Identification of Drugs Blocking SARS-Cov-2 Infection Using Human
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Unlicensed Medicines List for Suffolk D&T
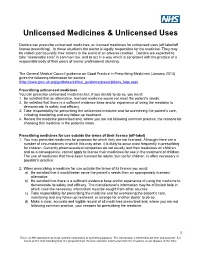
Unlicensed Medicines & Unlicensed Uses Doctors can prescribe unlicensed medicines, or licensed medicines for unlicensed uses (off-label/off license prescribing). In these situations the doctor is legally responsible for the medicine. They may be called upon to justify their actions in the event of an adverse reaction. Doctors are expected to take “reasonable care” in common law, and to act in a way which is consistent with the practice of a responsible body of their peers of similar professional standing. The General Medical Council guidance on Good Practice in Prescribing Medicines (January 2013) gives the following information for doctors (http://www.gmc-uk.org/guidance/ethical_guidance/prescriptions_faqs.asp) Prescribing unlicensed medicines You can prescribe unlicensed medicines but, if you decide to do so, you must: 1. Be satisfied that an alternative, licensed medicine would not meet the patient's needs. 2. Be satisfied that there is a sufficient evidence base and/or experience of using the medicine to demonstrate its safety and efficacy. 3. Take responsibility for prescribing the unlicensed medicine and for overseeing the patient's care, including monitoring and any follow up treatment. 4. Record the medicine prescribed and, where you are not following common practice, the reasons for choosing this medicine in the patient's notes. Prescribing medicines for use outside the terms of their licence (off-label) 1. You may prescribe medicines for purposes for which they are not licensed. Although there are a number of circumstances in which this may arise, it is likely to occur most frequently in prescribing for children. Currently pharmaceutical companies do not usually test their medicines on children and as a consequence, cannot apply to license their medicines for use in the treatment of children. -

Treatment of Relapsing Malaria with Specific Antimalarial Drugs In
Sept., 1947 J TREATMENT OF RELAPSING MALARIA: DESHMUKH 511 up to the expectation. But it soon became Articles clear that they did not control relapse, and Original also that they carry with them a danger of toxicity. Arsenic is notorious for causing to TREATMENT of relapsing malaria damage liver, kidneys and brain. When pregnancy complicates malaria, the use of WITH SPECIFIC ANTIMALARIAL quinine and arsenic may be particularly risky DRUGS IN COMBINATION WITH and one is on the horns of a dilemma as regards PENICILLIN the satisfactory treatment in such circumstances. The writer's experience of arsenicals in By P. L. DESHMUKH, m.d. (Bom.), malaria has been borne out other workers F.C.P.S. by D.T.M.\& II. (Lond.), and their findings in large-scale experiments Poona Sassoon Hospitals, given below will help to dislodge from the minds It must be admitted that even with quinine of the clinicians any lingering faith in arsenic and the synthetic antimalarial drugs like as an ideal antimalarial drug. atabrine, mepacrine, etc. (henceforth called Professor Blacklock (1944) has pointed out specific antimalarials ' for the sake of after long studies at the Liverpool school that tee brevity) treatment of malaria is still very unsatis- though the immediate effects of arsenic in factory. The recognized failure of the specific relapsing malaria were striking, the ultimate antimalarials singly or in combination to control results were disappointing in that practically relapses materially is a matter of great all cases relapsed even after full arsenical concern. A great variation is observed in the treatment. Thus, arsenicals though immediately mterval that may before the occurrence effective against vivax parasites do not eliminate a elapse y relapse. -

Light Sensitive Eruptions Treated with Atabrine and Chloroquine John M
LIGHT SENSITIVE ERUPTIONS TREATED WITH ATABRINE AND CHLOROQUINE JOHN M. KNOX, M.D.,JOHNH. LAMB,Ml)., BEDFORDSHELMIRE, M.D.,AND ROBERT J. MORGAN, M.D. In April 1951 a 50-year-old female, a Red Cross worker recently returned from India, came to one of us (J. M. K.) at Keesler Air Force Base, Biloxi, Mississippi. While in India she had taken atabrine for its antimalarial action. During the period that her skin was yellowed by atabrine pigmentation she had noticed a conspicuous decrease in the severity of a long-standing light-sensitive eruption, prurigo aestivale. The annoying disease was beginning to reappear arid she preferred a return of the yellow discoloration to the eruption. Her response tG atabrine was so noteworthy that later a man 28 years of age with a plaque-like, light-sensitive eruption of the face was given a similar therapeutic trial with the same success. The improvement noted in these two cases, plus the appearance of reports by Page (la) and others (ib, c, d) on atabrine in discoid lupus erythematosus encouraged a clinical evaluation of this drug for the treatment of light-sensitive eruptions. Black (2), in a report of the use of mepacrine in lupus erythematosus, tested four patients with actinic dermatitis with this preparation. No description of the types of dermatitis was recorded. Two female patients were cleared; they had had the disease each summer for 11 and 30 years respectively. The condition of the other two patients (who were males) was unaltered by this drug. DISCUSSION Figure 1 gives a summary of the 18 cases of various types of solar dermatitis. -

有限公司 API Antineoplastic Agents
® 伊域化學藥業(香港)有限公司 YICK-VIC CHEMICALS & PHARMACEUTICALS (HK) LTD Rm 1006, 10/F, Hewlett Centre, Tel: (852) 25412772 (4 lines) No. 52-54, Hoi Yuen Road, Fax: (852) 25423444 / 25420530 / 21912858 Kwun Tong, E-mail: [email protected] YICK -VIC 伊域 Kowloon, Hong Kong. Site: http://www.yickvic.com API Antineoplastic Agents Product Highlight The following is a selection of products we have sourced and supplied to our customers globally. For detailed specifications, certificates of analysis, supply position, and tailored pricing, please contact us at [email protected] . For any unlisted products that you require, feel free to contact us for support. We can source or custom manufacture at your specification. Product Code CAS Product Name PH-3107DA 522-17-8 (-)-DEGUELIN PH-4360CF 989-51-5 (-)-EPIGALLOCATECHIN GALLATE MIS-6071 32981-86-5 10-DEACETYLBACCATIN III (REFERENCE GRADE) MIS-5741 78432-77-6 10-DEACETYLPACLITAXEL (REFERENCE GRADE) PH-0441BA 19685-09-7 10-HYDROXYCAMPTOTHECIN 64439-81-2 (UNSPECIFIED ISOMER) PH-0441BC 19685-09-7 10-HYDROXYCAMPTOTHECIN (REFERENCE GRADE) 64439-81-2 (UNSPECIFIED ISOMER) PH-3394A 533-67-5 2-DEOXY-D-RIBOSE PH-1956DA 951-78-0 2'-DEOXYURIDINE PH-0865F 38390-45-3 3',4'-ANHYDROVINBLASTINE MIS-10676 75567-37-2 3-INGENYL ANGELATE (REFERENCE GRADE) 849146-39-0 Copyright © 2020 YICK-VIC CHEMICALS & PHARMACEUTICALS (HK) LTD. All rights reserved. Page 1 of 57 Product Code CAS Product Name PH-1578EK 2498-50-2 4-AMINOBENZAMIDINE DIHYDROCHLORIDE PH-1541D 23363-35-1 4'-DEMETHYLEPIPODOPHYLLOTOXIN-9 BETA-GLUCOPYRANOSIDE PH-4586B 1716-12-7 -

Mepacrine Hydrochloride/Metronidazole
Mepacrine Hydrochloride/Metronidazole 837 mothorax but the treatment is associated with pain and a high Metronidazole Hydrochloride (BANM, USAN, rINNM) lung cancer, although all 4 were in women who were smokers. frequency of toxic effects. Subsequent follow-up4 to 1984, covering a period of 15 to 25 Hidrocloruro de metronidazol; Métronidazole, Chlorhydrate de; Preparations years, still showed an excess of lung cancer cases even after al- Metronidazoli Hydrochloridum; SC-32642. lowing for smoking status. However, this follow-up also contin- Proprietary Preparations (details are given in Part 3) Метронидазола Гидрохлорид ued to show no significant increase overall in cancer-related India: Maladin. 5 C6H9N3O3,HCl = 207.6. morbidity or mortality. Follow-up of the patients from the sec- CAS — 69198-10-3. ond study for 11 to 15 years to 1984 also showed no increase in ATC — A01AB17; D06BX01; G01AF01; J01XD01; the overall incidence of cancers nor did it confirm any increase Methyl Benzoquate (BAN) P01AB01. in lung cancer. ATC Vet — QA01AB17; QD06BX01; QG01AF01; Risks to the fetus are discussed under Pregnancy in Precautions, Nequinate (USAN, pINN); AY-20385; ICI-55052; Néquinate; Ne- QJ01XD01; QP51AA01. below. quinato; Nequinatum. Methyl 7-benzyloxy-6-butyl-1,4-dihydro- 1. Bendesky A, et al. Is metronidazole carcinogenic? Mutat Res 4-oxoquinoline-3-carboxylate. Incompatibility. Solutions of metronidazole hydrochloride have a low pH, usually of less than 2.0, before dilution and neu- 2002; 511: 133–44. Нехинат 2. Beard CM, et al. Lack of evidence for cancer due to use of met- tralisation for intravenous use. These undiluted solutions react ronidazole. N Engl J Med 1979; 301: 519–22. -

OUH Formulary Approved for Use in Breast Surgery
Oxford University Hospitals NHS Foundation Trust Formulary FORMULARY (Y): the medicine can be used as per its licence. RESTRICTED FORMULARY (R): the medicine can be used as per the agreed restriction. NON-FORMULARY (NF): the medicine is not on the formulary and should not be used unless exceptional approval has been obtained from MMTC. UNLICENSED MEDICINE – RESTRICTED FORMULARY (UNR): the medicine is unlicensed and can be used as per the agreed restriction. SPECIAL MEDICINE – RESTRICTED FORMULARY (SR): the medicine is a “special” (unlicensed) and can be used as per the agreed restriction. EXTEMPORANEOUS PREPARATION – RESTRICTED FORMULARY (EXTR): the extemporaneous preparation (unlicensed) can be prepared and used as per the agreed restriction. UNLICENSED MEDICINE – NON-FORMULARY (UNNF): the medicine is unlicensed and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. SPECIAL MEDICINE – NON-FORMULARY (SNF): the medicine is a “special” (unlicensed) and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. EXTEMPORANEOUS PREPARATION – NON-FORMULARY (EXTNF): the extemporaneous preparation (unlicensed) cannot be prepared and used unless exceptional approval has been obtained from MMTC. CLINICAL TRIALS (C): the medicine is clinical trial material and is not for clinical use. NICE TECHNOLOGY APPRAISAL (NICETA): the medicine has received a positive appraisal from NICE. It will be available on the formulary from the day the Technology Appraisal is published. Prescribers who wish to treat patients who meet NICE criteria, will have access to these medicines from this date. However, these medicines will not be part of routine practice until a NICE TA Implementation Plan has been presented and approved by MMTC (when the drug will be given a Restricted formulary status). -

Sawbones 318: Hydroxychloroquine Published on April 12Th, 2020 Listen on Themcelroy.Family Clint
Sawbones 318: Hydroxychloroquine Published on April 12th, 2020 Listen on TheMcElroy.family Clint: Sawbones is a show about medical history, and nothing the hosts say should be taken as medical advice or opinion. It‘s for fun. Can't you just have fun for an hour and not try to diagnose your mystery boil? We think you've earned it. Just sit back, relax, and enjoy a moment of distraction from that weird growth. You're worth it [theme music plays] Justin: Hello everybody, and welcome to Sawbones, a marital tour of misguided medicine. I'm your co-host, Justin McElroy. Sydnee: And I'm Sydnee McElroy. Justin: Uh, Syd, y'know, it seems really unfair, in this day and age… lots is unfair about this situation we find ourselves in. The unpleasantness, as I have called it repeatedly. Sydnee: Yes. Justin: It isn't catching on, but that‘s okay. I'm patient. I've got nothing to do but wait. Sydnee: That‘s a bit of an understatement, but… Justin: Yeah, it is. Sydnee: Carry on. Justin: It is. That‘s fair. The very unpleasantness? Super unpleasant? I'll work on it. Um… Sydnee: I don't know. A lot of people are calling it the dystopian—the sickness. Justin: The sickness is like, very… Sydnee: It‘s quite dystopian. Yeah. It‘s hard. Justin: Charlie just says ‗the virus,‘ which is like… accurate. Sydnee: Yes. Justin: But lacks some amount of pageantry. Um, no, it seems unfair, because I feel like I have to educate myself about something new every few days. -

A Computational Tool for Pathway-Based Rational Drug Repositioning Supplementary Information
gene2drug: a Computational Tool for Pathway-based Rational Drug Repositioning Supplementary Information Francesco Napolitano1, Diego Carrella1, Barbara Mandriani1, Sandra Pisonero1, Diego Medina1, Nicola Brunetti-Pierri1,2, and Diego di Bernardo1,3 1Telethon Institute of Genetics and Medicine (TIGEM), Pozzuoli (NA), 80078, Italy. 2Department of Translational Medicine, Federico II University, 80131 Naples, Italy 3Department of Chemical, Materials and Industrial Production Engineering, University of Naples Federico II, 80125 Naples, Italy. List of Figures S1 Relation between PPI network-based and pathway based approaches. Given a therapeutic gene and the set of pathways it is annotated to according to the different databases, the other genes in the same pathways are topologically closer to it in the PPI network as compared to randomly chosen genes. The average shortest path from the selected gene to other pathway members is reported on the y axis for each database. 3 S2 Size of intersection between existent evidence scores in the STITCH database (subset matched against the Cmap database) as a percentage of the total number of evidences. Numbers on the diagonal represent how many times a drug-target evidence exists divided by the total number of reported pairs. A \combined score" always exist if one of the other evidences exist, thus \combined score" covers 100% of the pairs. Conversely, an \experimental" score is only present for 14% of the pairs. The \Text mining" evidence strongly drives the \combined score" covering 61% of all the known protein-target interactions in STITCH. 4 S3 Relative luminescence units (RLU) in Hepa1-6 cells transfected with a plasmid ex- pressing the luciferase gene under the control of the GPT promoter and incubated with various concentrations of fulvestrant. -

Malaria Chemotherapy & Drug Resistance
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this material constitutes acceptance of that license and the conditions of use of materials on this site. Copyright 2006, The Johns Hopkins University and David Sullivan. All rights reserved. Use of these materials permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for obtaining permissions for use from third parties as needed. Malaria Chemotherapy and Drug Resistance David Sullivan, MD Eradication Attempts •Hookworm1909-1924: Sanitation and drug treatment; no reduction in 15 yrs. • Yellow Fever 1915-1930s: Mosquito control; discovery of natural reservoir in jungle animals ceased efforts. •Yaws1940-1960: Mass screening and penicillin; continued spread after best efforts. •Malaria1955-1975: DDT & chloroquine; $2 billion spent; insecticide resistance & African failure of DDT ceased efforts. • Smallpox 1967-1977: Successful vaccine heat stable and 99% effective as single dose; no hidden carriers. • Dracunculiasis 1986-?: 3.5 million to 100,000; Sudan - 605 of current cases; Nigeria increase; surveillance and water control • Polio 1985-?: Gone from western hemisphere; problematic in Congo, Sudan, and Afghanistan; vaccination- and surveillance- based control. If Not Eradication, Then Control! "At this time one must question the wisdom of even contemplating another eradication effort until the two eradication programs now in progress have been successfully concluded, until the lessons from those programs have been digested and until the savings from polio eradication have begun to be realized. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Pharmacogenomic Associations Tables
Pharmacogenomic Associations Tables Disclaimer: This is educational material intended for health care professionals. This list is not comprehensive for all of the drugs in the pharmacopeia but focuses on commonly used drugs with high levels of evidence that the CYPs (CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4 and CYP3A5 only) and other select genes are relevant to a given drug’s metabolism. If a drug is not listed, there is not enough evidence for inclusion at this time. Other CYPs and other genes not described here may also be relevant but are out of scope for this document. This educational material is not intended to supersede the care provider’s experience and knowledge of her or his patient to establish a diagnosis or a treatment plan. All medications require careful clinical monitoring regardless of the information presented here. Table of Contents Table 1: Substrates of Cytochrome P450 (CYP) Enzymes Table 2: Inhibitors of Cytochrome P450 (CYP) Enzymes Table 3: Inducers of Cytochrome P450 (CYP) Enzymes Table 4: Alternate drugs NOT metabolized by CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4 or CYP3A5 enzymes Table 5: Glucose-6-Phosphate Dehydrogenase (G6PD) Associated Drugs and Compounds Table 6: Additional Pharmacogenomic Genes & Associated Drugs Table 1: Substrates of Cytochrome P450 (CYP) Enzymes Allergy Labetalol CYP2C19 Immunosuppressives Loratadine CYP3A4 Lidocaine CYP1A2 CYP2D6 Cyclosporine CYP3A4/5 Analgesic/Anesthesiology CYP3A4/5 Sirolimus CYP3A4/5 Losartan CYP2C9 CYP3A4/5 Codeine CYP2D6 activates Tacrolimus CYP3A4/5 Lovastatin -

Medicines Amendment Regulations 2018
2018/179 Medicines Amendment Regulations 2018 Patsy Reddy, Governor-General Order in Council At Wellington this 24th day of September 2018 Present: Her Excellency the Governor-General in Council These regulations are made under section 105(1)(j) of the Medicines Act 1981— (a) on the advice and with the consent of the Executive Council; and (b) on the advice of the Minister of Health tendered after consultation with the organisations or bodies appearing to the Minister to be representative of per- sons likely to be substantially affected. Contents Page 1 Title 1 2 Commencement 2 3 Principal regulations 2 4 Schedule 1 replaced 2 5 Regulations revoked 2 Schedule 2 Schedule 1 replaced Regulations 1 Title These regulations are the Medicines Amendment Regulations 2018. 1 r 2 Medicines Amendment Regulations 2018 2018/179 2 Commencement These regulations come into force on the 28th day after the date of their notifi- cation in the Gazette. 3 Principal regulations These regulations amend the Medicines Regulations 1984 (the principal regu- lations). 4 Schedule 1 replaced Replace Schedule 1 with the Schedule 1 set out in the Schedule of these regula- tions. 5 Regulations revoked The Medicines Amendment Regulations (No 2) 2015 (LI 2015/180) are revoked. Schedule Schedule 1 replaced r 4 Schedule 1 Prescription, restricted, and pharmacy-only medicines r 3 Every reference to a medicine in this schedule applies whether the medicine is syn- thetic in origin or is from biological or mineral sources. Unless specific reference is made otherwise, every reference applies also to medicines that are— • preparations and admixtures containing any proportion of any substance listed in this schedule: • salts and esters of any substance listed in this schedule: • preparations or extracts of biological materials listed in this schedule: • salts or oxides of elements listed in this schedule.