of New York at Albany, 1400 Washington Ave, Albany, NY, 12222, USA ARTICLE INFO ABSTRACT Keywords: Plants that produce atropine and scopolamine fall under several genera within the nightshade family. Both Hierarchical classification atropine and scopolamine are used clinically, but they are also important in a forensics context because they are Psychoactive plants abused recreationally for their psychoactive properties. The accurate species attribution of these plants, which Seed species identifiction are related taxonomically, and which all contain the same characteristic biomarkers, is a challenging problem in Metabolome profiling both forensics and horticulture, as the plants are not only mind-altering, but are also important in landscaping as Direct analysis in real time-mass spectrometry ornamentals. Ambient ionization mass spectrometry in combination with a hierarchical classification workflow Chemometrics is shown to enable species identification of these plants. The hierarchical classification simplifies the classifi- cation problem to primarily consider the subset of models that account for the hierarchy taxonomy, instead of having it be based on discrimination between species using a single flat classification model. Accordingly, the seeds of 24 nightshade plant species spanning 5 genera (i.e. Atropa, Brugmansia, Datura, Hyocyamus and Mandragora), were analyzed by direct analysis in real time-high resolution mass spectrometry (DART-HRMS) with minimal sample preparation required. -

Inventory of Toxic Plants in Morocco: an Overview of the Botanical, Biogeography, and Phytochemistry Studies
Hindawi Journal of Toxicology Volume 2018, Article ID 4563735, 13 pages https://doi.org/10.1155/2018/4563735 Review Article Inventory of Toxic Plants in Morocco: An Overview of the Botanical, Biogeography, and Phytochemistry Studies Hanane Benzeid , Fadma Gouaz, Abba Hamadoun Touré, Mustapha Bouatia , Mohamed Oulad Bouyahya Idrissi, and Mustapha Draoui LaboratoiredeChimieAnalytiqueetdeBromatologie,FacultedeM´ edecine´ et de Pharmacie, Universite´ Mohamed V, Rabat, Morocco Correspondence should be addressed to Hanane Benzeid; [email protected] Received 10 December 2017; Revised 22 February 2018; Accepted 25 March 2018; Published 3 May 2018 Academic Editor: Orish Ebere Orisakwe Copyright © 2018 Hanane Benzeid et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Since they are natural, plants are wrongly considered nondangerous; therefore people used them in various contexts. Each plant is used alone or in mixture with others, where knowledge and the requirements of preparation and consumption are not mastered. Tus, intoxications due to the use of plants have become more and more frequent. Te reports of intoxications made at the Antipoison Center and Pharmacovigilance of Morocco (ACPM) support this fnding, since the interrogations sufered by the victimsshowthattheuseofplantsispracticedirrationally,anarchically, and uncontrollably. Faced by the increase of these cases of poisoning in Morocco, it seemed necessary to investigate the nature of poisonous plants, their monographs, and the chemicals responsible for this toxicity. 1. Introduction Tus, we thought it is necessary to study the nature of these poisonous plants and their monographs. Sinceimmemorialtime,thehumanhasusedplants,frstto feed himself and then to heal himself. -

Report on the National Seminar on Radioimmunoassays Radiation Medicine Centre, B.A.R.C
REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16-20, 1978 RADIATION MEDICINE CENTRE, B.A.R.C. DEPARTMENT OF ATOMIC ENERGY AND WORLD HEALTH ORGANISATION REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16—20, 1978 RADIATION MEDICINE CENTRE, BARC TATA MEMORIAL HOSPITAL ANNEXE JERBAI WADIA ROAD, PAREL BOMBAY 400 012 ORGANISED UNDER THE AUSPICES OF THE DEPARTMENT OF ATOMIC ENERGY & WORLD HEALTH ORGANISATION CONTENTS Page Preface .. .. .. .. .. .. .. 3 Administrative Responsibilities .. .. .. .. 6 List of Participants 7 Programme .. .. .. .. .. .. .. 11 Basic Requirements of RIA in India .. .. .. 14 a. Radioisotopes for RIA's .. .. .. .. .. 15 b. Kits for RIA 17 c. Availability of Antibodies 19 d. National Pituitary Agency .. .. .. .. 20 e. Well-counter for RIA 21 f. Radiation Protection Aspects of RIA 23 Review of Discussion following the Session .. .. 26 State of Art of RIA's in India 28 Trigger Sessions 36 a. Quality Control of RIA's 37 b. Usefulness and limitations of RIA's in clinical diagnosis 39 c. RIA's in tropical diseases •. .. .. .. .. 42 d. Centralised assay services .. .. .. .. 44 Recommendations and Guidelines .. .. .. .. 46 Backword 51 Bibliography . .. .. .. .. .. .. 53 PREFACE This National Seminar on Radioimmunoassays was the second National Seminar jointly sponsored by Department of Atomic Energy and World Health Organisation and organised at Radiation Medicine Centre. The first one on 'Nuclear Medicine in India' was held in December 1976. The present Seminar on Radioimmunoassays was distinguished by the participation of Dr. Rosalyn Yalow, Nobel Laureate in Medicine for 1977. She, along with Dr. Solomon A. Berson, discovered the technique of Radioimmunoassay and nurtured it through the early years with hard and meticulous work to establish its usefulness in medical science. -

PSYCHEDELIC DRUGS (P.L) 1. Terminology “Hallucinogens
PSYCHEDELIC DRUGS (p.l) 1. Terminology “hallucinogens” – induce hallucinations, although sensory distortions are more common “psychotomimetics” – to minic psychotic states, although truly most drugs in this class do not do so “phantasticums”or “psychedelics” – alter sensory perception (Julien uses “psychedelics”) alterations in perception, cognition, and mood, in presence of otherwise clear ability to sense” may increase sensory awareness, increase clarity, decrease control over what is sensed/experienced “self-A” may feel a passive observer of what “self-B” is experiencing often accompanied by a sense of profound meaningfulness, of divine or cosmic importance (limbic system?) these drugs can be classified by what NT they mimic: anti-ACh, agonists for NE, 5HT, or glutamate (See p. 332, Table 12.l in Julien, 9th Ed.) 2. The Anti-ACh Psychedelics e.g. scopolamine (classified as an ACh blocker) high affinity, no efficacy plant product: Belladonna or “deadly nightshade” (Atropa belladonna) Datura stramonium (jimson weed, stinkweed) Mandragora officinarum (mandrake plant) pupillary dilation (2nd to atropine) PSYCHEDELIC DRUGS (p.2) 2. Anti-ACh Psychedelics (cont.) pharmacological effects: e.g. scopolamine (Donnatal) clinically used to tx motion sickness, relax smooth muscles (gastric cramping), mild sedation/anesthetic effect PNS effects --- dry mouth relaxation of smooth muscles decreased sweating increased body temperature blurred vision dry skin pupillary dilation tachycardia, increased BP CNS effects --- drowsiness, mild euphoria profound amnesia fatigue decreased attention, focus delirium, mental confusion decreased REM sleep no increase in sensory awareness as dose increases --- restlessness, excitement, hallucinations, euphoria, disorientation at toxic dose levels --- “psychotic delirium”, confusion, stupor, coma, respiratory depression so drug is really an intoxicant, amnestic, and deliriant 3. -

The Phytochemistry of Cherokee Aromatic Medicinal Plants
medicines Review The Phytochemistry of Cherokee Aromatic Medicinal Plants William N. Setzer 1,2 1 Department of Chemistry, University of Alabama in Huntsville, Huntsville, AL 35899, USA; [email protected]; Tel.: +1-256-824-6519 2 Aromatic Plant Research Center, 230 N 1200 E, Suite 102, Lehi, UT 84043, USA Received: 25 October 2018; Accepted: 8 November 2018; Published: 12 November 2018 Abstract: Background: Native Americans have had a rich ethnobotanical heritage for treating diseases, ailments, and injuries. Cherokee traditional medicine has provided numerous aromatic and medicinal plants that not only were used by the Cherokee people, but were also adopted for use by European settlers in North America. Methods: The aim of this review was to examine the Cherokee ethnobotanical literature and the published phytochemical investigations on Cherokee medicinal plants and to correlate phytochemical constituents with traditional uses and biological activities. Results: Several Cherokee medicinal plants are still in use today as herbal medicines, including, for example, yarrow (Achillea millefolium), black cohosh (Cimicifuga racemosa), American ginseng (Panax quinquefolius), and blue skullcap (Scutellaria lateriflora). This review presents a summary of the traditional uses, phytochemical constituents, and biological activities of Cherokee aromatic and medicinal plants. Conclusions: The list is not complete, however, as there is still much work needed in phytochemical investigation and pharmacological evaluation of many traditional herbal medicines. Keywords: Cherokee; Native American; traditional herbal medicine; chemical constituents; pharmacology 1. Introduction Natural products have been an important source of medicinal agents throughout history and modern medicine continues to rely on traditional knowledge for treatment of human maladies [1]. Traditional medicines such as Traditional Chinese Medicine [2], Ayurvedic [3], and medicinal plants from Latin America [4] have proven to be rich resources of biologically active compounds and potential new drugs. -

Common Poisonous Plants in Sri Lanka
COMMON POISONOUS PLANTS IN SRI LANKA ATHTHNA (THORN APPLE) Most poisonous flowers/ stem/ fruit/ leaves/roots Fatal dose: 50-75 seeds Botanical Name: Datura stramonium Toxin: Belladonna alkaloids (atropine, hyoscine and hyoscyamine) CIRCUMSTANCES OF DATURA POISONING Stupefying purpose Mixed with cigarettes produce state of unconsciousness to facilitate robbery & rape mixed with sweets (gingerly) robbery & rape Accidental poisoning: Children Suicidal Homicidal : very rare DATURA POISONING SIGNS & SYMPTOMS Produce characteristic manifestations of anticholinergic poisoning Dryness of mouth Autopsy findings Dysphagia Seeds in stomach & non specific Dysarthria features Diplopia Dry hot and red skin Drowsiness leading to coma Urinary retention Death : respiratory failure or cardiac arrhythmia DIVI KADURU (EVE’S APPLE) Most poisonous / latex/ fruit/ seeds Botanical Name: Pagiy antha dicotoma Botanical Name: Tabernaemanta dicotoma Toxin: alkaloids/ strychnine SIGNS & SYMPTOMS OF DIVI KADURU POISONING White latex : inflammation of eye Ingestion : dryness of mucus membranes, thirst, dilataiton of pupils, rapid pulse, psychomotor disturbances, hallucinogenic effects. Autopsy findings Accidental poisonin g: Children Seeds in stomach & non specific Suicidal poisoning features GODA KADURU (BITTER NUT) Most poisonous: Seed (although all parts toxics) Fatal dose: 1-2 seeds Botanical Name: Strychnos nux vomica Toxin: alkaloids ( strychnine/ brucine) CIRCUMSTANCES OF GODA KADURU POISONING Strychnine injections are used to kill stray dogs/ -

Toxicology in Antiquity
TOXICOLOGY IN ANTIQUITY Other published books in the History of Toxicology and Environmental Health series Wexler, History of Toxicology and Environmental Health: Toxicology in Antiquity, Volume I, May 2014, 978-0-12-800045-8 Wexler, History of Toxicology and Environmental Health: Toxicology in Antiquity, Volume II, September 2014, 978-0-12-801506-3 Wexler, Toxicology in the Middle Ages and Renaissance, March 2017, 978-0-12-809554-6 Bobst, History of Risk Assessment in Toxicology, October 2017, 978-0-12-809532-4 Balls, et al., The History of Alternative Test Methods in Toxicology, October 2018, 978-0-12-813697-3 TOXICOLOGY IN ANTIQUITY SECOND EDITION Edited by PHILIP WEXLER Retired, National Library of Medicine’s (NLM) Toxicology and Environmental Health Information Program, Bethesda, MD, USA Academic Press is an imprint of Elsevier 125 London Wall, London EC2Y 5AS, United Kingdom 525 B Street, Suite 1650, San Diego, CA 92101, United States 50 Hampshire Street, 5th Floor, Cambridge, MA 02139, United States The Boulevard, Langford Lane, Kidlington, Oxford OX5 1GB, United Kingdom Copyright r 2019 Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). -
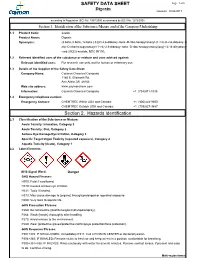
Digoxin SAFETY DATA SHEET Section 2. Hazards Identification
SAFETY DATA SHEET Page: 1 of 6 Digoxin Revision: 08/24/2017 according to Regulation (EC) No. 1907/2006 as amended by (EC) No. 1272/2008 Section 1. Identification of the Substance/Mixture and of the Company/Undertaking 1.1 Product Code: 22266 Product Name: Digoxin Synonyms: (3.beta.,5.beta.,12.beta.)-3-[(O-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl-(1->4)-O-2,6-dideoxy-.b eta.-D-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy- card-20(22)-enolide; NSC 95100; 1.2 Relevant identified uses of the substance or mixture and uses advised against: Relevant identified uses: For research use only, not for human or veterinary use. 1.3 Details of the Supplier of the Safety Data Sheet: Company Name: Cayman Chemical Company 1180 E. Ellsworth Rd. Ann Arbor, MI 48108 Web site address: www.caymanchem.com Information: Cayman Chemical Company +1 (734)971-3335 1.4 Emergency telephone number: Emergency Contact: CHEMTREC Within USA and Canada: +1 (800)424-9300 CHEMTREC Outside USA and Canada: +1 (703)527-3887 Section 2. Hazards Identification 2.1 Classification of the Substance or Mixture: Acute Toxicity: Inhalation, Category 3 Acute Toxicity: Oral, Category 2 Serious Eye Damage/Eye Irritation, Category 2 Specific Target Organ Toxicity (repeated exposure), Category 2 Aquatic Toxicity (Acute), Category 1 2.2 Label Elements: GHS Signal Word: Danger GHS Hazard Phrases: H300: Fatal if swallowed. H319: Causes serious eye irritation. H331: Toxic if inhaled. H373: May cause damage to {organs} through prolonged or repeated exposure. H400: Very toxic to aquatic life. -

Molecular Toxicology
EXS 99 Molecular, Clinical and Environmental Toxicology Volume 1: Molecular Toxicology Edited by Andreas Luch Birkhäuser Verlag Basel · Boston · Berlin Editor Andreas Luch Federal Institute for Risk Assessment Thielallee 88-92 14195 Berlin Germany Library of Congress Control Number: 2008938291 Bibliographic information published by Die Deutsche Bibliothek Die Deutsche Bibliothek lists this publication in the Deutsche Nationalbibliografie; detailed bibliographic data is available in the Internet at http://dnb.ddb.de ISBN 978-3-7643-8335-0 Birkhäuser Verlag AG, Basel – Boston – Berlin This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, re-use of illustrations, recitation, broad- casting, reproduction on microfilms or in other ways, and storage in data banks. For any kind of use, permission of the copyright owner must be obtained. The publisher and editor can give no guarantee for the information on drug dosage and administration contained in this publication. The respective user must check its accuracy by consulting other sources of reference in each individual case. The use of registered names, trademarks etc. in this publication, even if not identified as such, does not imply that they are exempt from the relevant protective laws and regulations or free for general use. © 2009 Birkhäuser Verlag AG Basel – Boston – Berlin P.O. Box 133, CH-4010 Basel, Switzerland Part of Springer Science+Business Media Printed on acid-free paper produced from chlorine-free pulp. TFC ∞ Cover illustration: with friendly permission of Andreas Luch Cover design: Benjamin Blankenburg, Basel, Switzerland Printed in Germany ISBN 978-3-7643-8335-0 e-ISBN 978-3-7643-8336-7 987654321 www. -

Digoxin Toxicity 1
Chronic Digoxin Toxicity Reviewers: Shawn M. Varney, Authors: Matthew Riddle, MD, Mel Otten, MD MD Target Audience: Emergency Medicine Residents (junior and senior level postgraduate learners), Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of digoxin toxicity 2. Order appropriate diagnostic studies for evaluation of digoxin toxicity 3. Appropriately interpret ECG 4. Administer digoxin-specific antibody fragments (DSFab) 5. Recognize acute kidney injury as a precipitating factor of toxicity, and treat acute kidney injury appropriately 6. Select an appropriate disposition for patient with digoxin toxicity Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Develop independent differential diagnosis in setting of leading information from the nurse 2. Describe the mechanism of digoxin toxicity and treatment, DSFab 3. Use appropriate dosing strategy for DSFab administration Critical actions checklist: 1. Order a basic metabolic panel 2. Order a digoxin level 3. Obtain ECG 4. Provide volume resuscitation for acute kidney injury 5. Administer digoxin antibody fragments 6. Consult Poison Center/Toxicologist 7. Admit to the MICU Environment: Emergency Department treatment area 1. Room Set Up – ED critical care area a. Manikin Set Up – Mid or high fidelity simulator b. Props – Standard ED equipment 2. Distractors – ED noise, alarming monitor For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background The setting is an urban emergency department. The patient is a 63-year-old male with a history of atrial fibrillation, HTN, and CHF brought to the emergency department by EMS for nausea and vomiting for the past four days and confusion that began shortly before arrival. PMHx: atrial fibrillation, HTN, and CHF PSHx: None Medications: ASA 81 mg once daily, Digoxin 250 mcg once daily, Amlodipine 10 mg once daily, Lasix 20 mg twice daily, warfarin 5 mg once daily Allergies: NKDA SocHx: smokes ½ ppd for 40 years.