Antidotes in Poisoning Binila Chacko1, John V Peter2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

Mapping the Dissociated Body
Lesley University DigitalCommons@Lesley Graduate School of Arts and Social Sciences Expressive Therapies Capstone Theses (GSASS) Spring 5-16-2020 Mapping the Dissociated Body Elizabeth Hough [email protected] Follow this and additional works at: https://digitalcommons.lesley.edu/expressive_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Hough, Elizabeth, "Mapping the Dissociated Body" (2020). Expressive Therapies Capstone Theses. 239. https://digitalcommons.lesley.edu/expressive_theses/239 This Thesis is brought to you for free and open access by the Graduate School of Arts and Social Sciences (GSASS) at DigitalCommons@Lesley. It has been accepted for inclusion in Expressive Therapies Capstone Theses by an authorized administrator of DigitalCommons@Lesley. For more information, please contact [email protected], [email protected]. Running Head: MAPPING THE DISSOCIATED BODY 1 Mapping the Dissociated Body Elizabeth Hough Lesley University Running Head: MAPPING THE DISSOCIATED BODY 2 Abstract This capstone thesis explored the use of body mapping and body scans as a tool for assessing and tracking somatic dissociation and embodiment. The researcher utilized a client- centered approach and mindfulness-based interventions and theory to ground the work with the clients. While there were a variety of questionnaire-based tools for assessing dissociation with clients, many of them were lacking in the somatic component of dissociation. The available assessments were also exclusively self-reported and written or verbal, which had the potential to result in biased reporting. Clients may have also struggled to identify their level of somatic dissociation due to an inherent disconnection or dismissal of their somatic experience. This research described two case studies in which body scans and body mapping were utilized as a method to assess and track the client’s level of body dissociation and embodiment. -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Report on the National Seminar on Radioimmunoassays Radiation Medicine Centre, B.A.R.C
REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16-20, 1978 RADIATION MEDICINE CENTRE, B.A.R.C. DEPARTMENT OF ATOMIC ENERGY AND WORLD HEALTH ORGANISATION REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16—20, 1978 RADIATION MEDICINE CENTRE, BARC TATA MEMORIAL HOSPITAL ANNEXE JERBAI WADIA ROAD, PAREL BOMBAY 400 012 ORGANISED UNDER THE AUSPICES OF THE DEPARTMENT OF ATOMIC ENERGY & WORLD HEALTH ORGANISATION CONTENTS Page Preface .. .. .. .. .. .. .. 3 Administrative Responsibilities .. .. .. .. 6 List of Participants 7 Programme .. .. .. .. .. .. .. 11 Basic Requirements of RIA in India .. .. .. 14 a. Radioisotopes for RIA's .. .. .. .. .. 15 b. Kits for RIA 17 c. Availability of Antibodies 19 d. National Pituitary Agency .. .. .. .. 20 e. Well-counter for RIA 21 f. Radiation Protection Aspects of RIA 23 Review of Discussion following the Session .. .. 26 State of Art of RIA's in India 28 Trigger Sessions 36 a. Quality Control of RIA's 37 b. Usefulness and limitations of RIA's in clinical diagnosis 39 c. RIA's in tropical diseases •. .. .. .. .. 42 d. Centralised assay services .. .. .. .. 44 Recommendations and Guidelines .. .. .. .. 46 Backword 51 Bibliography . .. .. .. .. .. .. 53 PREFACE This National Seminar on Radioimmunoassays was the second National Seminar jointly sponsored by Department of Atomic Energy and World Health Organisation and organised at Radiation Medicine Centre. The first one on 'Nuclear Medicine in India' was held in December 1976. The present Seminar on Radioimmunoassays was distinguished by the participation of Dr. Rosalyn Yalow, Nobel Laureate in Medicine for 1977. She, along with Dr. Solomon A. Berson, discovered the technique of Radioimmunoassay and nurtured it through the early years with hard and meticulous work to establish its usefulness in medical science. -

XELJANZ (Tofacitinib)
HIGHLIGHTS OF PRESCRIBING INFORMATION Psoriatic Arthritis (in combination with nonbiologic DMARDs) These highlights do not include all the information needed to use XELJANZ 5 mg twice daily or XELJANZ XR 11 mg once daily. (2.2) XELJANZ/XELJANZ XR safely and effectively. See full prescribing Recommended dosage in patients with moderate and severe renal information for XELJANZ. impairment or moderate hepatic impairment is XELJANZ 5 mg once daily. (2, 8.7, 8.8) ® XELJANZ (tofacitinib) tablets, for oral use Ulcerative Colitis ® XELJANZ XR (tofacitinib) extended-release tablets, for oral use XELJANZ 10 mg twice daily for at least 8 weeks; then 5 or 10 mg Initial U.S. Approval: 2012 twice daily. Discontinue after 16 weeks of 10 mg twice daily, if adequate therapeutic benefit is not achieved. Use the lowest effective dose to WARNING: SERIOUS INFECTIONS AND MALIGNANCY maintain response. (2.3) See full prescribing information for complete boxed warning. Recommended dosage in patients with moderate and severe renal impairment or moderate hepatic impairment: half the total daily dosage Serious infections leading to hospitalization or death, including recommended for patients with normal renal and hepatic function. (2, 8.7, tuberculosis and bacterial, invasive fungal, viral, and other 8.8) opportunistic infections, have occurred in patients receiving Dosage Adjustment XELJANZ. (5.1) See the full prescribing information for dosage adjustments by indication If a serious infection develops, interrupt XELJANZ/XELJANZ XR for patients receiving CYP2C19 and/or CYP3A4 inhibitors; in patients until the infection is controlled. (5.1) with moderate or severe renal impairment or moderate hepatic Prior to starting XELJANZ/XELJANZ XR, perform a test for latent impairment; and patients with lymphopenia, neutropenia, or anemia. -

1: Gastro-Intestinal System
1 1: GASTRO-INTESTINAL SYSTEM Antacids .......................................................... 1 Stimulant laxatives ...................................46 Compound alginate products .................. 3 Docuate sodium .......................................49 Simeticone ................................................... 4 Lactulose ....................................................50 Antimuscarinics .......................................... 5 Macrogols (polyethylene glycols) ..........51 Glycopyrronium .......................................13 Magnesium salts ........................................53 Hyoscine butylbromide ...........................16 Rectal products for constipation ..........55 Hyoscine hydrobromide .........................19 Products for haemorrhoids .................56 Propantheline ............................................21 Pancreatin ...................................................58 Orphenadrine ...........................................23 Prokinetics ..................................................24 Quick Clinical Guides: H2-receptor antagonists .......................27 Death rattle (noisy rattling breathing) 12 Proton pump inhibitors ........................30 Opioid-induced constipation .................42 Loperamide ................................................35 Bowel management in paraplegia Laxatives ......................................................38 and tetraplegia .....................................44 Ispaghula (Psyllium husk) ........................45 ANTACIDS Indications: -
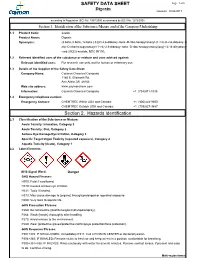
Digoxin SAFETY DATA SHEET Section 2. Hazards Identification
SAFETY DATA SHEET Page: 1 of 6 Digoxin Revision: 08/24/2017 according to Regulation (EC) No. 1907/2006 as amended by (EC) No. 1272/2008 Section 1. Identification of the Substance/Mixture and of the Company/Undertaking 1.1 Product Code: 22266 Product Name: Digoxin Synonyms: (3.beta.,5.beta.,12.beta.)-3-[(O-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl-(1->4)-O-2,6-dideoxy-.b eta.-D-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy- card-20(22)-enolide; NSC 95100; 1.2 Relevant identified uses of the substance or mixture and uses advised against: Relevant identified uses: For research use only, not for human or veterinary use. 1.3 Details of the Supplier of the Safety Data Sheet: Company Name: Cayman Chemical Company 1180 E. Ellsworth Rd. Ann Arbor, MI 48108 Web site address: www.caymanchem.com Information: Cayman Chemical Company +1 (734)971-3335 1.4 Emergency telephone number: Emergency Contact: CHEMTREC Within USA and Canada: +1 (800)424-9300 CHEMTREC Outside USA and Canada: +1 (703)527-3887 Section 2. Hazards Identification 2.1 Classification of the Substance or Mixture: Acute Toxicity: Inhalation, Category 3 Acute Toxicity: Oral, Category 2 Serious Eye Damage/Eye Irritation, Category 2 Specific Target Organ Toxicity (repeated exposure), Category 2 Aquatic Toxicity (Acute), Category 1 2.2 Label Elements: GHS Signal Word: Danger GHS Hazard Phrases: H300: Fatal if swallowed. H319: Causes serious eye irritation. H331: Toxic if inhaled. H373: May cause damage to {organs} through prolonged or repeated exposure. H400: Very toxic to aquatic life. -

Examining the Therapist's Internal Experience When a Patient Dissociates in Session
University of Pennsylvania ScholarlyCommons Doctorate in Social Work (DSW) Dissertations School of Social Policy and Practice Spring 5-13-2013 Do You Know What I Know? Examining the Therapist's Internal Experience when a Patient Dissociates in Session Jacqueline R. Strait University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/edissertations_sp2 Part of the Psychology Commons, and the Social Work Commons Recommended Citation Strait, Jacqueline R., "Do You Know What I Know? Examining the Therapist's Internal Experience when a Patient Dissociates in Session" (2013). Doctorate in Social Work (DSW) Dissertations. 36. https://repository.upenn.edu/edissertations_sp2/36 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/edissertations_sp2/36 For more information, please contact [email protected]. Do You Know What I Know? Examining the Therapist's Internal Experience when a Patient Dissociates in Session Abstract There is rich theoretical literature that cites the importance of the therapist’s use of self as a way of knowing, especially in cases where a patient has been severely traumatized in early life. There is limited empirical research that explores the in-session experience of therapists working with traumatized patients in order to support these claims. This study employed a qualitative design to explore a therapist’s internal experience when a patient dissociates in session. The aim of this study was to further develop the theoretical construct of dissociative attunement to explain the way that therapist and patient engage in a nonverbal process of synchronicity that has the potential to communicate dissociated images, affect or somatosensory experiences by way of the therapist’s internal experience. -

Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com
Hallucinogens And Dissociative Drug Use And Addiction Introduction Hallucinogens are a diverse group of drugs that cause alterations in perception, thought, or mood. This heterogeneous group has compounds with different chemical structures, different mechanisms of action, and different adverse effects. Despite their description, most hallucinogens do not consistently cause hallucinations. The drugs are more likely to cause changes in mood or in thought than actual hallucinations. Hallucinogenic substances that form naturally have been used worldwide for millennia to induce altered states for religious or spiritual purposes. While these practices still exist, the more common use of hallucinogens today involves the recreational use of synthetic hallucinogens. Hallucinogen And Dissociative Drug Toxicity Hallucinogens comprise a collection of compounds that are used to induce hallucinations or alterations of consciousness. Hallucinogens are drugs that cause alteration of visual, auditory, or tactile perceptions; they are also referred to as a class of drugs that cause alteration of thought and emotion. Hallucinogens disrupt a person’s ability to think and communicate effectively. Hallucinations are defined as false sensations that have no basis in reality: The sensory experience is not actually there. The term “hallucinogen” is slightly misleading because hallucinogens do not consistently cause hallucinations. 1 ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com How hallucinogens cause alterations in a person’s sensory experience is not entirely understood. Hallucinogens work, at least in part, by disrupting communication between neurotransmitter systems throughout the body including those that regulate sleep, hunger, sexual behavior and muscle control. Patients under the influence of hallucinogens may show a wide range of unusual and often sudden, volatile behaviors with the potential to rapidly fluctuate from a relaxed, euphoric state to one of extreme agitation and aggression. -

Pharmacology/Therapeutics II Block I Lectures – 2013‐14
Pharmacology/Therapeutics II Block I Lectures – 2013‐14 54. H2 Blocker, PPls – Patel 55. Principles of Clinical Toxicology – Kennedy 56. Anti‐Parasitic Agents – Johnson (To be posted later) 57. Palliation of Constipation & Nausea/vomiting – Kristopaitis (Lecture in Room 190) Tarun B. Patel, Ph.D Date: January 9, 2013: 10:30 a.m. Reading Assignment: Katzung, Basic and Clinical Pharmacology, 11th Edition, pp. 1067-1077. KEY CONCEPTS AND LEARNING OBJECTIVES Histamine via its different receptors produces a number of physiological and pathological actions. Therefore, anti-histaminergic drugs may be used to treat different conditions. 1. To know the physiological functions of histamine. 2. To understand which histamine receptors mediate the different effects of histamine in stomach ulcers. 3. To know what stimuli cause the release of histamine and acid in stomach. 4. To know the types of histamine H2 receptor antagonists that are available clinically. 5. To know the clinical uses of H2 receptor antagonists. 6. To know the drug interactions associated with the use of H2 receptor antagonists. 7. To understand the mechanism of action of PPIs 8. To know the adverse effects and drugs interactions with PPIs 9. To know the role of H. pylori in gastric ulceration 10. To know the drugs used to treat H. pylori infection Drug List: See Summary Table Provided at end of handout. Page 1 Tarun B. Patel, Ph.D Histamine H2 receptor antagonists and PPIs in the treatment of GI Ulcers: The following section covers medicines used to treat ulcer. These medicines include H2 receptor antagonists, proton pump inhibitors, mucosal protective agents and antibiotics (for treatment of H. -

Digoxin Toxicity 1
Chronic Digoxin Toxicity Reviewers: Shawn M. Varney, Authors: Matthew Riddle, MD, Mel Otten, MD MD Target Audience: Emergency Medicine Residents (junior and senior level postgraduate learners), Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of digoxin toxicity 2. Order appropriate diagnostic studies for evaluation of digoxin toxicity 3. Appropriately interpret ECG 4. Administer digoxin-specific antibody fragments (DSFab) 5. Recognize acute kidney injury as a precipitating factor of toxicity, and treat acute kidney injury appropriately 6. Select an appropriate disposition for patient with digoxin toxicity Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Develop independent differential diagnosis in setting of leading information from the nurse 2. Describe the mechanism of digoxin toxicity and treatment, DSFab 3. Use appropriate dosing strategy for DSFab administration Critical actions checklist: 1. Order a basic metabolic panel 2. Order a digoxin level 3. Obtain ECG 4. Provide volume resuscitation for acute kidney injury 5. Administer digoxin antibody fragments 6. Consult Poison Center/Toxicologist 7. Admit to the MICU Environment: Emergency Department treatment area 1. Room Set Up – ED critical care area a. Manikin Set Up – Mid or high fidelity simulator b. Props – Standard ED equipment 2. Distractors – ED noise, alarming monitor For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background The setting is an urban emergency department. The patient is a 63-year-old male with a history of atrial fibrillation, HTN, and CHF brought to the emergency department by EMS for nausea and vomiting for the past four days and confusion that began shortly before arrival. PMHx: atrial fibrillation, HTN, and CHF PSHx: None Medications: ASA 81 mg once daily, Digoxin 250 mcg once daily, Amlodipine 10 mg once daily, Lasix 20 mg twice daily, warfarin 5 mg once daily Allergies: NKDA SocHx: smokes ½ ppd for 40 years. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves.