Re-Envisioning Anti-Apicomplexan Parasite Drug Discovery Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Molecular Data and the Evolutionary History of Dinoflagellates by Juan Fernando Saldarriaga Echavarria Diplom, Ruprecht-Karls-Un
Molecular data and the evolutionary history of dinoflagellates by Juan Fernando Saldarriaga Echavarria Diplom, Ruprecht-Karls-Universitat Heidelberg, 1993 A THESIS SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY in THE FACULTY OF GRADUATE STUDIES Department of Botany We accept this thesis as conforming to the required standard THE UNIVERSITY OF BRITISH COLUMBIA November 2003 © Juan Fernando Saldarriaga Echavarria, 2003 ABSTRACT New sequences of ribosomal and protein genes were combined with available morphological and paleontological data to produce a phylogenetic framework for dinoflagellates. The evolutionary history of some of the major morphological features of the group was then investigated in the light of that framework. Phylogenetic trees of dinoflagellates based on the small subunit ribosomal RNA gene (SSU) are generally poorly resolved but include many well- supported clades, and while combined analyses of SSU and LSU (large subunit ribosomal RNA) improve the support for several nodes, they are still generally unsatisfactory. Protein-gene based trees lack the degree of species representation necessary for meaningful in-group phylogenetic analyses, but do provide important insights to the phylogenetic position of dinoflagellates as a whole and on the identity of their close relatives. Molecular data agree with paleontology in suggesting an early evolutionary radiation of the group, but whereas paleontological data include only taxa with fossilizable cysts, the new data examined here establish that this radiation event included all dinokaryotic lineages, including athecate forms. Plastids were lost and replaced many times in dinoflagellates, a situation entirely unique for this group. Histones could well have been lost earlier in the lineage than previously assumed. -

Exploration of Laboratory Techniques Relating to Cryptosporidium Parvum Propagation, Life Cycle Observation, and Host Immune Responses to Infection
EXPLORATION OF LABORATORY TECHNIQUES RELATING TO CRYPTOSPORIDIUM PARVUM PROPAGATION, LIFE CYCLE OBSERVATION, AND HOST IMMUNE RESPONSES TO INFECTION A Thesis Submitted to the Graduate Faculty of the North Dakota State University of Agriculture and Applied Science By Cheryl Marie Brown In Partial Fulfillment for the Degree of MASTER OF SCIENCE Major Department: Veterinary and Microbiological Sciences February 2014 Fargo, North Dakota North Dakota State University Graduate School Title EXPLORATION OF LABORATORY TECHNIQUES RELATING TO CRYPTOSPORIDIUM PARVUM PROPAGATION, LIFE CYCLE OBSERVATION, AND HOST IMMUNE RESPONSES TO INFECTION By Cheryl Marie Brown The Supervisory Committee certifies that this disquisition complies with North Dakota State University’s regulations and meets the accepted standards for the degree of MASTER OF SCIENCE SUPERVISORY COMMITTEE: Dr. Jane Schuh Chair Dr. John McEvoy Dr. Carrie Hammer Approved: 4-8-14 Dr. Charlene Wolf-Hall Date Department Chair ii ABSTRACT Cryptosporidium causes cryptosporidiosis, a self-limiting diarrheal disease in healthy people, but causes serious health issues for immunocompromised individuals. Cryptosporidiosis has been observed in humans since the early 1970s and continues to cause public health concerns. Cryptosporidium has a complicated life cycle making laboratory study challenging. This project explores several ways of studying Cryptosporidium parvum, with a goal of applying existing techniques to further understand this life cycle. Utilization of a neonatal mouse model demonstrated laser microdissection as a tool for studying host immune response to infeciton. A cell culture technique developed on FrameSlides™ enables laser microdissection of individual infected cells for further analysis. Finally, the hypothesis that the availability of cells to infect drives the switch from asexual to sexual parasite reproduction was tested by time-series infection. -

The Transcriptome of the Avian Malaria Parasite Plasmodium
bioRxiv preprint doi: https://doi.org/10.1101/072454; this version posted August 31, 2016. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 The Transcriptome of the Avian Malaria Parasite 2 Plasmodium ashfordi Displays Host-Specific Gene 3 Expression 4 5 6 7 8 Running title 9 The Transcriptome of Plasmodium ashfordi 10 11 Authors 12 Elin Videvall1, Charlie K. Cornwallis1, Dag Ahrén1,3, Vaidas Palinauskas2, Gediminas Valkiūnas2, 13 Olof Hellgren1 14 15 Affiliation 16 1Department of Biology, Lund University, Lund, Sweden 17 2Institute of Ecology, Nature Research Centre, Vilnius, Lithuania 18 3National Bioinformatics Infrastructure Sweden (NBIS), Lund University, Lund, Sweden 19 20 Corresponding authors 21 Elin Videvall ([email protected]) 22 Olof Hellgren ([email protected]) 23 24 1 bioRxiv preprint doi: https://doi.org/10.1101/072454; this version posted August 31, 2016. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 25 Abstract 26 27 Malaria parasites (Plasmodium spp.) include some of the world’s most widespread and virulent 28 pathogens, infecting a wide array of vertebrates. Our knowledge of the molecular mechanisms these 29 parasites use to invade and exploit hosts other than mice and primates is, however, extremely limited. 30 How do Plasmodium adapt to individual hosts and to the immune response of hosts throughout an 31 infection? To better understand parasite plasticity, and identify genes that are conserved across the 32 phylogeny, it is imperative that we characterize transcriptome-wide gene expression from non-model 33 malaria parasites in multiple host individuals. -

Download the Abstract Book
1 Exploring the male-induced female reproduction of Schistosoma mansoni in a novel medium Jipeng Wang1, Rui Chen1, James Collins1 1) UT Southwestern Medical Center. Schistosomiasis is a neglected tropical disease caused by schistosome parasites that infect over 200 million people. The prodigious egg output of these parasites is the sole driver of pathology due to infection. Female schistosomes rely on continuous pairing with male worms to fuel the maturation of their reproductive organs, yet our understanding of their sexual reproduction is limited because egg production is not sustained for more than a few days in vitro. Here, we explore the process of male-stimulated female maturation in our newly developed ABC169 medium and demonstrate that physical contact with a male worm, and not insemination, is sufficient to induce female development and the production of viable parthenogenetic haploid embryos. By performing an RNAi screen for genes whose expression was enriched in the female reproductive organs, we identify a single nuclear hormone receptor that is required for differentiation and maturation of germ line stem cells in female gonad. Furthermore, we screen genes in non-reproductive tissues that maybe involved in mediating cell signaling during the male-female interplay and identify a transcription factor gli1 whose knockdown prevents male worms from inducing the female sexual maturation while having no effect on male:female pairing. Using RNA-seq, we characterize the gene expression changes of male worms after gli1 knockdown as well as the female transcriptomic changes after pairing with gli1-knockdown males. We are currently exploring the downstream genes of this transcription factor that may mediate the male stimulus associated with pairing. -

Real-Time Dynamics of Plasmodium NDC80 Reveals Unusual Modes of Chromosome Segregation During Parasite Proliferation Mohammad Zeeshan1,*, Rajan Pandey1,*, David J
© 2020. Published by The Company of Biologists Ltd | Journal of Cell Science (2021) 134, jcs245753. doi:10.1242/jcs.245753 RESEARCH ARTICLE SPECIAL ISSUE: CELL BIOLOGY OF HOST–PATHOGEN INTERACTIONS Real-time dynamics of Plasmodium NDC80 reveals unusual modes of chromosome segregation during parasite proliferation Mohammad Zeeshan1,*, Rajan Pandey1,*, David J. P. Ferguson2,3, Eelco C. Tromer4, Robert Markus1, Steven Abel5, Declan Brady1, Emilie Daniel1, Rebecca Limenitakis6, Andrew R. Bottrill7, Karine G. Le Roch5, Anthony A. Holder8, Ross F. Waller4, David S. Guttery9 and Rita Tewari1,‡ ABSTRACT eukaryotic organisms to proliferate, propagate and survive. During Eukaryotic cell proliferation requires chromosome replication and these processes, microtubular spindles form to facilitate an equal precise segregation to ensure daughter cells have identical genomic segregation of duplicated chromosomes to the spindle poles. copies. Species of the genus Plasmodium, the causative agents of Chromosome attachment to spindle microtubules (MTs) is malaria, display remarkable aspects of nuclear division throughout their mediated by kinetochores, which are large multiprotein complexes life cycle to meet some peculiar and unique challenges to DNA assembled on centromeres located at the constriction point of sister replication and chromosome segregation. The parasite undergoes chromatids (Cheeseman, 2014; McKinley and Cheeseman, 2016; atypical endomitosis and endoreduplication with an intact nuclear Musacchio and Desai, 2017; Vader and Musacchio, 2017). Each membrane and intranuclear mitotic spindle. To understand these diverse sister chromatid has its own kinetochore, oriented to facilitate modes of Plasmodium cell division, we have studied the behaviour movement to opposite poles of the spindle apparatus. During and composition of the outer kinetochore NDC80 complex, a key part of anaphase, the spindle elongates and the sister chromatids separate, the mitotic apparatus that attaches the centromere of chromosomes to resulting in segregation of the two genomes during telophase. -
Unlicensed Medicines List for Suffolk D&T
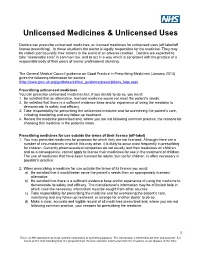
Unlicensed Medicines & Unlicensed Uses Doctors can prescribe unlicensed medicines, or licensed medicines for unlicensed uses (off-label/off license prescribing). In these situations the doctor is legally responsible for the medicine. They may be called upon to justify their actions in the event of an adverse reaction. Doctors are expected to take “reasonable care” in common law, and to act in a way which is consistent with the practice of a responsible body of their peers of similar professional standing. The General Medical Council guidance on Good Practice in Prescribing Medicines (January 2013) gives the following information for doctors (http://www.gmc-uk.org/guidance/ethical_guidance/prescriptions_faqs.asp) Prescribing unlicensed medicines You can prescribe unlicensed medicines but, if you decide to do so, you must: 1. Be satisfied that an alternative, licensed medicine would not meet the patient's needs. 2. Be satisfied that there is a sufficient evidence base and/or experience of using the medicine to demonstrate its safety and efficacy. 3. Take responsibility for prescribing the unlicensed medicine and for overseeing the patient's care, including monitoring and any follow up treatment. 4. Record the medicine prescribed and, where you are not following common practice, the reasons for choosing this medicine in the patient's notes. Prescribing medicines for use outside the terms of their licence (off-label) 1. You may prescribe medicines for purposes for which they are not licensed. Although there are a number of circumstances in which this may arise, it is likely to occur most frequently in prescribing for children. Currently pharmaceutical companies do not usually test their medicines on children and as a consequence, cannot apply to license their medicines for use in the treatment of children. -

Looking Under the Skin: the First Steps in Malarial Infection and Immunity
REVIEWS Looking under the skin: the first steps in malarial infection and immunity Robert Ménard1, Joana Tavares1, Ian Cockburn2, Miles Markus3, Fidel Zavala4 and Rogerio Amino1 Abstract | Malaria, which is caused by Plasmodium spp., starts with an asymptomatic phase, during which sporozoites, the parasite form that is injected into the skin by a mosquito, develop into merozoites, the form that infects erythrocytes. This pre-erythrocytic phase is still the most enigmatic in the parasite life cycle, but has long been recognized as an attractive vaccination target. In this Review, we present what has been learned in recent years about the natural history of the pre-erythrocytic stages, mainly using intravital imaging in rodents. We also consider how this new knowledge is in turn changing our understanding of the immune response mounted by the host against the pre-erythrocytic forms. Sterilizing immunity Malaria is the most deadly parasitic infection of humans. subject of intensive immunological research ever since Immunity resulting in parasite Although economic development and the implementa- the first demonstrations, in animal models and humans, clearance from the host. tion of control measures during the twentieth century that injection of attenuated parasites which do not cause have eliminated malaria from many areas of the world1, blood infection confers protection against sporozoite the disease is still rampant in the tropics and in the poor- challenge4–6. Today, this vaccination method is still 1Institut Pasteur, Unité de est regions of the globe, affecting 3 billion people and the most efficient at offering sterilizing immunity against Biologie et Génétique du 2 Paludisme, 28 Rue du Dr Roux, killing up to 1 million annually . -

Artemisia Annua and Artemisinins Are Ineffective Against Human Babesia Microti and Six Candida Sp
13 Original Article Page 1 of 13 Artemisia annua and artemisinins are ineffective against human Babesia microti and six Candida sp Mostafa A. Elfawal1, Olivia Gray2, Claire Dickson-Burke2, Pamela J. Weathers2, Stephen M. Rich1 1Laboratory of Medical Zoology, Department of Microbiology, University Massachusetts, Amherst, MA, USA; 2Department of Biology and Biotechnology, Worcester Polytechnic Institute, Worcester, MA, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: PJ Weathers, SM Rich; (III) Provision of study materials: PJ Weathers; (IV) Collection and assembly of data: MA Elfawal, O Gray, C Dickson-Burke; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors Correspondence to: Pamela J. Weathers. Department of Biology and Biotechnology, Worcester Polytechnic Institute, 100 Institute Rd, Worcester, MA 01609, USA. Email: [email protected]. Background: Artemisia annua L.is a well-established medicinal herb used for millennia to treat parasites and fever-related ailments caused by various microbes. Although effective against many infectious agents, the plant is not a miracle cure and there are infections where it has proved ineffective or limited. It is important to report those failures. Methods: Here artemisinin, artesunate and dried leaf slurries of A. annua were used daily for 6 days in vivo against Babesia microti in mice 2 days post infection at 100 µg artemisinin/kg body weight. Parasitemia was measure before and 15 days days post treatment. Artemisinin and extracts of A. annua also were tested in vitro against six Candida sp. at artemisinin concentrations up to 180 µM and growth measured after cultures were fed drugs once at different stages of growth and also after repeated dosing. -

Pharmaceutical Compositions Comprising Hydroxychloroquine (HCQ), Curcumin, Piperine/ Bioperine and Uses Thereof in the Medical Field
(19) TZZ 56_8A_T (11) EP 2 561 868 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 27.02.2013 Bulletin 2013/09 A61K 31/12 (2006.01) A61K 31/4706 (2006.01) A61K 45/06 (2006.01) A61P 35/00 (2006.01) (21) Application number: 11178638.0 (22) Date of filing: 24.08.2011 (84) Designated Contracting States: (72) Inventor: Van Oosten, Anton Bernhard AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 3920 Lommel (BE) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR (74) Representative: DeltaPatents B.V. Designated Extension States: Fellenoord 370 BA ME 5611 ZL Eindhoven (NL) (71) Applicant: Van Oosten, Anton Bernhard 3920 Lommel (BE) (54) Pharmaceutical compositions comprising hydroxychloroquine (HCQ), Curcumin, Piperine/ BioPerine and uses thereof in the medical field (57) The present invention concerns a pharmaceuti- of a premalignant plasma cell proliferative disorder like cal composition containing HCQ, curcumin and BioPer- a monoclonal gammopathy of undetermined significance ine/piperine and its application in the medical field. In (MGUS) and/or smoldering (asymptomatic) multiple my- particular, the composition according to the invention can eloma (SMM) and/or Indolent multiple myeloma (IMM) be advantageously employed in the prevention or treat- and/or to cause remission of a cancer arising from a pre- ment of a subject presenting with a proliferative disorder, malignant plasma cell proliferative disorder like multiple to slow the progression of and/or or to cause regression myeloma (MM). -

Treatment of Relapsing Malaria with Specific Antimalarial Drugs In
Sept., 1947 J TREATMENT OF RELAPSING MALARIA: DESHMUKH 511 up to the expectation. But it soon became Articles clear that they did not control relapse, and Original also that they carry with them a danger of toxicity. Arsenic is notorious for causing to TREATMENT of relapsing malaria damage liver, kidneys and brain. When pregnancy complicates malaria, the use of WITH SPECIFIC ANTIMALARIAL quinine and arsenic may be particularly risky DRUGS IN COMBINATION WITH and one is on the horns of a dilemma as regards PENICILLIN the satisfactory treatment in such circumstances. The writer's experience of arsenicals in By P. L. DESHMUKH, m.d. (Bom.), malaria has been borne out other workers F.C.P.S. by D.T.M.\& II. (Lond.), and their findings in large-scale experiments Poona Sassoon Hospitals, given below will help to dislodge from the minds It must be admitted that even with quinine of the clinicians any lingering faith in arsenic and the synthetic antimalarial drugs like as an ideal antimalarial drug. atabrine, mepacrine, etc. (henceforth called Professor Blacklock (1944) has pointed out specific antimalarials ' for the sake of after long studies at the Liverpool school that tee brevity) treatment of malaria is still very unsatis- though the immediate effects of arsenic in factory. The recognized failure of the specific relapsing malaria were striking, the ultimate antimalarials singly or in combination to control results were disappointing in that practically relapses materially is a matter of great all cases relapsed even after full arsenical concern. A great variation is observed in the treatment. Thus, arsenicals though immediately mterval that may before the occurrence effective against vivax parasites do not eliminate a elapse y relapse. -

The Rise to Prominence of Artemisia Annua L. – the Transformation of a Chinese Plant to a Global Pharmaceutical
24 AFRIcaN SOCIologIcal REVIEW 14(2) 2010 The rise to prominence of Artemisia annua L. – the transformation of a Chinese plant to a global pharmaceutical Caroline Meier zu Biesen Institute of Social and Cultural Anthropology, Landoltweg 9-11 14195 Berlin, Germany [email protected] Abstract This paper focuses on the transformation of a recently promoted medicinal plant named Artemisia annua L. For over 2000 years, the Chinese have used A. annua as a herbal tea preparation against malaria. Pharmacological studies led to the isolation of artemisinin as the principal anti-malarial compound. Since 2001, the World Health Organisation (WHO) has recommended artemisinin-based combined therapies (‘ACTs’) for the treatment of malaria – Novartis is the leading actor to extract the compound in tablet form. In the 1990s, A. annua was introduced to Tanzania. Beside the local plant-based promotion of Artemisia-tea as an efficient, inexpensive natural practice to treat malaria, Tanzania hosts influential actors who seek to commercialise the plant. By following the biography of the Chinese medicinal plant, its global transfer, production, marketing, distribution, consumption, and its transformation to a highly demanded commodity, the paper critically reveals the dialectics and reciprocities between different actors and their relation to existing powerful reference systems (such as WHO, Pharmaceutical Industry). Keywords: Artemisia annua L., artemisinin, Tanzania, ACT, effectiveness, social life of medicines “Artemisia (Artemisia annua) is a seemingly simple, though versatile, medicinal plant suddenly at the heart of international attention. It was long a traditional remedy for a variety of ills. But by virtue of the extraordinary qualities of a puri- fied extract, artemisinin, it is now a key player in global efforts to help control malaria, particularly in Africa where it is a particular scourge. -

Artemisia Annua L., Potential Source of Molecules with Pharmacological Activity in Human Diseases Luz Estella Mesa*1,2, Pierre Lutgen3, Ivan D
Original Article Artemisia annua L., Potential Source of Molecules with Pharmacological Activity in Human Diseases Luz Estella Mesa*1,2, Pierre Lutgen3, Ivan D. Velez1, Angela M. Segura2 and Sara M. Robledo1 1PECET- Medical Research Institute, School of Medicine, University of Antioquia-UdeA. Calle 70 # 52-21, Medellin-Colombia 2Epidemiology and Biostatistic, Universidad CES Calle 10 A No. 22 - 04. Medellin-Colombia 3IFBV-BELHERB, PO Box 98, L-6905 Niederanven, Luxembourg ABSTRACT Objective: This review intends to motivate and encourage researchers to explore new alternatives to treat different diseases with Artemisia annua L., an important plant of traditional Chinese pharmacopoeia that has been used for more than 2.000 years in the treatment of different diseases, mainly malaria. Methods: Data include currently available information about A. annua, its origin, traditional use in medicine, pharmacological activity, toxicity and main metabolites with reported clinical activity. The information was collected by literature search on web databases such as Pubmed and Google Scholar up to 2014 on publications about the medicinal uses of A. annua L., in the treatment of different diseases that affect humans but also some animals. Results: Pharmacological activity against chronic and infectious diseases of various metabolites from A. annua, artemisinin and its derivatives, flavonoids and essential oils, reported in this review, is supported by preclinical experimental evidence both in vivo and in vitro and clinical observations in human beings of different parts of Address for the plant, mainly leaves, in the treatment of malaria. Leaves, seeds Correspondence and whole plant of A. annua have also proved pharmacological activity against parasites responsible of leishmaniasis and Chagas PECET- Medical disease.