Plasmodium Asexual Growth and Sexual Development in the Haematopoietic Niche of the Host
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Basal Body Structure and Composition in the Apicomplexans Toxoplasma and Plasmodium Maria E
Francia et al. Cilia (2016) 5:3 DOI 10.1186/s13630-016-0025-5 Cilia REVIEW Open Access Basal body structure and composition in the apicomplexans Toxoplasma and Plasmodium Maria E. Francia1* , Jean‑Francois Dubremetz2 and Naomi S. Morrissette3 Abstract The phylum Apicomplexa encompasses numerous important human and animal disease-causing parasites, includ‑ ing the Plasmodium species, and Toxoplasma gondii, causative agents of malaria and toxoplasmosis, respectively. Apicomplexans proliferate by asexual replication and can also undergo sexual recombination. Most life cycle stages of the parasite lack flagella; these structures only appear on male gametes. Although male gametes (microgametes) assemble a typical 9 2 axoneme, the structure of the templating basal body is poorly defined. Moreover, the rela‑ tionship between asexual+ stage centrioles and microgamete basal bodies remains unclear. While asexual stages of Plasmodium lack defined centriole structures, the asexual stages of Toxoplasma and closely related coccidian api‑ complexans contain centrioles that consist of nine singlet microtubules and a central tubule. There are relatively few ultra-structural images of Toxoplasma microgametes, which only develop in cat intestinal epithelium. Only a subset of these include sections through the basal body: to date, none have unambiguously captured organization of the basal body structure. Moreover, it is unclear whether this basal body is derived from pre-existing asexual stage centrioles or is synthesized de novo. Basal bodies in Plasmodium microgametes are thought to be synthesized de novo, and their assembly remains ill-defined. Apicomplexan genomes harbor genes encoding δ- and ε-tubulin homologs, potentially enabling these parasites to assemble a typical triplet basal body structure. -

First Description of Cryptosporidium Parvum in Carrier Pigeons
Veterinary Parasitology 243 (2017) 148–150 Contents lists available at ScienceDirect Veterinary Parasitology journal homepage: www.elsevier.com/locate/vetpar Research paper First description of Cryptosporidium parvum in carrier pigeons (Columba livia) MARK Bruno César Miranda Oliveiraa, Elis Domingos Ferraria, Mariele Fernanda da Cruz Panegossia, Alex Akira Nakamuraa, Flávio Sader Corbuccia, Walter Bertequini Nagataa, Bianca Martins dos Santosb, Jancarlo Ferreira Gomesb, Marcelo Vasconcelos Meirelesa, ⁎ Giovanni Widmerc, Katia Denise Saraiva Brescianid, a Universidade Estadual Paulista (Unesp), Faculdade de Medicina Veterinária, Araçatuba, Brazil b Laboratory of Visual Informatics in Biomedical and Health, Institute of Computing, University of Campinas – UNICAMP, São Paulo, Brazil c Department of Infectious Disease & Global Health, Cummings School of Veterinary Medicine at Tufts University, North Grafton, MA, USA d Universidade Estadual Paulista (Unesp), Faculdade de Medicina Veterinária, Araçatuba. Rua Clóvis Pestana, 793, Jardim Dona Amélia, cep 16050-680, Araçatuba, São Paulo, Brazil ARTICLE INFO ABSTRACT Keywords: The carrier pigeon and the domestic pigeon are different breeds of the species Columba livia. Carrier pigeons are Birds used for recreational activities such as bird contests and exhibitions. Due to the close contact with humans, these Carrier pigeons birds may potentially represent a public health risk, since they can host and disseminate zoonotic parasites, such Columba livia as those belonging to the genus Cryptosporidium (phylum Apicomplexa). The purpose of this work was the de- Cryptosporidiosis tection by microscopic and molecular techniques of Cryptosporidium spp. oocysts in fecal samples of carrier Cryptosporidium parvum pigeons, and subsequently to sequence the 18S ribosomal RNA marker of positive samples to identify the species. Nested PCR A total of 100 fecal samples were collected individually in two pigeon breeding facilities from Formiga and Araçatuba, cities located in Minas Gerais state and São Paulo state, Brazil, respectively. -

And Toxoplasmosis in Jackass Penguins in South Africa
IMMUNOLOGICAL SURVEY OF BABESIOSIS (BABESIA PEIRCEI) AND TOXOPLASMOSIS IN JACKASS PENGUINS IN SOUTH AFRICA GRACZYK T.K.', B1~OSSY J.].", SA DERS M.L. ', D UBEY J.P.···, PLOS A .. ••• & STOSKOPF M. K .. •••• Sununary : ReSlIlIle: E x-I1V\c n oN l~ lIrIUSATION D'Ar\'"TIGENE DE B ;IB£,'lA PH/Re El EN ELISA ET simoNi,cATIVlTli t'OUR 7 bxo l'l.ASMA GONIJfI DE SI'I-IENICUS was extracted from nucleated erythrocytes Babesia peircei of IJEMIiNSUS EN ArRIQUE D U SUD naturally infected Jackass penguin (Spheniscus demersus) from South Africo (SA). Babesia peircei glycoprotein·enriched fractions Babesia peircei a ele extra it d 'erythrocytes nue/fies p,ovenanl de Sphenicus demersus originoires d 'Afrique du Sud infectes were obto ined by conca navalin A-Sepharose affinity column natulellement. Des fractions de Babesia peircei enrichies en chromatogrophy and separated by sod ium dodecyl sulphate glycoproleines onl ele oblenues par chromatographie sur colonne polyacrylam ide gel electrophoresis (SDS-PAGE ). At least d 'alfinite concona valine A-Sephorose et separees par 14 protein bonds (9, 11, 13, 20, 22, 23, 24, 43, 62, 90, electrophorese en gel de polyacrylamide-dodecylsuJfale de sodium 120, 204, and 205 kDa) were observed, with the major protein (SOS'PAGE) Q uotorze bandes proleiques au minimum ont ete at 25 kDa. Blood samples of 191 adult S. demersus were tes ted observees (9, 1 I, 13, 20, 22, 23, 24, 43, 62, 90, 120, 204, by enzyme-linked immunosorbent assoy (ELISA) utilizing B. peircei et 205 Wa), 10 proleine ma;eure elant de 25 Wo. -

Malaria History
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this material constitutes acceptance of that license and the conditions of use of materials on this site. Copyright 2006, The Johns Hopkins University and David Sullivan. All rights reserved. Use of these materials permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for obtaining permissions for use from third parties as needed. Malariology Overview History, Lifecycle, Epidemiology, Pathology, and Control David Sullivan, MD Malaria History • 2700 BCE: The Nei Ching (Chinese Canon of Medicine) discussed malaria symptoms and the relationship between fevers and enlarged spleens. • 1550 BCE: The Ebers Papyrus mentions fevers, rigors, splenomegaly, and oil from Balantines tree as mosquito repellent. • 6th century BCE: Cuneiform tablets mention deadly malaria-like fevers affecting Mesopotamia. • Hippocrates from studies in Egypt was first to make connection between nearness of stagnant bodies of water and occurrence of fevers in local population. • Romans also associated marshes with fever and pioneered efforts to drain swamps. • Italian: “aria cattiva” = bad air; “mal aria” = bad air. • French: “paludisme” = rooted in swamp. Cure Before Etiology: Mid 17th Century - Three Theories • PC Garnham relates that following: An earthquake caused destruction in Loxa in which many cinchona trees collapsed and fell into small lake or pond and water became very bitter as to be almost undrinkable. Yet an Indian so thirsty with a violent fever quenched his thirst with this cinchona bark contaminated water and was better in a day or two. -
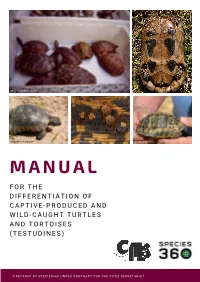
Manual for the Differentiation of Captive-Produced and Wild-Caught Turtles and Tortoises (Testudines)
Image: Peter Paul van Dijk Image:Henrik Bringsøe Image: Henrik Bringsøe Image: Andrei Daniel Mihalca Image: Beate Pfau MANUAL F O R T H E DIFFERENTIATION OF CAPTIVE-PRODUCED AND WILD-CAUGHT TURTLES AND TORTOISES (TESTUDINES) PREPARED BY SPECIES360 UNDER CONTRACT FOR THE CITES SECRETARIAT Manual for the differentiation of captive-produced and wild-caught turtles and tortoises (Testudines) This document was prepared by Species360 under contract for the CITES Secretariat. Principal Investigators: Prof. Dalia A. Conde, Ph.D. and Johanna Staerk, Ph.D., Species360 Conservation Science Alliance, https://www.species360.orG Authors: Johanna Staerk1,2, A. Rita da Silva1,2, Lionel Jouvet 1,2, Peter Paul van Dijk3,4,5, Beate Pfau5, Ioanna Alexiadou1,2 and Dalia A. Conde 1,2 Affiliations: 1 Species360 Conservation Science Alliance, www.species360.orG,2 Center on Population Dynamics (CPop), Department of Biology, University of Southern Denmark, Denmark, 3 The Turtle Conservancy, www.turtleconservancy.orG , 4 Global Wildlife Conservation, globalwildlife.orG , 5 IUCN SSC Tortoise & Freshwater Turtle Specialist Group, www.iucn-tftsG.org. 6 Deutsche Gesellschaft für HerpetoloGie und Terrarienkunde (DGHT) Images (title page): First row, left: Mixed species shipment (imaGe taken by Peter Paul van Dijk) First row, riGht: Wild Testudo marginata from Greece with damaGe of the plastron (imaGe taken by Henrik BrinGsøe) Second row, left: Wild Testudo marginata from Greece with minor damaGe of the carapace (imaGe taken by Henrik BrinGsøe) Second row, middle: Ticks on tortoise shell (Amblyomma sp. in Geochelone pardalis) (imaGe taken by Andrei Daniel Mihalca) Second row, riGht: Testudo graeca with doG bite marks (imaGe taken by Beate Pfau) Acknowledgements: The development of this manual would not have been possible without the help, support and guidance of many people. -
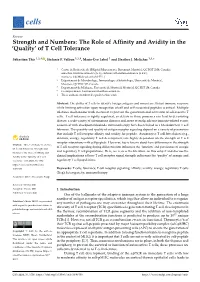
Of T Cell Tolerance
cells Review Strength and Numbers: The Role of Affinity and Avidity in the ‘Quality’ of T Cell Tolerance Sébastien This 1,2,† , Stefanie F. Valbon 1,2,†, Marie-Ève Lebel 1 and Heather J. Melichar 1,3,* 1 Centre de Recherche de l’Hôpital Maisonneuve-Rosemont, Montréal, QC H1T 2M4, Canada; [email protected] (S.T.); [email protected] (S.F.V.); [email protected] (M.-È.L.) 2 Département de Microbiologie, Immunologie et Infectiologie, Université de Montréal, Montréal, QC H3C 3J7, Canada 3 Département de Médecine, Université de Montréal, Montréal, QC H3T 1J4, Canada * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The ability of T cells to identify foreign antigens and mount an efficient immune response while limiting activation upon recognition of self and self-associated peptides is critical. Multiple tolerance mechanisms work in concert to prevent the generation and activation of self-reactive T cells. T cell tolerance is tightly regulated, as defects in these processes can lead to devastating disease; a wide variety of autoimmune diseases and, more recently, adverse immune-related events associated with checkpoint blockade immunotherapy have been linked to a breakdown in T cell tolerance. The quantity and quality of antigen receptor signaling depend on a variety of parameters that include T cell receptor affinity and avidity for peptide. Autoreactive T cell fate choices (e.g., deletion, anergy, regulatory T cell development) are highly dependent on the strength of T cell receptor interactions with self-peptide. However, less is known about how differences in the strength Citation: This, S.; Valbon, S.F.; Lebel, of T cell receptor signaling during differentiation influences the ‘function’ and persistence of anergic M.-È.; Melichar, H.J. -

Malaria: Bad for Business Why Investing in Ending Malaria Provides Some of the Highest Economic Returns
Malaria: Bad for business Why investing in ending malaria provides some of the highest economic returns. Malaria’s burden on the health and wealth of nations While huge progress has been made in recent years, one of the most striking signs of the global impact of the 215 million cases of malaria reported last year is that up to 40% of public health spending goes on the disease in the most heavily affected countries. But malaria reaches far beyond public health, taking its toll on households, local and multinational business profits, and national economic development. Critically, annual economic growth in countries with high malaria transmission has historically been lower than in countries without malaria. In some African countries, malaria reduces GDP growth up to an estimated 1.3%. Malaria costs productivity. Adults are forced to be absent from work, children miss school, and households spend disproportionately on health when they can least afford it. But it need not be this way. With developing countries, donors and private sector firms beginning to take real action, we can be the generation that ends malaria for good and boosts prosperity for all. The economic growth penalty Malaria’s impact on national economies Malaria and poverty occupy common ground. Where the burden of malaria is highest, economic prosperity is lowest. We know that poverty can promote malaria transmission, and that malaria causes poverty by blocking economic growth. Research shows that malaria can strain national economics, having a deleterious impact on some nations’ GDP by as much as an estimated 5 - 6%. It keeps households in poverty, discourages domestic and foreign investment and tourism, affects land use patterns, and reduces productivity through lost work days and diminished job performance. -

Costs of Avian Malaria in Austral-Papuan Avifauna
Association of Avian Veterinarians Australasian Committee Ltd. Annual Conference 2016 pp 67-71 Costs of Avian Malaria in Australo-Papuan Avifauna Lee Peacock BSc (Vet) BVSc (Hons)1, Anders Gonçalves da Silva PhD2, Rohan Clarke PhD3 1. PhD Candidate Monash University 2. University of Melbourne 3. Monash University Clayton VIC 3800 Parkville. VIC. 2010. Wellington Rd. And Blackburn Rd. [email protected] Clayton. VIC. 3800 Introduction factors. These parasites are thus not detected evenly throughout their distribution; instead a mosaic pat- Avian malarial parasites are represented by a large tern nested within a general trend of higher diversity diversity of haemosporida within Plasmodiidae and and prevalence at lower altitudes and latitudes is ob- Haemoproteidae families. Other closely related hae- served (Mendes et al., 2005; Wood et al., 2007; Clark mosporida from Leukocytozoidae and Garniidae also et al., 2016). Large-scale migratory movements of infect birds and are often discussed under the um- avian hosts and near life-long infections mean these brella of avian malaria. Each family differs in life-cy- parasites can move within their avian hosts well be- cle, host and vector specificity, distribution, and yond current transmission zones, effectively expand- pathogenicity. ing their distribution. Avian malarial infections are described as acute, Avian malaria is associated with island bird extinc- chronic and abortive (Valkiunas 2004b; Valkiunas tions and can impose significant restrictions to avi- 2011). The acute phase is distinguished by a rising an distributions ( Warner 1968; van Riper III et al., parasitaemia, occurring after a latent or prepatent 1982). This is in stark contrast to evidence reveal- period following inoculation. -

Reconstruction of the Evolutionary History of Haemosporida
Parasitology International 65 (2016) 5–11 Contents lists available at ScienceDirect Parasitology International journal homepage: www.elsevier.com/locate/parint Reconstruction of the evolutionary history of Haemosporida (Apicomplexa) based on the cyt b gene with characterization of Haemocystidium in geckos (Squamata: Gekkota) from Oman João P. Maia a,b,c,⁎, D. James Harris a,b, Salvador Carranza c a CIBIO Research Centre in Biodiversity and Genetic Resources, InBIO, Universidade do Porto, Campus Agrário de Vairão, Rua Padre Armando Quintas, N° 7, 4485-661 Vairão, Vila do Conde, Portugal b Departamento de Biologia, Faculdade de Ciências, Universidade do Porto, Rua do Campo Alegre FC4 4169-007 Porto, Portugal c Institut de Biologia Evolutiva (CSIC-Universitat Pompeu Fabra), Passeig Maritím de la Barceloneta, 37-49, 08003 Barcelona, Spain article info abstract Article history: The order Haemosporida (Apicomplexa) includes many medically important parasites. Knowledge on the diver- Received 4 April 2015 sity and distribution of Haemosporida has increased in recent years, but remains less known in reptiles and their Received in revised form 7 September 2015 taxonomy is still uncertain. Further, estimates of evolutionary relationships of this order tend to change when Accepted 10 September 2015 new genes, taxa, outgroups or alternative methodologies are used. We inferred an updated phylogeny for the Available online 12 September 2015 Cytochrome b gene (cyt b) of Haemosporida and screened a total of 80 blood smears from 17 lizard species from Oman belonging to 11 genera. The inclusion of previously underrepresented genera resulted in an alterna- Keywords: Haemoproteus tive estimate of phylogeny for Haemosporida based on the cyt b gene. -

Wildlife Parasitology in Australia: Past, Present and Future
CSIRO PUBLISHING Australian Journal of Zoology, 2018, 66, 286–305 Review https://doi.org/10.1071/ZO19017 Wildlife parasitology in Australia: past, present and future David M. Spratt A,C and Ian Beveridge B AAustralian National Wildlife Collection, National Research Collections Australia, CSIRO, GPO Box 1700, Canberra, ACT 2601, Australia. BVeterinary Clinical Centre, Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Werribee, Vic. 3030, Australia. CCorresponding author. Email: [email protected] Abstract. Wildlife parasitology is a highly diverse area of research encompassing many fields including taxonomy, ecology, pathology and epidemiology, and with participants from extremely disparate scientific fields. In addition, the organisms studied are highly dissimilar, ranging from platyhelminths, nematodes and acanthocephalans to insects, arachnids, crustaceans and protists. This review of the parasites of wildlife in Australia highlights the advances made to date, focussing on the work, interests and major findings of researchers over the years and identifies current significant gaps that exist in our understanding. The review is divided into three sections covering protist, helminth and arthropod parasites. The challenge to document the diversity of parasites in Australia continues at a traditional level but the advent of molecular methods has heightened the significance of this issue. Modern methods are providing an avenue for major advances in documenting and restructuring the phylogeny of protistan parasites in particular, while facilitating the recognition of species complexes in helminth taxa previously defined by traditional morphological methods. The life cycles, ecology and general biology of most parasites of wildlife in Australia are extremely poorly understood. While the phylogenetic origins of the Australian vertebrate fauna are complex, so too are the likely origins of their parasites, which do not necessarily mirror those of their hosts. -

Studies on Blood Parasites of Birds in Coles County, Illinois Edward G
Eastern Illinois University The Keep Masters Theses Student Theses & Publications 1968 Studies on Blood Parasites of Birds in Coles County, Illinois Edward G. Fox Eastern Illinois University This research is a product of the graduate program in Zoology at Eastern Illinois University. Find out more about the program. Recommended Citation Fox, Edward G., "Studies on Blood Parasites of Birds in Coles County, Illinois" (1968). Masters Theses. 4148. https://thekeep.eiu.edu/theses/4148 This is brought to you for free and open access by the Student Theses & Publications at The Keep. It has been accepted for inclusion in Masters Theses by an authorized administrator of The Keep. For more information, please contact [email protected]. PAPER CERTIFICATE #3 To: Graduate Degree Candidates who have written formal theses. Subject: Permission to reproduce theses. The University Library is receiving a number of requests from other institutions asking permission to reproduce dissertations for inclusion in their library holdings. Although no copyright laws are involved, we feel that professional courtesy demands that permission be obtained from the author before we allow theses to be copied. Please sign one of the following statements. Booth Library of Eastern Illinois University has my permission to lend my thesis to a reputable college or university for the purpose of copying it for inclusion in that institution's library or research holdings. I respectfully request Booth Library of Eastern Illinois University not allow my thesis be reproduced because------------- Date Author STUDIES CB BLOOD PARA.SIDS 0, BlRDS Xlf COLES COUIITY, tI,JJJIOXI (TITLE) BY Bdward G. iox B. s. -

Real-Time Dynamics of Plasmodium NDC80 Reveals Unusual Modes of Chromosome Segregation During Parasite Proliferation Mohammad Zeeshan1,*, Rajan Pandey1,*, David J
© 2020. Published by The Company of Biologists Ltd | Journal of Cell Science (2021) 134, jcs245753. doi:10.1242/jcs.245753 RESEARCH ARTICLE SPECIAL ISSUE: CELL BIOLOGY OF HOST–PATHOGEN INTERACTIONS Real-time dynamics of Plasmodium NDC80 reveals unusual modes of chromosome segregation during parasite proliferation Mohammad Zeeshan1,*, Rajan Pandey1,*, David J. P. Ferguson2,3, Eelco C. Tromer4, Robert Markus1, Steven Abel5, Declan Brady1, Emilie Daniel1, Rebecca Limenitakis6, Andrew R. Bottrill7, Karine G. Le Roch5, Anthony A. Holder8, Ross F. Waller4, David S. Guttery9 and Rita Tewari1,‡ ABSTRACT eukaryotic organisms to proliferate, propagate and survive. During Eukaryotic cell proliferation requires chromosome replication and these processes, microtubular spindles form to facilitate an equal precise segregation to ensure daughter cells have identical genomic segregation of duplicated chromosomes to the spindle poles. copies. Species of the genus Plasmodium, the causative agents of Chromosome attachment to spindle microtubules (MTs) is malaria, display remarkable aspects of nuclear division throughout their mediated by kinetochores, which are large multiprotein complexes life cycle to meet some peculiar and unique challenges to DNA assembled on centromeres located at the constriction point of sister replication and chromosome segregation. The parasite undergoes chromatids (Cheeseman, 2014; McKinley and Cheeseman, 2016; atypical endomitosis and endoreduplication with an intact nuclear Musacchio and Desai, 2017; Vader and Musacchio, 2017). Each membrane and intranuclear mitotic spindle. To understand these diverse sister chromatid has its own kinetochore, oriented to facilitate modes of Plasmodium cell division, we have studied the behaviour movement to opposite poles of the spindle apparatus. During and composition of the outer kinetochore NDC80 complex, a key part of anaphase, the spindle elongates and the sister chromatids separate, the mitotic apparatus that attaches the centromere of chromosomes to resulting in segregation of the two genomes during telophase.