Atopic Dermatitis: a Practice Parameter Update 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Draft Recommendations for Use of Smallpox Vaccine in a Pre-Event
Draft Recommendations for Use of Smallpox Vaccine in a Pre-Event Smallpox Vaccination Program: Supplemental Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Healthcare Infection Control Practices Advisory Committee (HICPAC) In June 2001, the Advisory Committee on Immunization Practices (ACIP) made recommendations for the use of smallpox (vaccinia) vaccine to protect persons working with orthopoxviruses, and to prepare for a possible bioterrorism attack and for response to an attack involving smallpox.[1] Because of the terrorist attacks in the fall of 2001, the Centers for Disease Control and Prevention (CDC) asked the ACIP to review their previous recommendations for smallpox vaccination. These supplemental recommendations update the 2001 recommendations for vaccination of persons designated to respond or care for a suspected or confirmed case of smallpox. In addition, they clarify and expand the primary strategy for control and containment of smallpox in the event of an outbreak. Recommendations for vaccination of laboratory workers who directly handle recombinant vaccinia viruses derived from non-highly attenuated vaccinia strains, or other orthopoxviruses that infect humans (e.g., monkeypox, cowpox, vaccinia, and variola) remain unchanged.[1] The following recommendations were developed after formation of a joint Working Group of the ACIP and the National Vaccine Advisory Committee (NVAC) in April 2002, joined in September 2002 by the Healthcare Infection Control Practices Advisory Committee (HICPAC), and a series of public meetings and forums to review available data on smallpox, smallpox vaccine, smallpox control strategies, and other issues related to smallpox vaccination. Smallpox Transmission and Control Smallpox is transmitted from an infected person. Patients are most infectious during the first 7 to 10 days following rash onset; transmission can occur during the prodromal period just prior to rash onset, when lesions in the mouth ulcerate, releasing virus into oral secretions. -

Painful Bubbles
Osteopathic Family Physician (2018) 29 - 31 29 CLINICAL IMAGES Painful Bubbles Craig Bober, DO & Amy Schultz, DO Lankenau Hospital Family Medicine Residency A 25 year-old female with a past medical history of well controlled eczema presented to her primary care physician with a one week his- tory of a painful “bubbles” localized to her right antecubital fossa as seen in Figure 1. She noted that the new rash appeared to form over- night, was extremely painful, and would occasionally drain a clear liquid after scratching. It did not respond to her usual over-the-counter regimen of moisturizers prompting her to be evaluated. She had subjective fevers and malaise but denied oral or genital ulcers, vaginal discharge, dysuria, ocular irritation, visual disturbances, and upper respiratory or gastrointestinal symptoms. Review of systems was oth- erwise unremarkable. She had no other known medical problems, allergies, and denied drug and alcohol use. She denied any recent travel, sick contacts, pets, or OTC medications/creams. She was sexually active in a monogamous relationship for over a year. QUESTIONS 1. What is the most likely diagnosis? A. Cellulitis B. Eczema herpeticum C. Impetigo D. Primary varicella infection 2. Which test should be performed initally? A. Blood culture B. Direct fuorescent antibody staining FIGURE 1: C. Tzanck smear D. Wound culture 3. What is the best treatment? A. Acyclovir B. Augmentin C. Doxycycline D. Varicella Zoster Immune Globulin CORRESPONDENCE: Amy Schultz, DO | [email protected] 1877-5773X/$ - see front matter. © 2018 ACOFP. All rights reserved. 30 Osteopathic Family Physician | Volume 10, No. 3 | May/June, 2018 ANSWERS 1. -

Eczema Vaccinatum in Indiana’S Public Health Nurses Play a Vital Role in Protecting, Aiding, Child Resulting from and Educating Hoosiers
Volume 10, Issue 6 June 2007 Public Health Nurse Conference Article Page 2007 No. Public Health Nurse Tom Duszynski, BS Conference 2007 1 Eczema Vaccinatum in Indiana’s public health nurses play a vital role in protecting, aiding, Child Resulting from and educating Hoosiers. The Indiana State Department of Health Transmission of (ISDH) recognizes the contribution these nurses make to public health Vaccinia from in Indiana and assists their efforts by offering continuing education Smallpox Vaccinee opportunities, such as the annual Public Health Nurse Conference. with Tertiary Spread to the Mother 3 On June 8, more than 150 public A Decade of Indiana health nurses and Sentinel Influenza Data nursing students Surveillance 8 attended the 2007 ISDH Public Training Room 13 Health Nurse Conference. This Data Reports 14 year’s conference was the most well HIV Summary 14 attended in conference history. Disease Reports 15 Several years ago, the conference began as a “training day” to provide newly hired public health nurses with general education about public health responsibilities within local health departments. The conference has consistently grown over the past several years, and new ideas and different topics have emerged based on suggestions from those who have attended. Conference planners have used participants’ input to restructure the program to meet the needs of public health nurses. This year’s conference was no exception. Deputy State Health Commissioner Mary Hill, an attorney and registered nurse, opened the conference by reminding public health nurses and nursing students of the important work they do every day for Hoosiers and how, since September 11, 2001, their roles and knowledge have changed and expanded to include the world of preparedness, again demonstrating the flexibility of public health nursing. -
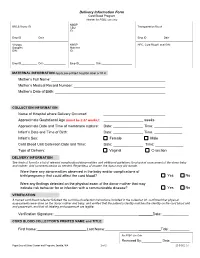
Delivery Information Form Cord Blood Program Header for PSBC Use Only NMDP BBCS Donor ID______CBU Transportation Box #______ID
Delivery Information Form Cord Blood Program Header for PSBC use only NMDP BBCS Donor ID________________________ CBU Transportation Box #____________________ ID: Emp ID___________ Date_______________ Emp ID___________ Date_______________ Virology NMDP HPC, Cord Blood Local DIN: Samples Maternal DIN: ID: Emp ID___________ Date_______________ Emp ID___________ Date_____________________ MATERNAL INFORMATION Apply pre-printed hospital label or fill in Mother’s Full Name: Mother’s Medical Record Number: Mother’s Date of Birth: COLLECTION INFORMATION Name of Hospital where Delivery Occurred: Approximate Gestational Age (must be ≥ 37 weeks): _ weeks Approximate Date and Time of membrane rupture: Date: _______________ Time: ______________ Infant’s Date and Time of Birth: Date: _______________ Time: ______________ Infant’s Sex: Female Male Cord Blood Unit Collection Date and Time: Date: _______________ Time: ______________ Type of Delivery: Vaginal C-section DELIVERY INFORMATION See back of form for a list of relevant complications/abnormalities and additional guidelines for physical assessment of the donor baby and mother. Add comments below as needed. Regardless of answer, the donor may still donate. Were there any abnormalities observed in the baby and/or complications of birth/pregnancy that could affect the cord blood? Yes No Were any findings detected on the physical exam of the donor mother that may indicate risk behavior for or infection with a communicable disease? Yes No VERIFICATION A trained cord blood collector followed the cord blood collection instructions included in the collection kit, confirmed that physical assessments were done on the donor mother and baby, and verified that the patient’s identity matches the identity on the cord blood unit and paperwork, and that all labeling and paperwork are legible. -

BODY LOTIONS/CREAMS and HOMOEOPATHY © Dr
BODY LOTIONS/CREAMS AND HOMOEOPATHY © Dr. Rajneesh Kumar Sharma M.D. (Homoeopathy) Homoeo Cure & Research Centre P. Ltd. NH 74, Moradabad Road, Kashipur (Uttaranchal) INDIA, Pin- 244713 Ph. 05947- 260327, 9897618594 [email protected], [email protected] Definition There are two types of body lotions and creams- 1- Moisturizers, lubricants or softening ones. 2- Cleansing ones. 1- Body lotions and creams are the cosmetic emollient substances, which when applied to skin, protect it from loss of moisture, lubricating and softening dead keratin, thereby lowering the rate at which water evaporates from the skin surface, acting similarly to the natural sebum, secreted by sebaceous glands of the skin. 2- Cleansing creams and lotions are detergent-based or emulsified oil systems that are designed primarily for the removal of surface oil, pollutants, or cellular debris along with makeup. History Perfumed oils About 3100–2907 BC, during the First empire of Egypt, men and women used perfumed oils, stored in unguent jars made of alabaster and marble, to maintain soft, supple, and unwrinkled skin. Face pack By the middle of the first century AD, Romans used a face pack of barley-bean flour, egg, and mashed narcissus bulbs to promote smooth skin. Cold cream A Greek physician of the second century AD invented cold cream containing water, beeswax, and olive oil. When rubbed on the face, the water evaporated, cooling the skin. (Cold cream formulations of the 1920s were of similar composition.) Oiled packs By 1700, smooth skin was in fashion and women applied oiled cloths on their foreheads and wore gloves in bed to prevent wrinkles. -
EL 04-85-GC1 a Study to Define a Set of Requirements for Cleansing Agents for Use in the Space Station Whole Body Shower
FINAL REPORT NAS 9-17428 - EL 04-85-GC1 A Study To Define A Set of Requirements For Cleansing Agents For Use in the Space Station Whole Body Shower. October 29, 1985 _ , MT.X \t> )> C ^ ^>'- N86-16903 S final Unclas 05 ml HC A05/WF A01 ECONOMICS LABORATORY. INC. Osborn Building St. Paul, Minnesota 55102 INDEX CONTENTS PAGE Introduction Final Report 1-26 Table #1 - Foam Test Results Table #2 - Shampoo Ingredient Comparisons Appendix A - Database References Appendix B - Dermal Sensitization Study Appendix C - Eye Irritation Study Appendix D - Protocol For Comparing Shampoos Appendix E - Detergent Filming Build Up Study Figure 1 - Whole Body Portable Shower Head Unit Page 2 October 25, 1985 NAS 9-17428 - EL 04-85-GC1 INTRODUCTION The purpose of this contract is to assist NASA engineers in defining a set of requirements for a whole body cleansing agent to be used in the Space Station Whole Body Shower System. In addition, cleansing agent candidates are to be identified that are likely to satisfy requirements defined in the first part of the study. It is understood that the main reason for having a Whole Body Shower is to satisfy the physiological, psychological and social needs of the crew throughout the duration of duty in ^ the Space Station. The cleansing agent must also be compatible with the vortex water/gas separator and the water reclamation system. To accomplish these goals the study was divided into six tasks. These tasks are as follows: 1. Task One: Survey literature and unpublished information to ascertain state-of-the-art in Whole Body Shower cleansing and the potential impacts of extended use of WBS cleansing agents in a mic'rogravity environment. -

Dermatological Conditions
18 Dermatological Conditions JAMES E. LESSENGER Key words: predisposing factors, patch testing, wood’s light, urticarian, dermatitis Skin problems in worldwide agricultural workers are very common. Among California grape and tomato harvesters, pustular eruptions such as acne and fol- liculitis were present in 30% of studied workers. Irritant or allergic contact der- matitis was present in 2%. In Iowa, 9.6% of male farmers and 14.4% of wives of farmers reported dermatitis during the previous 12-month period. In Washington State, researchers studied 7445 claims for occupational skin disorders filed over a 5-year period. Medical bills totaled $1.22 million, and lost time payments were $1.23 million. The highest rates of occupational skin disorder claims were seen in agriculture with 2.8 claims per 10,000 full-time equivalent employee years. Most of these skin disorders were due to chemical and vegetation exposures (1–4). Among northern Ecuadorian potato farm workers, high rates of dermatitis and pigmentation disorders were attributable to the use of pesticides and fungi- cides. Among California farm workers, skin disease rates were found in tomato workers (6.2%), citrus (10.8%), and vineyard workers (21.0%). Factors found to contribute to dermatitis in farm workers included the specific type of crop cul- tivated, specific job activity, use of personal protective measures, field and home sanitation, environmental conditions of heat and humidity, personal hygiene, allergic history (including atopy), and ethnicity. Several pesticides were shown to cause irritant and allergic contact dermatitis. Causes were found to include pes- ticides, naturally occurring plant substances, heat, sunlight and humidity, atopy, and infectious fungal and bacterial agents (5,6). -

15 Occupational Irritant Dermatitis – Metal Workers
137 15 Occupational Irritant Dermatitis – Metal Workers Undine Berndt, Peter Elsner Contents tates the skin by denaturating keratin, defatting and dehydrating the stratum corneum [6, 7]. In addition, References . 138 frequent wetting and drying cycles contribute to the skin-damaging effect. An above-average incidence of irritant contact dermatitis in those machinists who work at machines with short running periods and do Although computerized tooling operations are in- mechanical work in between has been observed [8]. creasing, the metalworking industry is a trade that Within the phase of manual work, the cutting fluid continues to have a great deal of work done by hand. that the workers are exposed to during machine oper- Consequently, the parts of the body which are pre- ating dries on the skin surface, thus reaching a higher, dominantly affected by occupational skin disease are and thus, irritant concentration. the hands and forearms. Among the frequently ob- served cases of hand dermatitis in metalworkers, the vast majority is of irritant origin [1, 2] (Fig. 1). This condition is closely related to exposure to metalwork- ing fluids. These liquids are sprayed or flow over the Number of case work piece that is being shaped by different mechani- cal means, such as turning, drilling, grinding, or plan- ing. Thus, cutting fluids carry away the produced heat and decrease its production by lubricating the area Observation period (years) between the tool and the metal so as to minimize fric- Fig. 1. Cumulative incidence of irritant hand dermatitis dur- tion. Secondly, they wash away metal chips, reduce ing the observation of 201 trainee metal workers over a period strain hardening, and protect the workpiece against of 2.5 years [9] rusting [3,4]. -

Skin Notation (SK) Profile Pentachlorophenol (PCP) [CAS No
Skin Notation (SK) Profile Pentachlorophenol (PCP) [CAS No. 87-86-5] Department of Health and Human Services Centers for Disease Control and Prevention National Institute for Occupational Safety and Health Disclaimer Mention of any company or product does not constitute endorsement by the National Institute for Occupational Safety and Health (NIOSH). In addition, citations to Web sites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these Web sites. Ordering Information To receive this document or information about other occupational safety and health topics, contact NIOSH: Telephone: 1-800-CDC-INFO (1-800-232-4636) TTY: 1-888-232-6348 E-mail: [email protected] Or visit the NIOSH Web site: www.cdc.gov/niosh For a monthly update on news at NIOSH, subscribe to NIOSH eNews by visiting www.cdc.gov/niosh/eNews. Suggested Citation NIOSH [20XX]. NIOSH skin notation profile: Pentachlorophenol (PCP). By Hudson NL, Dotson GS. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. XXX DHHS (NIOSH) Publication No. XXX ii This information is distributed solely for the purpose of pre-dissemination peer review under applicable information quality guidelines. It has not been formally disseminated by the National Institute for Occupational Safety and Health. It does not represent and should not be construed to represent any agency determination or policy. Foreword As the largest organ of the body, the skin performs multiple critical functions, such as serving as the primary barrier to the external environment. -

Disseminated Varicella Zoster Virus Infection After Vaccination with a Live Attenuated Vaccine
PRACTICE | CASES SEPSIS CPD Disseminated varicella zoster virus infection after vaccination with a live attenuated vaccine Vinita Dubey MD, Derek MacFadden MD n Cite as: CMAJ 2019 September 16;191:E1025-7. doi: 10.1503/cmaj.190270 70-year-old man presented to the emergency depart- ment with a 2-week history of rash, which started as a KEY POINTS localized eruption on his forehead and progressed to a • Live attenuated vaccines are capable of causing symptomatic vesicularA rash involving his entire body (Figure 1). Over this same vaccine-derived infection, even weeks following vaccination. period, he noted increasing shortness of breath, tiredness, pain- • Immunocompromised hosts, including those taking low-dose ful swallowing and chills. He did not report recent travel. immunosuppressive medications, are at increased risk for The patient had a past history of hypertension, coronary artery infection with live vaccine strains. disease, congestive heart failure, chronic obstructive pulmonary • Caution is required before using live attenuated vaccines in immunocompromised people; expert consultation may be disease and atrial flutter. Successful cardiac ablation had been required. performed 2 weeks before the onset of the rash. He also had rheu- • Severe and unusual adverse events following vaccination matoid arthritis, treated with methotrexate, 2.5 mg/d (6 d per should be reported to local public health authorities for week) for 3 years, hydroxychloroquine, 200 mg/d and prednisone, surveillance and investigative purposes. 10 mg/d. In the previous month, his prednisone dosage had been tapered from 10 mg/d. He was not receiving any biologic agents. On examination, the patient’s blood pressure was 110/60 mm Hg, multiple vesicular and crusted lesions, disseminated varicella heart rate 86 beats/min and temperature 36.8°C. -

Skin Conditions That Mean You Should Not Get Smallpox Vaccine
SMALLPOX VACCINE INFORMATION STATEMENT (VIS) SUPPLEMENT C Skin Conditions That Mean You Should Not Get Smallpox Vaccine The smallpox vaccine is made from a live virus related to smallpox called vaccinia (not smallpox virus). The vaccine stimulates the immune system to react against the vaccinia virus, and develop immunity to it. Immunity to vaccinia also provides immunity to smallpox. For most people, live virus vaccines are safe and effective. However, people with certain skin conditions are more likely to have rare and serious reactions to the smallpox vaccine, including bad skin rashes (eczema vaccinatum).This results when virus from the vaccine site gets into broken skin and causes a rash in that area. While most people recover from this rash with treatment, it can be quite severe, sometimes leading to scarring or even death. SKIN CONDITIONS THAT MEAN YOU SHOULD NOT BE VACCINATED: • Individuals who have ever been diagnosed with eczema or atopic dermatitis, (conditions involving repeated episodes of red, itchy or inflamed skin) even if the condition is mild, not presently active, or if you had it only as a child, should not get the vaccine. • Individuals with Darier’s disease should not get the vaccine. • Individuals in close contact with someone who has ever been diagnosed with eczema or atopic dermatitis, even if the condition is mild, not presently active, or if they had it only as a child, should not get the vaccine because of the risk it poses to that close contact. (Close contacts include anyone living in your household and anyone you have close physical contact with such as a sexual partner.) SKIN CONDITIONS THAT MEAN YOU SHOULD WAIT BEFORE BEING VACCINATED: • Individuals with breaks in their skin should not be vaccinated until the skin is fully healed. -

Journal of the Society of Cosmetic Chemists 1976 Volume.27 No.3
Voi. 27 No. 3 March 1976 Journal of the Society of Cosmetic Chemists■ C o n te n ts Page REVIEW PAPER The nature of dandruff Albert M. Kligman, Kenneth J. McGinley, and James J. Leyden ................................................................................ Ill ORIGINAL PAPER Neue insektenabwehrmittel-am Stickstoff disubstituierte /3-alaninderivate (New insect repellent derivatives of N-diubstituted /3-alanine) Manfred Klier and Friedrich Kuhlow ........ ..................................... 141 DEPARTMENTS Synposes fo r c a rd in d e x e s ......................................................................................... XIX In d e x to a d v e rtis e r s ...................................................................................................... XXI Ü* jb. ' ' ' M JJ** La Gronda Sphinx, Asia Minor, 4th Century B.C What sets man apart from all other forms of life is creativity. And it is creativity that sets Givaudan apart. QVAUDAN ïttdeSÉeiïceiif* « < # creativity Givaudan Corporation, 100 Delawanna Avenue,Clifton, N.J.07014. In Canada Givaudan Limited. 60 Overlea Boulevard. Toronto. Ontario Also Argentina • Australia • Brazil • Columbia • England • France • West Germany • Hong Kong • Italy • Japan • Mexico • Republic of South For cold wave lotions and depilatories use Evans Thioglycol made from uniform and high quality vacuum di THIOGLYCOLIC ACID. EVANS THIOGLYCOLATES can help you three important advantages for your cold perman wave and depilatory formulations: (1) uniformity, (2) purity, (3) high quality. Get additional information from EVANS technical service specialists in the field of hair chemistry. EVANS SPECIALIZES IN COMPOUNDS FOR COLD WAVE LOTIONS (PERMS) Emulsifier K-700— a lanolin clouding agent with four ounces of water will produce a for PERMS containing wetting agents and viscous on-the-rod neutralizer. conditioning oils. 4. High Speed Neutralizer containing sodium PERM Neutralizers perborate monohydrate as the active in gredient is available either in foil enve 1.