Vaccinations in Pregnancy DENISE K
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

For Schools and Parents: K-12 Immunization Requirements
FOR SCHOOLS AND PARENTS: K-12 IMMUNIZATION REQUIREMENTS NJ Department of Health (NJDOH) Vaccine Preventable Disease Program Summary of NJ School Immunization Requirements Listed in the chart below are the minimum required number of doses your child must have to attend a NJ school.* This is strictly a summary document. Exceptions to these requirements (i.e. provisional admission, grace periods, and exemptions) are specified in the Immunization of Pupils in School rules, New Jersey Administrative Code (N.J.A.C. 8:57-4). Please reference the administrative rules for more details https://www.nj.gov/health/cd/imm_requirements/acode/. Additional vaccines are recommended by Advisory Committee on Immunization Practices (ACIP) for optimal protection. For the complete ACIP Recommended Immunization Schedule, please visit http://www.cdc.gov/vaccines/schedules/index.html. Minimum Number of Doses for Each Vaccine Grade/level child DTaP Polio MMR Varicella Hepatitis Meningococcal Tdap enters school: Diphtheria, Tetanus, acellular Pertussis Inactivated (Measles, (Chickenpox) B (Tetanus, Polio Vaccine Mumps, diphtheria, (IPV) Rubella) acellular pertussis) § | Kindergarten – A total of 4 doses with one of these doses A total of 3 2 doses 1 dose 3 doses None None 1st grade on or after the 4th birthday doses with one OR any 5 doses† of these doses given on or after the 4th birthday ‡ OR any 4 doses nd th † 2 – 5 grade 3 doses 3 doses 2 doses 1 dose 3 doses None See footnote NOTE: Children 7 years of age and older, who have not been previously vaccinated with the primary DTaP series, should receive 3 doses of Td. -

Polio Vaccine May Be Given at the Same Time As Other Paralysis (Can’T Move Arm Or Leg)
POLIO VVPOLIO AAACCINECCINECCINE (_________ W H A T Y O U N E E D T O K N O W ) (_I111 ________What is polio? ) (_I ________Who should get polio ) 333 vaccine and when? Polio is a disease caused by a virus. It enters a child’s (or adult’s) body through the mouth. Sometimes it does IPV is a shot, given in the leg or arm, depending on age. not cause serious illness. But sometimes it causes Polio vaccine may be given at the same time as other paralysis (can’t move arm or leg). It can kill people who vaccines. get it, usually by paralyzing the muscles that help them Children breathe. Most people should get polio vaccine when they are Polio used to be very common in the United States. It children. Children get 4 doses of IPV, at these ages: paralyzed and killed thousands of people a year before we 333 A dose at 2 months 333 A dose at 6-18 months had a vaccine for it. 333 A dose at 4 months 333 A booster dose at 4-6 years 222 Why get vaccinated? ) Adults c I Most adults do not need polio vaccine because they were Inactivated Polio Vaccine (IPV) can prevent polio. already vaccinated as children. But three groups of adults are at higher risk and should consider polio vaccination: History: A 1916 polio epidemic in the United States killed (1) people traveling to areas of the world where polio is 6,000 people and paralyzed 27,000 more. In the early common, 1950’s there were more than 20,000 cases of polio each (2) laboratory workers who might handle polio virus, and year. -

Swine Flu and Polio Vaccines: Some Parallels and Some Differences
Swine Fluand Polio Vaccines: Some Parallelsand Some Differences Howard B. Baumel College of Staten Island of the City Universityof New York Staten Island 10301 The swine flu vaccinationprogram vaccine could be successfullydevel- facturedby a single pharmaceutical generated debate in scientific and oped. company.The cause of this outbreak medical circlesthat extended to the Salkrelied heavily on his previous was never clearly established. Be- Downloaded from http://online.ucpress.edu/abt/article-pdf/39/9/550/36038/4446085.pdf by guest on 29 September 2021 general public.The controversythat experience as he attemptedto pro- cause bottles of tissue culture fluid centered on the vaccine's effective- duce a killedvirus polio vaccine.He containingthe virushad been stored ness and safety was reminiscentof used formalinto kill the virus and priorto being treated with formalin, the problemsthat accompaniedthe isolated one strain for each of the it was possiblethat bits of tissue had development of the polio vaccine three knowntypes of polio virus.To settled to the bottom covering the years ago. A review of that earlier determineif any live virusremained viruses and protecting them from scientific achievement can provide after the exposure to formalin,the the formalin.To prevent this, the insightsinto the swineflu dilemma. treated virus was injected into the tissue culture fluid was filtered to By the mid-1930's,only threeviral brain of a monkey. If the monkey remove the debris before exposure diseases,smallpox, rabies, and yellow contracted polio, it was concluded to formalin. fever, had yielded to vaccines. In that live viruswas present.To deter- HeraldCox and HilaryKoprowski each of these cases, the vaccine mine if the treated virus was effec- (1955, 1956) had developed an consisted of a live virus. -

Polio Fact Sheet
Polio Fact Sheet 1. What is Polio? - Polio is a disease caused by a virus that lives in the human throat and intestinal tract. It is spread by exposure to infected human stool: e.g. from poor sanitation practices. The 1952 Polio epidemic was the worst outbreak in the nation's history. Of nearly 58,000 cases reported that year, 3,145 people died and 21,269 were left with mild to disabling paralysis, with most of the victims being children. The "public reaction was to a plague", said historian William O'Neill. "Citizens of urban areas were to be terrified every summer when this frightful visitor returned.” A Polio vaccine first became available in 1955. 2. What are the symptoms of Polio? - Up to 95 % of people infected with Polio virus are not aware they are infected, but can still transmit it to others. While some develop just a fever, sore throat, upset stomach, and/or flu-like symptoms and have no paralysis or other serious symptoms, others get a stiffness of the back or legs, and experience increased sensitivity. However, a few develop life-threatening paralysis of muscles. The risk of developing serious symptoms increases with the age of the ill person. 3. Is Polio still a disease seen in the United States? - The last naturally occurring cases of Polio in the United States were in 1979, when an outbreak occurred among the Amish in several states including Pennsylvania. 4. What kinds of Polio vaccines are used in the United States? - There is now only one kind of Polio vaccine used in the United States: the Inactivated Polio vaccine (IPV) is given as an injection (shot). -

Draft Recommendations for Use of Smallpox Vaccine in a Pre-Event
Draft Recommendations for Use of Smallpox Vaccine in a Pre-Event Smallpox Vaccination Program: Supplemental Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Healthcare Infection Control Practices Advisory Committee (HICPAC) In June 2001, the Advisory Committee on Immunization Practices (ACIP) made recommendations for the use of smallpox (vaccinia) vaccine to protect persons working with orthopoxviruses, and to prepare for a possible bioterrorism attack and for response to an attack involving smallpox.[1] Because of the terrorist attacks in the fall of 2001, the Centers for Disease Control and Prevention (CDC) asked the ACIP to review their previous recommendations for smallpox vaccination. These supplemental recommendations update the 2001 recommendations for vaccination of persons designated to respond or care for a suspected or confirmed case of smallpox. In addition, they clarify and expand the primary strategy for control and containment of smallpox in the event of an outbreak. Recommendations for vaccination of laboratory workers who directly handle recombinant vaccinia viruses derived from non-highly attenuated vaccinia strains, or other orthopoxviruses that infect humans (e.g., monkeypox, cowpox, vaccinia, and variola) remain unchanged.[1] The following recommendations were developed after formation of a joint Working Group of the ACIP and the National Vaccine Advisory Committee (NVAC) in April 2002, joined in September 2002 by the Healthcare Infection Control Practices Advisory Committee (HICPAC), and a series of public meetings and forums to review available data on smallpox, smallpox vaccine, smallpox control strategies, and other issues related to smallpox vaccination. Smallpox Transmission and Control Smallpox is transmitted from an infected person. Patients are most infectious during the first 7 to 10 days following rash onset; transmission can occur during the prodromal period just prior to rash onset, when lesions in the mouth ulcerate, releasing virus into oral secretions. -

Painful Bubbles
Osteopathic Family Physician (2018) 29 - 31 29 CLINICAL IMAGES Painful Bubbles Craig Bober, DO & Amy Schultz, DO Lankenau Hospital Family Medicine Residency A 25 year-old female with a past medical history of well controlled eczema presented to her primary care physician with a one week his- tory of a painful “bubbles” localized to her right antecubital fossa as seen in Figure 1. She noted that the new rash appeared to form over- night, was extremely painful, and would occasionally drain a clear liquid after scratching. It did not respond to her usual over-the-counter regimen of moisturizers prompting her to be evaluated. She had subjective fevers and malaise but denied oral or genital ulcers, vaginal discharge, dysuria, ocular irritation, visual disturbances, and upper respiratory or gastrointestinal symptoms. Review of systems was oth- erwise unremarkable. She had no other known medical problems, allergies, and denied drug and alcohol use. She denied any recent travel, sick contacts, pets, or OTC medications/creams. She was sexually active in a monogamous relationship for over a year. QUESTIONS 1. What is the most likely diagnosis? A. Cellulitis B. Eczema herpeticum C. Impetigo D. Primary varicella infection 2. Which test should be performed initally? A. Blood culture B. Direct fuorescent antibody staining FIGURE 1: C. Tzanck smear D. Wound culture 3. What is the best treatment? A. Acyclovir B. Augmentin C. Doxycycline D. Varicella Zoster Immune Globulin CORRESPONDENCE: Amy Schultz, DO | [email protected] 1877-5773X/$ - see front matter. © 2018 ACOFP. All rights reserved. 30 Osteopathic Family Physician | Volume 10, No. 3 | May/June, 2018 ANSWERS 1. -

2021-22 School Year New York State Immunization Requirements for School Entrance/Attendance1
2021-22 School Year New York State Immunization Requirements for School Entrance/Attendance1 NOTES: Children in a prekindergarten setting should be age-appropriately immunized. The number of doses depends on the schedule recommended by the Advisory Committee on Immunization Practices (ACIP). Intervals between doses of vaccine should be in accordance with the ACIP-recommended immunization schedule for persons 0 through 18 years of age. Doses received before the minimum age or intervals are not valid and do not count toward the number of doses listed below. See footnotes for specific information foreach vaccine. Children who are enrolling in grade-less classes should meet the immunization requirements of the grades for which they are age equivalent. Dose requirements MUST be read with the footnotes of this schedule Prekindergarten Kindergarten and Grades Grades Grade Vaccines (Day Care, 1, 2, 3, 4 and 5 6, 7, 8, 9, 10 12 Head Start, and 11 Nursery or Pre-k) Diphtheria and Tetanus 5 doses toxoid-containing vaccine or 4 doses and Pertussis vaccine 4 doses if the 4th dose was received 3 doses (DTaP/DTP/Tdap/Td)2 at 4 years or older or 3 doses if 7 years or older and the series was started at 1 year or older Tetanus and Diphtheria toxoid-containing vaccine Not applicable 1 dose and Pertussis vaccine adolescent booster (Tdap)3 Polio vaccine (IPV/OPV)4 4 doses 3 doses or 3 doses if the 3rd dose was received at 4 years or older Measles, Mumps and 1 dose 2 doses Rubella vaccine (MMR)5 Hepatitis B vaccine6 3 doses 3 doses or 2 doses of adult hepatitis B vaccine (Recombivax) for children who received the doses at least 4 months apart between the ages of 11 through 15 years Varicella (Chickenpox) 1 dose 2 doses vaccine7 Meningococcal conjugate Grades 2 doses vaccine (MenACWY)8 7, 8, 9, 10 or 1 dose Not applicable and 11: if the dose 1 dose was received at 16 years or older Haemophilus influenzae type b conjugate vaccine 1 to 4 doses Not applicable (Hib)9 Pneumococcal Conjugate 1 to 4 doses Not applicable vaccine (PCV)10 Department of Health 1. -

Eczema Vaccinatum in Indiana’S Public Health Nurses Play a Vital Role in Protecting, Aiding, Child Resulting from and Educating Hoosiers
Volume 10, Issue 6 June 2007 Public Health Nurse Conference Article Page 2007 No. Public Health Nurse Tom Duszynski, BS Conference 2007 1 Eczema Vaccinatum in Indiana’s public health nurses play a vital role in protecting, aiding, Child Resulting from and educating Hoosiers. The Indiana State Department of Health Transmission of (ISDH) recognizes the contribution these nurses make to public health Vaccinia from in Indiana and assists their efforts by offering continuing education Smallpox Vaccinee opportunities, such as the annual Public Health Nurse Conference. with Tertiary Spread to the Mother 3 On June 8, more than 150 public A Decade of Indiana health nurses and Sentinel Influenza Data nursing students Surveillance 8 attended the 2007 ISDH Public Training Room 13 Health Nurse Conference. This Data Reports 14 year’s conference was the most well HIV Summary 14 attended in conference history. Disease Reports 15 Several years ago, the conference began as a “training day” to provide newly hired public health nurses with general education about public health responsibilities within local health departments. The conference has consistently grown over the past several years, and new ideas and different topics have emerged based on suggestions from those who have attended. Conference planners have used participants’ input to restructure the program to meet the needs of public health nurses. This year’s conference was no exception. Deputy State Health Commissioner Mary Hill, an attorney and registered nurse, opened the conference by reminding public health nurses and nursing students of the important work they do every day for Hoosiers and how, since September 11, 2001, their roles and knowledge have changed and expanded to include the world of preparedness, again demonstrating the flexibility of public health nursing. -

Vaccinations for Preteens and Teens, Age 11-19 Years
Vaccinations for Preteens and Teens, Age 11–19 Years Getting immunized is a lifelong, life-protecting job. Make sure you and your healthcare provider keep your immunizations up to date. Check to be sure you’ve had all the vaccinations you need. Vaccine Do you need it? Chickenpox Yes! If you haven’t been vaccinated and haven’t had chickenpox, you need 2 doses of this vaccine. (varicella; Var) Anybody who was vaccinated with only 1 dose should get a second dose. Hepatitis A Yes! If you haven’t been vaccinated, you need 2 doses of this vaccine. Anybody who was vaccinated (HepA) with only 1 dose should get a second dose at least 6–18 months later. Hepatitis B Yes! This vaccine is recommended for all people age 0–18 years. You need a hepatitis B vaccine series (HepB) if you have not already received it. Haemophilus influ- Maybe. If you haven’t been vaccinated against Hib and have a high-risk condition (such as a non- enzae type b (Hib) functioning spleen), you need this vaccine. Human Yes! All preteens need 2 doses of HPV vaccine at age 11 or 12. Older teens who haven't been vacci- papillomavirus nated will need 2 or 3 doses. This vaccine protects against HPV, a common cause of genital warts and (HPV) several types of cancer, including cervical cancer and cancer of the anus, penis, and throat. Influenza Yes! Everyone age 6 months and older needs annual influenza vaccination every fall or winter and (Flu) for the rest of their lives. -
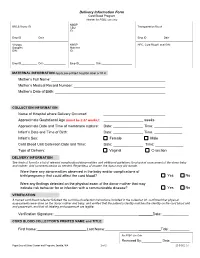
Delivery Information Form Cord Blood Program Header for PSBC Use Only NMDP BBCS Donor ID______CBU Transportation Box #______ID
Delivery Information Form Cord Blood Program Header for PSBC use only NMDP BBCS Donor ID________________________ CBU Transportation Box #____________________ ID: Emp ID___________ Date_______________ Emp ID___________ Date_______________ Virology NMDP HPC, Cord Blood Local DIN: Samples Maternal DIN: ID: Emp ID___________ Date_______________ Emp ID___________ Date_____________________ MATERNAL INFORMATION Apply pre-printed hospital label or fill in Mother’s Full Name: Mother’s Medical Record Number: Mother’s Date of Birth: COLLECTION INFORMATION Name of Hospital where Delivery Occurred: Approximate Gestational Age (must be ≥ 37 weeks): _ weeks Approximate Date and Time of membrane rupture: Date: _______________ Time: ______________ Infant’s Date and Time of Birth: Date: _______________ Time: ______________ Infant’s Sex: Female Male Cord Blood Unit Collection Date and Time: Date: _______________ Time: ______________ Type of Delivery: Vaginal C-section DELIVERY INFORMATION See back of form for a list of relevant complications/abnormalities and additional guidelines for physical assessment of the donor baby and mother. Add comments below as needed. Regardless of answer, the donor may still donate. Were there any abnormalities observed in the baby and/or complications of birth/pregnancy that could affect the cord blood? Yes No Were any findings detected on the physical exam of the donor mother that may indicate risk behavior for or infection with a communicable disease? Yes No VERIFICATION A trained cord blood collector followed the cord blood collection instructions included in the collection kit, confirmed that physical assessments were done on the donor mother and baby, and verified that the patient’s identity matches the identity on the cord blood unit and paperwork, and that all labeling and paperwork are legible. -

U.S. Support Essential to Ambitious Global Introduction of Inactivated Polio Vaccine
December 2014 U.S. Support Essential to Ambitious Global Introduction of Inactivated Polio Vaccine Nellie Bristol1 Earlier this fall, Nepal became the first low-income country to introduce the inactivated polio vaccine (IPV) into its immunization system. Many more countries will have to follow suit to meet the ambitious deadlines laid out in the Global Polio Eradication Initiative’s (GPEI)2 Polio Eradication & Endgame Strategic Plan 2013–2018.3 The plan calls for global introduction of at least one dose of IPV into routine childhood immunization schedules followed by eventual withdrawal of the widely used oral polio vaccine (OPV). Currently, 75 mostly high- and middle-income countries use the injectable IPV in their immunization systems, leaving 119 that need to do so by the end of 2015 to keep with the plan’s schedule. The IPV introduction timeline called for in the strategy is extraordinarily quick; most vaccines are incorporated into national routine immunization programs over years if not decades. In calling for universal adoption of IPV over several years, “We’ll be trying to do something that’s never been done in terms of speed,” said Bruce Aylward, the World Health Organization’s assistant director-general for polio and emergencies.4 The move is necessary to complete and sustain global polio eradication. OPV has long been the vaccine of choice for many countries and is used in mass vaccination campaigns. It is inexpensive (as little as 14 cents per dose),5 easy to administer, and provides comprehensive immunity. But it has one serious drawback: since it uses a live, weakened virus, in rare instances, polioviruses in the vaccine can cause the disease. -

COVID-19 Vaccines: Summary of Current State-Of-Play Prepared Under Urgency 21 May 2020 – Updated 16 July 2020
Office of the Prime Minister’s Chief Science Advisor Kaitohutohu Mātanga Pūtaiao Matua ki te Pirimia COVID-19 vaccines: Summary of current state-of-play Prepared under urgency 21 May 2020 – updated 16 July 2020 The COVID-19 pandemic has spurred a global effort to find a vaccine to protect people from SARS- CoV-2 infection. This summary highlights selected candidates, explains the different types of vaccines being investigated and outlines some of the potential issues and risks that may arise during the clinical testing process and beyond. Key points • There are at least 22 vaccine candidates registered in clinical (human) trials, out of a total of at least 194 in various stages of active development. • It is too early to choose a particular frontrunner as we lack safety and efficacy information for these candidates. • It is difficult to predict when a vaccine will be widely available. The fastest turnaround from exploratory research to vaccine approval was previously 4–5 years (ebolavirus vaccine), although it is likely that current efforts will break this record. • There are a number of challenges associated with accelerated vaccine development, including ensuring safety, proving efficacy in a rapidly changing pandemic landscape, and scaling up manufacture. • The vaccine that is licensed first will not necessarily confer full or long-lasting protection. 1 Contents Key points .................................................................................................................................. 1 1. Types of vaccines ...............................................................................................................