Acute Periodontal Lesions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report Abstract Hereditary gingival fibromatosis (HGF) is a rare condition characterized by varying degrees of gingival hyperplasia. Gingival fibromatosis usually occurs as an isolated disorder or can be associated with a variety of other syndromes. A 33-year-old male patient who had a generalized severe gingival overgrowth covering two thirds of almost all maxillary and mandibular teeth is reported. A mucoperiosteal flap was performed using interdental and crevicular incisions to remove excess gingival tissues and an internal bevel incision to reflect flaps. The patient was treated 15 years ago in the same clinical facility using the same treatment strategy. There was no recurrence one year following the most recent surgery. Keywords: Gingival hyperplasia, hereditary gingival hyperplasia, HGF, hereditary disease, therapy, mucoperiostal flap Citation: S¸engün D, Hatipog˘lu H, Hatipog˘lu MG. Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report. J Contemp Dent Pract 2007 January;(8)1:090-096. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 8, No. 1, January 1, 2007 Introduction Hereditary gingival fibromatosis (HGF), also Ankara, Turkey with a complaint of recurrent known as elephantiasis gingiva, hereditary generalized gingival overgrowth. The patient gingival hyperplasia, idiopathic fibromatosis, had presented himself for examination at the and hypertrophied gingival, is a rare condition same clinic with the same complaint 15 years (1:750000)1 which can present as an isolated ago. At that time, he was treated with full-mouth disorder or more rarely as a syndrome periodontal surgery after the diagnosis of HGF component.2,3 This condition is characterized by had been made following clinical and histological a slow and progressive enlargement of both the examination (Figures 1 A-B). -

ABC of Oral Health Periodontal Disease John Coventry, Gareth Griffiths, Crispian Scully, Maurizio Tonetti
Clinical review ABC of oral health Periodontal disease John Coventry, Gareth Griffiths, Crispian Scully, Maurizio Tonetti Most periodontal disease arises from, or is aggravated by, accumulation of plaque, and periodontitis is associated particularly with anaerobes such as Porphyromonas gingivalis, Bacteroides forsythus, and Actinobacillus actinomycetemcomitans. Calculus (tartar) may form from calcification of plaque above or below the gum line, and the plaque that collects on calculus exacerbates the inflammation. The inflammatory reaction is associated with progressive loss of periodontal ligament and alveolar bone and, eventually, with mobility and loss of teeth. Periodontal diseases are ecogenetic in the sense that, in subjects rendered susceptible by genetic or environmental factors (such as polymorphisms in the gene for interleukin 1, cigarette smoking, immune depression, and diabetes), the infection leads to more rapidly progressive disease. Osteoporosis also seems to have some effect on periodontal bone loss. The possible effects of periodontal disease on systemic Chronic marginal gingivitis showing erythematous oedematous appearance health, via pro-inflammatory cytokines, have been the focus of much attention. Studies to test the strength of associations with atherosclerosis, hypertension, coronary heart disease, cerebrovascular disease, and low birth weight, and any effects on diabetic control, are ongoing. Gingivitis Chronic gingivitis to some degree affects over 90% of the population. If treated, the prognosis is good, but otherwise it may progress to periodontitis and tooth mobility and loss. Marginal gingivitis is painless but may manifest with bleeding from the gingival crevice, particularly when brushing the teeth. The gingival margins are slightly red and swollen, eventually with mild gingival hyperplasia. Management—Unless plaque is assiduously removed and Gingivitis with hyperplasia kept under control by tooth brushing and flossing and, where necessary, by removal of calculus by scaling and polishing by dental staff, the condition will recur. -

Management of Acute Periodontal Abscess Mimicking Acute Apical Abscess in the Anterior Lingual Region: a Case Report
Open Access Case Report DOI: 10.7759/cureus.5592 Management of Acute Periodontal Abscess Mimicking Acute Apical Abscess in the Anterior Lingual Region: A Case Report Omar A. Alharbi 1 , Muhammad Zubair Ahmad 1 , Atif S. Agwan 1 , Durre Sadaf 1 1. Conservative Dentistry, Qassim University, College of Dentistry, Buraydha, SAU Corresponding author: Muhammad Zubair Ahmad, [email protected] Abstract Purulent infections of periodontal tissues are known as periodontal abscesses localized to the region of the involved tooth. Due to the high prevalence rate and aggressive symptoms, it is considered a dental emergency; urgent care is mandatory to maintain the overall health and well being of the patient. This case report describes the management of a patient who presented with an acute periodontal abscess secondary to poor oral hygiene. Clinically and radiographically, the lesion was mimicking an acute apical abscess secondary to pulpal necrosis. Periodontal treatment was started after completion of antibiotic therapy. The clinical presentation of the condition and results of the recovery, along with a brief review of relevant literature are discussed. Categories: Pain Management, Miscellaneous, Dentistry Keywords: periodontal abscess, antimicrobial agents, dental pulp test, dental pulp necrosis, apical suppurative periodontitis Introduction Periodontium, as a general term, describes the tissues surrounding and supporting the tooth structure. A localized purulent infection of the periodontal tissues adjacent to a periodontal pocket, also known as a periodontal abscess, is a frequently encountered periodontal condition that may be characterized by the rapid destruction of periodontal tissues [1-2]. The symptoms generally involve severe pain, swelling of the alveolar mucosa or gingiva, a reddish blue or red appearance of the affected tissues, and difficulty in chewing [1-3]. -
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
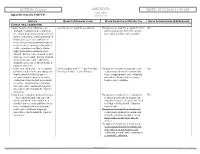
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief
Scottish Dental SD Clinical Effectiveness Programme cep Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief June 2014 Scottish Dental SD Clinical Effectiveness Programme cep The Scottish Dental Clinical Effectiveness Programme (SDCEP) is an initiative of the National Dental Advisory Committee (NDAC) in partnership with NHS Education for Scotland. The Programme provides user-friendly, evidence-based guidance on topics identified as priorities for oral health care. SDCEP guidance aims to support improvements in patient care by bringing together, in a structured manner, the best available information that is relevant to the topic and presenting this information in a form that can be interpreted easily and implemented. Supporting the provision of safe, effective, person-centred care Scottish Dental SD Clinical Effectiveness Programme cep Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief June 2014 Prevention and Treatment of Periodontal Diseases in Primary Care Cover image: Colour-enhanced photomicrograph of oral bacterial colonies growing on an agar plate. Derren Ready, Wellcome Images. © Scottish Dental Clinical Effectiveness Programme SDCEP operates within NHS Education for Scotland. You may copy or reproduce the information in this document for use within NHS Scotland and for non-commercial educational purposes. Use of this document for commercial purposes is permitted only with written permission. ISBN 978 1 905829 18 7 Published June 2014 Scottish Dental Clinical Effectiveness Programme Dundee Dental Education Centre, Frankland Building, Small’s Wynd, Dundee DD1 4HN Email [email protected] Tel 01382 425751 / 425771 Website www.sdcep.org.uk Prevention and Treatment of Periodontal Diseases in Primary Care Introduction Prevention and Treatment of Periodontal Diseases in Primary Care is designed to assist and support primary care dental teams in providing appropriate care for patients both at risk of and with periodontal diseases. -

National Standardized Dental Claim Utilization Review Criteria
NATIONAL STANDARDIZED DENTAL CLAIM UTILIZATION REVIEW CRITERIA Revised: 4/1/2017 The following Dental Clinical Policies, Dental Coverage Guidelines, and dental criteria are designed to provide guidance for the adjudication of claims or prior authorization requests by the clinical dental consultant. The consultant should use these guidelines in conjunction with clinical judgment and any unique circumstances that accompany a request for coverage. Specific plan coverage, exclusions or limitations may supersede these criteria. For reference, criteria approved by the Clinical Policy and Technology Committee are provided. These represent clinical guidelines that are evidence-based. Please Note: Links to the specific Dental Clinical Policies and Dental Coverage Guidelines are embedded in this document. Additionally, for notices of new and updated Dental Clinical Policies and Coverage Guidelines or for a full listing of Dental Clinical Policies and Coverage Guidelines, refer to UnitedHealthcareOnline.com > Tools & Resources > Policies, Protocols and Guides > Dental Clinical Policies & Coverage Guidelines. CLAIM UR CRITERIA / DENTAL CLINICAL POLICY / DENTAL PROCEDURE DOCUMENTATION COVERAGE GUIDELINE DIAGNOSTIC Clinical Oral Evaluations Documentation in member record that includes all services performed D0120–D0191 for the code submitted Pre-Diagnostic Services Documentation in member record that includes all services performed D0190 screening of a patient for the code submitted. D0191 assessment of a patient Diagnostic Imaging Documentation in the member record. Diagnostic, clear, readable Criteria for codes D0364–D0368, D0380–D0386, D0391–D0395: images, dated with member name. Image capture with interpretation Cone beam computed tomography (CBCT) is unproven and not medically D0210–D0371 necessary for routine dental applications. There is insufficient evidence that CBCT is beneficial for use in routine dental Image Capture only applications. -

Diagnosis and Treatment of Periodontal Emergencies
PERIODONTAL Dr. Nazli Rabienejad DDS,MSc; Periodontist Assistant professor of Hamadan Dentistry faculty viral shedding may begin 5–6 days before the appearance of the first symptoms. Pre symptomatic carriers are difficult to identify viral load is shown to be the highest at the time of symptom onset any person who enters may be a potential source of transmission Dr. Nazli Rabienejad 3 Dr. Nazli Rabienejad 4 Dr. Nazli Rabienejad 5 انتقال حین درمان های دندانپزشکی دراپلت بزاقی دراپلت تنفسی آئروسل Dr. Nazli Rabienejad موارد اورژانس و ضروری در ارائه خدمات دندانپزشکی در شرایط همه گیری کووید19- تسکین درد کنترل خونریزی بیمار خطر برای کنترل عفونت سﻻمتی Dr. Nazli Rabienejad 7 Dr. Nazli Rabienejad Dr. Nazli Rabienejad Dr. Nazli Rabienejad PERIODONTAL EMERGENCIES 1. Pericoronitis 2. Periodontal and gingival abscess 3. Chemical and physical injuries 4. Acute herpetic gingivostomatitis 5. Necrotizing ulcerative gingivitis 6. Cracked tooth syndrome 7. Periodontic and endodontic problems 8. Dentine hypersensitivity Dr. Nazli Rabienejad 11 Classification of Abscesses • marginal gingival and interdental tissues gingival abscess • periodontal pocket periodontal abscess • crown of a partially erupted tooth. Pericoronal abscess Dr. Nazli Rabienejad 12 Pericoronal Abscess (pericoronitis) • Most common periodontal emergency • inflammation of the soft tissue operculum, which covers a partially erupted tooth. • most often observed around the mandibular third molars Dr. Nazli Rabienejad 13 The clinical picture of pericoronitis • red, swollen, possibly suppurative lesion that is extremely painful to touch. • Swelling of the cheek at the angle of jaw, partial trismus, and radiating pain to ear and systemic complications such as fever, leukocytosis and general malaise are common findings. -

Chronic Inflammatory Gingival Enlargement and Treatment: a Case Report
Case Report Adv Dent & Oral Health Volume 9 Issue 4- July 2018 Copyright © All rights are reserved by Mehmet Özgöz DOI: 10.19080/ADOH.2018.09.555766 Chronic Inflammatory Gingival Enlargement and Treatment: A Case Report Mehmet Özgöz1* and Taner Arabaci2 1Department of Periodontology, Akdeniz University, Turkey 2Department of Periodontology, Atatürk University, Turkey Submission: June 14, 2018; Published: July 18, 2018 *Corresponding author: Özgöz, Department of Periodontology, Akdeniz University Faculty of Dentistry, Antalya, Turkey, Fax:+902423106967; Email: Abstract Gingival enlargement is a common feature in gingival disease. If gingival enlargement isn’t treated, it may some aesthetic problems, plaque accumulation,Keywords: Gingival gingival enlargement; bleeding, and Periodontal periodontitis. treatments; In this paper, Etiological inflammatory factors; Plasma gingival cell enlargement gingivitis and treatment was presented. Introduction and retention include poor oral hygiene, abnormal relationship of Gingival enlargement is a common feature in gingival disease adjacent teeth, lack of tooth function, cervical cavities, improperly contoured dental restorations, food impaction, nasal obstruction, connection with etiological factors and pathological changes [3-5]. [1,2]. Many types of gingival enlargement can be classified in orthodontic therapy involving repositioning of the teeth, and habits such as mouth breathing and pressing the tongue against the gingival [18-20]. a)b) InflammatoryDrug-induced enlargement:enlargement [7-12]. chronic and acute [6]. c) Gingival enlargements associated with systemic diseases: patients to maintain oral hygiene [9,21]. Surgical correction of Overgrowth of the gingival tissue makes it more difficult for i. Conditioned enlargement (pregnancy, puberty, vitamin the gingival overgrowth is still the most frequent treatment. Such treatment is only advocated when the overgrowth is severe. -

SAID 2010 Literature Review (Articles from 2009)
2010 Literature Review (SAID’s Search of Dental Literature Published in Calendar Year 2009*) SAID Special Care Advocates in Dentistry Recent journal articles related to oral health care for people with mental and physical disabilities. Search Program = PubMed Database = Medline Journal Subset = Dental Publication Timeframe = Calendar Year 2009* Language = English SAID Search-Term Results 6,552 Initial Selection Results = 521 articles Final Selected Results = 151 articles Compiled by Robert G. Henry, DMD, MPH *NOTE: The American Dental Association is responsible for entering journal articles into the National Library of Medicine database; however, some articles are not entered in a timely manner. Some articles are entered years after they were published and some are never entered. 1 SAID Search-Terms Employed: 1. Mental retardation 21. Protective devices 2. Mental deficiency 22. Conscious sedation 3. Mental disorders 23. Analgesia 4. Mental health 24. Anesthesia 5. Mental illness 25. Dental anxiety 6. Dental care for disabled 26. Nitrous oxide 7. Dental care for chronically ill 27. Gingival hyperplasia 8. Self-mutilation 28. Gingival hypertrophy 9. Disabled 29. Glossectomy 10. Behavior management 30. Sialorrhea 11. Behavior modification 31. Bruxism 12. Behavior therapy 32. Deglutition disorders 13. Cognitive therapy 33. Community dentistry 14. Down syndrome 34. State dentistry 15. Cerebral palsy 35. Gagging 16. Epilepsy 36. Substance abuse 17. Enteral nutrition 37. Syndromes 18. Physical restraint 38. Tooth brushing 19. Immobilization 39. Pharmaceutical preparations 20. Pediatric dentistry 40. Public health dentistry Program: EndNote X3 used to organize search and provide abstract. Copyright 2009 Thomson Reuters, Version X3 for Windows. Categories and Highlights: A. Mental Issues (1-5) F. -

Generalized Aggressive Periodontitis Associated with Plasma Cell Gingivitis Lesion: a Case Report and Non-Surgical Treatment
Clinical Advances in Periodontics; Copyright 2013 DOI: 10.1902/cap.2013.130050 Generalized Aggressive Periodontitis Associated With Plasma Cell Gingivitis Lesion: A Case Report and Non-Surgical Treatment * Andreas O. Parashis, Emmanouil Vardas, † Konstantinos Tosios, ‡ * Private practice limited to Periodontics, Athens, Greece; and, Department of Periodontology, School of Dental Medicine, Tufts University, Boston, MA, United States of America. †Clinic of Hospital Dentistry, Dental Oncology Unit, University of Athens, Greece. ‡ Private practice limited to Oral Pathology, Athens, Greece. Introduction: Plasma cell gingivitis (PCG) is an unusual inflammatory condition characterized by dense, band-like polyclonal plasmacytic infiltration of the lamina propria. Clinically, appears as gingival enlargement with erythema and swelling of the attached and free gingiva, and is not associated with any loss of attachment. The aim of this report is to present a rare case of severe generalized aggressive periodontitis (GAP) associated with a PCG lesion that was successfully treated and maintained non-surgically. Case presentation: A 32-year-old white male with a non-contributory medical history presented with gingival enlargement with diffuse erythema and edematous swelling, predominantly around teeth #5-8. Clinical and radiographic examination revealed generalized severe periodontal destruction. A complete blood count and biochemical tests were within normal limits. Histological and immunohistochemical examination were consistent with PCG. A diagnosis of severe GAP associated with a PCG lesion was assigned. Treatment included elimination of possible allergens and non- surgical periodontal treatment in combination with azithromycin. Clinical examination at re-evaluation revealed complete resolution of gingival enlargement, erythema and edema and localized residual probing depths 5 mm. One year post-treatment the clinical condition was stable.