Addressing the 'C' in Aces Webinar Transcript
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Young-Voices-2019.Pdf
2019 young voices /youngvoices The Beast Within Cathy Lu, 17 welcome to young voices 2019 GET PUBLISHED! The writing and art in this magazine was created by in Young Voices 2020 talented young people from all across Toronto. Love what you’re reading here? Their humour, compassion, anger and intelligence Want to be part of it? make these pages crackle and shine. Whether their Submit stories, poems, rants, pieces are about technology, racism, nature, despair, or artwork, comics, photos... love, their expression is clear, passionate and original. Making art is often a solitary pursuit, and for many Submit NOW! See page 79 for details. writers and artists in this magazine, this is the first time they’ve shared their work with a broad audience. As the audience, you’ll find poems and photos, drawings and essays that will challenge you to see the world from Cover Art by new perspectives and maybe inspire you to make your Alicia Tian, 17 own voice heard. All the pieces in the magazine were selected by teens working with professional writer/artist mentors on editorial teams. A big thank you to them all for the thoughtfulness and care they brought to their work. The Young Voices 2019 editorial board: Lillian Allen Mahak Jain Jareeat Purnava Rishona Altenberg Juanita Lam Ken Sparling Zawadi Bunzigiye Olivia Li Phoebe Tsang Leia Kook Chen Wenting Li Patrick Walters Kathryn Dou Barton Lu Chloe Xuan Bessa Fan Furqan Mohamed Maria Yang Lucy Haughton Sachiko Murakami Rain YeYang Monidipa Nath The Young Voices program is supported through the generosity of the Daniels brothers in honour of their mother, Norine Rose, and the Friends of Toronto Public Library, South Chapter. -

Tolono Library CD List
Tolono Library CD List CD# Title of CD Artist Category 1 MUCH AFRAID JARS OF CLAY CG CHRISTIAN/GOSPEL 2 FRESH HORSES GARTH BROOOKS CO COUNTRY 3 MI REFLEJO CHRISTINA AGUILERA PO POP 4 CONGRATULATIONS I'M SORRY GIN BLOSSOMS RO ROCK 5 PRIMARY COLORS SOUNDTRACK SO SOUNDTRACK 6 CHILDREN'S FAVORITES 3 DISNEY RECORDS CH CHILDREN 7 AUTOMATIC FOR THE PEOPLE R.E.M. AL ALTERNATIVE 8 LIVE AT THE ACROPOLIS YANNI IN INSTRUMENTAL 9 ROOTS AND WINGS JAMES BONAMY CO 10 NOTORIOUS CONFEDERATE RAILROAD CO 11 IV DIAMOND RIO CO 12 ALONE IN HIS PRESENCE CECE WINANS CG 13 BROWN SUGAR D'ANGELO RA RAP 14 WILD ANGELS MARTINA MCBRIDE CO 15 CMT PRESENTS MOST WANTED VOLUME 1 VARIOUS CO 16 LOUIS ARMSTRONG LOUIS ARMSTRONG JB JAZZ/BIG BAND 17 LOUIS ARMSTRONG & HIS HOT 5 & HOT 7 LOUIS ARMSTRONG JB 18 MARTINA MARTINA MCBRIDE CO 19 FREE AT LAST DC TALK CG 20 PLACIDO DOMINGO PLACIDO DOMINGO CL CLASSICAL 21 1979 SMASHING PUMPKINS RO ROCK 22 STEADY ON POINT OF GRACE CG 23 NEON BALLROOM SILVERCHAIR RO 24 LOVE LESSONS TRACY BYRD CO 26 YOU GOTTA LOVE THAT NEAL MCCOY CO 27 SHELTER GARY CHAPMAN CG 28 HAVE YOU FORGOTTEN WORLEY, DARRYL CO 29 A THOUSAND MEMORIES RHETT AKINS CO 30 HUNTER JENNIFER WARNES PO 31 UPFRONT DAVID SANBORN IN 32 TWO ROOMS ELTON JOHN & BERNIE TAUPIN RO 33 SEAL SEAL PO 34 FULL MOON FEVER TOM PETTY RO 35 JARS OF CLAY JARS OF CLAY CG 36 FAIRWEATHER JOHNSON HOOTIE AND THE BLOWFISH RO 37 A DAY IN THE LIFE ERIC BENET PO 38 IN THE MOOD FOR X-MAS MULTIPLE MUSICIANS HO HOLIDAY 39 GRUMPIER OLD MEN SOUNDTRACK SO 40 TO THE FAITHFUL DEPARTED CRANBERRIES PO 41 OLIVER AND COMPANY SOUNDTRACK SO 42 DOWN ON THE UPSIDE SOUND GARDEN RO 43 SONGS FOR THE ARISTOCATS DISNEY RECORDS CH 44 WHATCHA LOOKIN 4 KIRK FRANKLIN & THE FAMILY CG 45 PURE ATTRACTION KATHY TROCCOLI CG 46 Tolono Library CD List 47 BOBBY BOBBY BROWN RO 48 UNFORGETTABLE NATALIE COLE PO 49 HOMEBASE D.J. -
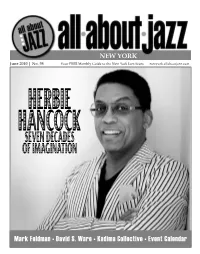
June 2010 Issue
NEW YORK June 2010 | No. 98 Your FREE Monthly Guide to the New York Jazz Scene newyork.allaboutjazz.com HERBIE HANCOCKSEVEN DECADES OF IMAGINATION Mark Feldman • David S. Ware • Kadima Collective • Event Calendar NEW YORK Despite the burgeoning reputations of other cities, New York still remains the jazz capital of the world, if only for sheer volume. A night in NYC is a month, if not more, anywhere else - an astonishing amount of music packed in its 305 square miles (Manhattan only 34 of those!). This is normal for the city but this month, there’s even more, seams bursting with amazing concerts. New York@Night Summer is traditionally festival season but never in recent memory have 4 there been so many happening all at once. We welcome back impresario George Interview: Mark Feldman Wein (Megaphone) and his annual celebration after a year’s absence, now (and by Sean Fitzell hopefully for a long time to come) sponsored by CareFusion and featuring the 6 70th Birthday Celebration of Herbie Hancock (On The Cover). Then there’s the Artist Feature: David S. Ware always-compelling Vision Festival, its 15th edition expanded this year to 11 days 7 by Martin Longley at 7 venues, including the groups of saxophonist David S. Ware (Artist Profile), drummer Muhammad Ali (Encore) and roster members of Kadima Collective On The Cover: Herbie Hancock (Label Spotlight). And based on the success of the WinterJazz Fest, a warmer 9 by Andrey Henkin edition, eerily titled the Undead Jazz Festival, invades the West Village for two days with dozens of bands June. -

The Case of Imposed Identity for Multiracial Individuals
YOUR PERCEPTION, MY REALITY: THE CASE OF IMPOSED IDENTITY FOR MULTIRACIAL INDIVIDUALS A Dissertation by NICHOLE CRYSTELL BOUTTÉ-HEINILUOMA Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY August 2012 Major Subject: Sociology Your Perception, My Reality: The Case of Imposed Identity for Multiracial Individuals Copyright 2012 Nichole Crystell Boutté-Heiniluoma YOUR PERCEPTION, MY REALITY: THE CASE OF IMPOSED IDENTITY FOR MULTIRACIAL INDIVIDUALS A Dissertation by NICHOLE CRYSTELL BOUTTÉ-HEINILUOMA Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY Approved by: Chair of Committee, Joe Feagin Committee Members, Sarah Gatson Alex McIntosh Jane Sell Head of Department, Jane Sell August 2012 Major Subject: Sociology iii ABSTRACT Your Perception, My Reality: The Case of Imposed Identity for Multiracial Individuals. (August 2012) Nichole Crystell Boutté-Heiniluoma, B.A., Texas A&M University; M.I.A., Texas A&M University Chair of Advisory Committee: Dr. Joe Feagin Prior to this exploratory study, issues of multiracial identity development and imposed identity had not been explored in great detail. This study sought to expand the current knowledge base by offering an examination of a) multiracial identity development for different bi/multiracial backgrounds, b) the influence of the perception of race on social interactions (imposed identity), and c) racial identification in the public and private spheres from the perspective of multi-racial individuals. A literature based survey was developed and piloted with an expert panel to increase face and content validity. -

2020 PRODUCT CATALOG 2 Call Sales Support at 800-325-7354 Page 04 Introduction TABLE 06 PRE-PEN® (Benzylpenicilloyl Polylysine Injection USP)
2020 PRODUCT CATALOG 2 Call Sales Support at 800-325-7354 page 04 Introduction TABLE 06 PRE-PEN® (benzylpenicilloyl polylysine injection USP) 07 Center-Al® (allergenic extract, alum precipitated) OF 08 Sublingual Immunotherapy Tablets 09 ODACTRA® CONTENTS 10 GRASTEK® 11 RAGWITEK® 12 Allergen Extracts 13 Pollen Extracts 16 Pollen Mixes 17 Molds 17 Smuts 18 Insects 18 Epidermals 19 Foods/Ingestants 21 Standardized Extracts 22 Pollen 22 Pollen Mixes 22 Epidermals 22 Mites 23 Ancillary Products 24 Normal Saline with Phenol (NSP) 24 Albumin Saline with Phenol (HSA) 24 50% Glycerin 25 Sterile Empty Vials (SEV) 26 Amber Sterile Empty Vials (SEV) 27 Non-Sterile Dropper Vials, Dropper Tips, Pumps 28 Colored Caps for Vials 28 Miscellaneous (labels, information sheets, etc.) 29 Allergy Diagnostics 29 Diagnostic Controls 29 Skin Testing Systems 30 Syringes 30 Mixing Syringes 30 Safety Syringes 30 Standard Syringes 31 Trays 32 Package Inserts 57 Fax Order Form 58 Ordering Information You are encouraged to report patient reactions to skin testing and/or immunotherapy to ALK. Our contact information is toll-free 1-855-216-6497 or email [email protected] ALK is a global allergy solutions company, with a wide range of allergy treatments, products and services that meet the unique needs of allergy sufferers, their families and healthcare professionals. ALK is committed to helping as many people with allergy as possible, which means providing your practice with quality supplies and services to help your business thrive and provide your patients with educational materials to support immunotherapy awareness and improve compliance. From our extensive selection of allergy extracts, skin testing devices, unique products, and patient resources, we are committed to helping you improve the lives of more allergic patients. -

The “Pop Pacific” Japanese-American Sojourners and the Development of Japanese Popular Music
The “Pop Pacific” Japanese-American Sojourners and the Development of Japanese Popular Music By Jayson Makoto Chun The year 2013 proved a record-setting year in Japanese popular music. The male idol group Arashi occupied the spot for the top-selling album for the fourth year in a row, matching the record set by female singer Utada Hikaru. Arashi, managed by Johnny & Associates, a talent management agency specializing in male idol groups, also occupied the top spot for artist total sales while seven of the top twenty-five singles (and twenty of the top fifty) that year also came from Johnny & Associates groups (Oricon 2013b).1 With Japan as the world’s second largest music market at US$3.01 billion in sales in 2013, trailing only the United States (RIAJ 2014), this talent management agency has been one of the most profitable in the world. Across several decades, Johnny Hiromu Kitagawa (born 1931), the brains behind this agency, produced more than 232 chart-topping singles from forty acts and 8,419 concerts (between 2010 and 2012), the most by any individual in history, according to Guinness World Records, which presented two awards to Kitagawa in 2010 (Schwartz 2013), and a third award for the most number-one acts (thirty-five) produced by an individual (Guinness World Record News 2012). Beginning with the debut album of his first group, Johnnys in 1964, Kitagawa has presided over a hit-making factory. One should also look at R&B (Rhythm and Blues) singer Utada Hikaru (born 1983), whose record of four number one albums of the year Arashi matched. -

Creative Cosmetics, 2Nd Edition, English Illustrations: Ashley Greenleaf and Thames & Kosmos LLC
EXPERIMENT MANUAL Please observe the safety information below, the advice for supervising adults on page 1, the safety rules on page 3, and the information about hazardous substances (chemicals) and their environmentally sound disposal, the first aid information, and the other safety information on the inside front cover. WARNING. Not suitable for children under 8 years. For use under adult supervision. Read the instructions before use, follow them and keep them for reference. Keep the kit out of reach of children under 8 years old. Contains glass that may break. Contains some chemicals which present a hazard to health. Do not allow chemicals to come into contact with any part of the body, particularly the mouth and eyes (except as instructed in the manual). Keep small children and animals away from experiments. WARNING — This set contains chemicals that may be harmful if misused. Read cautions on individual containers and in manual carefully. Not to be used by children except under adult supervision. Franckh-Kosmos Verlags-GmbH & Co. KG, Pfizerstr. 5-7, 70184 Stuttgart, Germany | +49 (0) 711 2191-0 | www.kosmos.de Thames & Kosmos, 301 Friendship St., Providence, RI, 02903, USA | 1-800-587-2872 | www.thamesandkosmos.com Thames & Kosmos UK Ltd, Goudhurst, Kent, TN17 2QZ , United Kingdom | 01580 212000 | www.thamesandkosmos.co.uk › › › SAFETY INFORMATION Warning! • Parts in this kit have functional sharp points, corners, or edges. There is a risk of injury. • Always store this experiment kit in a cool place that is inaccessible for small children. Always close containers tightly and keep them away from sources of ignition or open flames (e.g. -

Budget Car Rental Launches New Advertising Campaign Featuring Jessica Simpson
BUDGET CAR RENTAL LAUNCHES NEW ADVERTISING CAMPAIGN FEATURING JESSICA SIMPSON PARSIPPANY, N.J., April 11, 2016 – Budget Car Rental today announced a new series of broadcast commercials, featuring singer, songwriter, actress and fashion designer Jessica Simpson. Breaking today on television and online, Simpson serves as Budget’s brand ambassador in a series of advertisements offering consumers a special limited-time discount offer. The first spot, called “Paparazzi,” — something Simpson is all too familiar with — illustrates how Simpson uses a Budget rental vehicle to dodge pesky photographers while promoting an offer to rent a sporty compact car for $17 on weekend days or $129 for a week-long rental. Another spot, called “You’ve Arrived,” features Simpson talking to her phone and asking it to find her a family getaway. The phone directs her to a Budget SUV. The offer that accompanies the ad is for a sporty SUV for $23 on weekend days or $149 for a week-long rental. “We believe that Budget is the leading value car rental brand in America and is ideal for anyone who wants to get away for the weekend or the week, or for avoiding the paparazzi if you’re an entertainment superstar,” said Scott Deaver, executive vice president and chief marketing officer, Avis Budget Group. “Jessica Simpson embodies the joyful, exuberant entrepreneurial spirit of our customers and is a great fit for the brand. She’s a professional busy mom of two who values the time she spends with her family.” “I like to be spontaneous with my family. We are always up for an adventure!” said Simpson. -

Colin Mortensen from MTV's the Real World Hawaii Comes To
B^JL»^WIN-WAI.H.4LC:E COLLEGE^ September 17, 2003 Volume 90, Issue 3 Colin Mortensen from MTV's The Real World Hawaii Comes to B-W tayOretchenWiuignnmri and immediately capti ended and he had his ankle stnfF writer vated the audience with' checked out by a doctor, he found hjs humor. out that he had competed on an On Wednesday, September 10th lie began his speech by ankle that did not have any liga Colin Mortensen from the t.'v. talking about his back ment across it. •John Rllter and show The Real World: Hawaii ground. Colin lives right • Colin took n break from his lec Johnny Cash pass spoke to students. The event was outside of Los Angeles, ture style and answered questions ...page 6 sponsored by CEP and was held California, and had from the audience. After getting at 9:00 p.m. in the SAC. Students learned about the open asked whether or not he had a girl were given leis at the door in cel casting call for the MTV friend, Colin told the audience that ebration of Colin's MTV show. television show when he he was in a relationship with a Radio station 96.5 FM was blast was attending Berkley woman, thai the relationship had ing over the sound system as an University. While at the been going strong for over a year, estimated ISO audience members easting call, he impressed and that she was very important to anxiously awaited Colin's arrival. him. B-W students also got all of the executive director of Colin Mortensen. -

Media Representations of Simpson and Romo
San Jose State University SJSU ScholarWorks Master's Theses Master's Theses and Graduate Research Fall 2009 "Firing the pigskin real right": Media representations of Simpson and Romo. Lindsey M. Eliopulos San Jose State University Follow this and additional works at: https://scholarworks.sjsu.edu/etd_theses Recommended Citation Eliopulos, Lindsey M., ""Firing the pigskin real right": Media representations of Simpson and Romo." (2009). Master's Theses. 3968. DOI: https://doi.org/10.31979/etd.rhsq-g7hf https://scholarworks.sjsu.edu/etd_theses/3968 This Thesis is brought to you for free and open access by the Master's Theses and Graduate Research at SJSU ScholarWorks. It has been accepted for inclusion in Master's Theses by an authorized administrator of SJSU ScholarWorks. For more information, please contact [email protected]. NOTE TO USERS This reproduction is the best copy available. UMI "FIRING THE PIGSKIN REAL RIGHT": MEDIA REPRESENTATIONS OF SIMPSON AND ROMO A Thesis Presented to The Faculty of the Department of Kinesiology San Jose State University In Partial Fulfillment of the Requirements for the Degree Master of Arts by Lindsey M. Eliopulos December 2009 UMI Number: 1484315 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. UMT Dissertation Publishing UMI 1484315 Copyright 2010 by ProQuest LLC. All rights reserved. This edition of the work is protected against unauthorized copying under Title 17, United States Code. -

Constructing Identity Between the Myths of Black Inferiority and a Post-Racial America
Georgia Southern University Digital Commons@Georgia Southern Electronic Theses and Dissertations Graduate Studies, Jack N. Averitt College of Fall 2012 Through Smoke and Mirrors: Constructing Identity between the Myths of Black Inferiority and a Post-Racial America Gwyneira Yvette Dixon Ledford Follow this and additional works at: https://digitalcommons.georgiasouthern.edu/etd Part of the African American Studies Commons, and the Curriculum and Social Inquiry Commons Recommended Citation Ledford, Gwyneira Yvette Dixon, "Through Smoke and Mirrors: Constructing Identity between the Myths of Black Inferiority and a Post-Racial America" (2012). Electronic Theses and Dissertations. 66. https://digitalcommons.georgiasouthern.edu/etd/66 This dissertation (open access) is brought to you for free and open access by the Graduate Studies, Jack N. Averitt College of at Digital Commons@Georgia Southern. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Digital Commons@Georgia Southern. For more information, please contact [email protected]. THROUGH SMOKE AND MIRRORS: CONSTRUCTING IDENTITY BETWEEN THE MYTHS OF BLACK INFERIORITY AND A POST-RACIAL AMERICA by GWYNEIRA YVETTE DIXON LEDFORD (Under the Direction of Daniel Chapman) ABSTRACT This dissertation is an inquiry into my life. It is an exploration of my lived experience as an African American female negotiating through traditions in Southern culture and societal pressures to create a positive identity. Using autobiographical narrative (Connelly, He, & Phillion, 2008, Pinar, 2008) as a methodology and Black Feminist Thought (Collins, 2000), double consciousness (DuBois, 1903), and the Nigrescence Theory of black identity development (Cross, 1991) as the theoretical framework, I examine my experiences from childhood to adulthood. -

2004 Mtv Video Music Awards”
USHER, KANYE WEST, HOOBASTANK, YELLOWCARD, JET, & JESSICA SIMPSON SET TO PERFORM AT THE “2004 MTV VIDEO MUSIC AWARDS” THE “2004 MTV VIDEO MUSIC AWARDS” TO AIR LIVE FROM MIAMI ON SUNDAY, AUGUST 29th AT 8:00pm ET/PT New York, NY (July 27, 2004) – MTV: Music Television today announced that mega-chart toppers Usher, Kanye West, and Jessica Simpson will all perform at the “2004 MTV Video Music Awards.” Hoobastank, Yellowcard, & Jet will also team up for a super-sized rock performance. This is the first in a rapidly growing list of performers and celebrity guests to be announced for the star-studded event. Each is also nominated for a 2004 VMA. For the first time in the show’s 20-year history, the “2004 MTV Video Music Awards” will air live from Miami, FL on Sunday, August 29th at 8pm ET/PT. “We’ve brought in the heavy hitters,” said Van Toffler, President, MTV & MTV2. “These artists put on incredible live shows, which combined with the heat of Miami, some surprise collaborations, and a stage like no other seen on television will make for an unforgettable night.” The diverse line-up of performers appearing at this year’s show has each achieved recognizable success among music fans and the MTV audience. Usher’s fourth and most recent album CONFESSIONS debuted at #1 on the Billboard 200 and Top R&B/Hip-Hop Album charts, setting an astonishing seven Soundscan sales records and selling 1.1 million albums the first week. Usher has also had considerable success on MTV with his video “Burn,” which is nominated for Best R&B Video, and his video “Yeah” featuring Lil’ Jon and Ludacris which is nominated for four awards including nods for Video of the Year, Best Male Video, Best Dance Video and Best Choreography.