Week 33, 12-18 August 2018 CDTR
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wnv-Case-Definition.Pdf
Draft Case Definition for West Nile Fever Animal and Plant Health Inspection Service West Nile Fever Veterinary Services October 2018 Case Definition (Notifiable) 1. Clinical Signs 1.1 Clinical Signs: West Nile Fever (WNF) is a zoonotic mosquito-borne viral disease caused by the West Nile virus (WNV), a Flavivirus of the family Flaviviridae. Many vertebrate species are susceptible to natural WNV infection; however, fatal neurological outbreaks have only been documented in equids, humans, geese, wild birds (particularly corvids), squirrels, farmed alligators, and dogs. Birds serve as the natural host reservoir of WNV. The incubation period is estimated to be three to 15 days in horses Ten to 39 percent of unvaccinated horses infected with WNV will develop clinical signs. Most clinically affected horses exhibit neurological signs such as ataxia (including stumbling, staggering, wobbly gait, or incoordination) or at least two of the following: circling, hind limb weakness, recumbency or inability to stand (or both), multiple limb paralysis, muscle fasciculation, proprioceptive deficits, altered mental status, blindness, lip droop/paralysis, teeth grinding. Behavioral changes including somnolence, listlessness, apprehension, or periods of hyperexcitability may occur. Other common clinical signs include colic, lameness, anorexia, and fever. 2. Laboratory criteria: 2.1 Agent isolation and identification: The virus can be identified by polymerase chain reaction (PCR) and virus isolation (VI). Preferred tissues from equids are brain or spinal cord. 2.2 Serology: Antibody titers can be identified in paired serum samples by IgM and IgG capture enzyme linked immunosorbent assay (ELISA), plaque reduction neutralization test (PRNT), and virus neutralization (VN). Only a single serum sample is required for IgM capture ELISA, and this is the preferred serologic test in live animals. -

Rift Valley Fever for Host Innate Immunity in Resistance to a New
A New Mouse Model Reveals a Critical Role for Host Innate Immunity in Resistance to Rift Valley Fever This information is current as Tânia Zaverucha do Valle, Agnès Billecocq, Laurent of September 25, 2021. Guillemot, Rudi Alberts, Céline Gommet, Robert Geffers, Kátia Calabrese, Klaus Schughart, Michèle Bouloy, Xavier Montagutelli and Jean-Jacques Panthier J Immunol 2010; 185:6146-6156; Prepublished online 11 October 2010; Downloaded from doi: 10.4049/jimmunol.1000949 http://www.jimmunol.org/content/185/10/6146 Supplementary http://www.jimmunol.org/content/suppl/2010/10/12/jimmunol.100094 http://www.jimmunol.org/ Material 9.DC1 References This article cites 46 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/185/10/6146.full#ref-list-1 Why The JI? Submit online. by guest on September 25, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American -
West Nile Virus Questions and Answers
West Nile Virus Questions and Answers Q: How do people get infected with West Nile Virus (WNV)? A: The most likely way a human would become infected with WNV is through the bite of an infected mosquito. Some people have also become infected with WNV following receipt of contaminated blood or blood products, or transplanted organs from an infected donor. Mothers who are recently infected with WNV may also transmit the virus to their unborn child, or to their baby while breastfeeding. Q: Who is at risk for getting West Nile encephalitis? A: All residents of areas where WNV activity has been identified are at risk of getting West Nile encephalitis. Q: What is the time from exposure to onset of disease symptoms for West Nile encephalitis in humans? A: Usually 3 to 15 days. Q: What are the symptoms of West Nile virus infection? A: Most people who are infected with WNV will not have any noticeable illness, or have a mild form of illness called West Nile Fever. Persons with West Nile Fever typically experience symptoms of fever, headache, nausea, muscle weakness, and body aches lasting 2 to 6 days or longer. Sensitivity when looking at light and a skin rash appearing on the trunk of the body may also be present. Approximately 20% of persons infected with WNV will develop more severe neurologic disease that may be life-threatening. Adults over the age of 50 years are at greater risk of having serious disease. Potential symptoms of severe infection (West Nile encephalitis or meningitis) include intense headache, dizziness, severe muscle weakness, neck stiffness, vomiting, disorientation, mental confusion, tremors, muscle paralysis, or convulsions and coma. -

West Nile Virus
Oklahoma State Department of Health Acute Disease Service Public Health Fact Sheet West Nile Virus What is West Nile virus? West Nile virus is one of a group of viruses called arboviruses that are spread by mosquitoes and may cause illness in birds, animals, and humans. West Nile virus was not known to be present in the United States until the summer of 1999. Previously, West Nile virus was only found in Africa, western Asia, the Middle East, and Eastern Europe. Where is West Nile virus in the United States? West Nile virus was first identified as a disease threat in the United States during the summer of 1999 and was limited to the northeastern states through 2000. However, the virus rapidly expanded its geographic range. By the end of 2004, West Nile virus had spread from the Atlantic to the Pacific coast with viral activity confirmed in all 48 contiguous states. How is it spread? West Nile virus is primarily spread through the bite of an infected mosquito. Mosquitoes pick up the virus when they feed on infected birds. The virus must then circulate in the mosquito for a few days before they are capable of passing the infection to animals or humans while biting. West Nile virus is not spread person to person through casual contact such as touching or kissing. Rarely, West Nile virus has also been spread through blood transfusions, although blood banks do screen blood supply for the infection. How long does it take to get sick after a bite from an infected mosquito? It takes about three to 15 days for both human and equine (horse, mule, or donkey) illness to occur after a bite from infected mosquito. -

DSHS Arbovirus Activity 061817
Arbovirus Activity in Texas 2017 Surveillance Report June 2018 Texas Department of State Health Services Infectious Disease Control Unit Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California serogroup viruses (CAL), chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2017, reported human arboviral disease cases were attributed to WNV (54%), ZIKV (22%), DENV (17%), and CHIKV (6%) (Table 1). Animal infections or disease caused by CAL, EEEV, SLEV, and WNV were also reported during 2017. Table 1. Year-End Arbovirus Activity Summary, Texas, 2017 California Serogroup Viruses California serogroup viruses (CAL) are bunyaviruses and include California encephalitis virus (CEV), Jamestown Canyon virus, Keystone virus, La Crosse virus (LACV), snowshoe hare virus, and Trivittatus virus. These viruses are maintained in a cycle between mosquito vectors and vertebrate hosts in forest habitats. In the United States (U.S.), approximately 80-100 reported cases of human neuroinvasive disease are caused by LACV each year (CDC), mostly in mid-Atlantic and southeastern states. From 2002-2016, Texas reported a total of 5 cases of human CAL disease (range: 0-3 cases/year): 1 case of CEV neuroinvasive disease and 4 cases of LACV neuroinvasive disease. In 2017, one CEV-positive mosquito pool was identified in Orange County (Figure 1); no human cases of CAL disease were reported. -
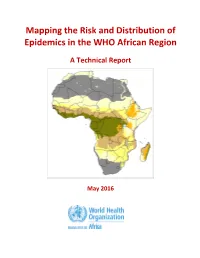
Mapping the Risk and Distribution of Epidemics in the WHO African Region
Mapping the Risk and Distribution of Epidemics in the WHO African Region A Technical Report May 2016 WHO/AFRO Library Cataloguing – in – Publication Data Mapping the Risk and Distribution of Epidemics in the WHO African Region: a technical report 1. Disease Outbreaks – statistics and numerical data 2. Epidemics – statistics and numerical data 3. Communicable Diseases – statistics and numerical data 4. Risk Assessment – supply and distribution – statistics and numerical data 5. Data collection – utilization 6. Africa I. Work Health Organization. Regional Office for Africa II. Title ISBN: 978-9290233084-4 (NLM Classification : WA 105) © WHO Regional Office for Africa, 2016 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. Copies of this publication may be obtained from the Library, WHO Regional Office for Africa, P.O. Box 6, Brazzaville, Republic of Congo (Tel: +47 241 39100; Fax: +47 241 39507; E-mail: [email protected]). Requests for permission to reproduce or translate this publication – whether for sale or for non-commercial distribution – should be sent to the same address. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

West Nile Virus
West Nile Virus Frequently Asked Questions What is West Nile virus? West Nile virus is a viral infection that is spread by the bite of an infected mosquito. Mosquitoes get infected with the West Nile virus by feeding on infected birds. The infected mosquitoes then spread the virus by biting humans and other animals, such as horses. Identified in the United States in 1999, West Nile virus is seen most often during the summer and early fall months. Who gets West Nile virus? Anyone can get infected with the West Nile virus. The virus can affect anyone bitten by an infected mosquito. People over the age of 50 and people with weak immune systems are at greater risk of developing severe illness. How do people get West Nile virus? The virus is spread by the bite of a mosquito infected with the West Nile virus. What are the symptoms of West Nile virus? Many people infected with West Nile virus do not become ill and may not develop symptoms. About 20% of infected people will develop West Nile fever. When symptoms do occur, they may be mild or severe and show up 3 to 15 days after being bitten by an infected mosquito. • Mild symptoms inlcude flu-like illness with fever, headache, body aches, nausea and sometimes swollen lymph glands or a skin rash on the chest, stomach and back. • Severe symptoms include high fever, neck stiffness and swelling of the brain (encephalitis) which can lead to coma, convulsions and death. Less than 1% of infected people will develop severe symptoms. -

Zoonotic Potential of International Trade in CITES-Listed Species Annexes B, C and D JNCC Report No
Zoonotic potential of international trade in CITES-listed species Annexes B, C and D JNCC Report No. 678 Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex C: CITES-listed species and directly associated zoonotic diseases Annex D: Full trade summaries by taxonomic family UNEP-WCMC & JNCC May 2021 © JNCC, Peterborough 2021 Zoonotic potential of international trade in CITES-listed species Prepared for JNCC Published May 2021 Copyright JNCC, Peterborough 2021 Citation UNEP-WCMC and JNCC, 2021. Zoonotic potential of international trade in CITES- listed species. JNCC Report No. 678, JNCC, Peterborough, ISSN 0963-8091. Contributing authors Stafford, C., Pavitt, A., Vitale, J., Blömer, N., McLardy, C., Phillips, K., Scholz, L., Littlewood, A.H.L, Fleming, L.V. & Malsch, K. Acknowledgements We are grateful for the constructive comments and input from Jules McAlpine (JNCC), Becky Austin (JNCC), Neville Ash (UNEP-WCMC) and Doreen Robinson (UNEP). We also thank colleagues from OIE for their expert input and review in relation to the zoonotic disease dataset. Cover Photographs Adobe Stock images ISSN 0963-8091 JNCC Report No. 678: Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex B: Taxonomic orders and associated zoonotic diseases Table B1: Taxonomic orders1 associated with at least one zoonotic disease according to the source papers, ranked by number of associated zoonotic diseases identified. -

West Nile Virus Restriction in Mosquito and Human Cells: a Virus Under Confinement
Review West Nile Virus Restriction in Mosquito and Human Cells: A Virus under Confinement Marie-France Martin and Sébastien Nisole * Viral Trafficking, Restriction and Innate Signaling Team, Institut de Recherche en Infectiologie de Montpellier (IRIM), CNRS, 34090 Montpellier, France; [email protected] * Correspondence: [email protected] Received: 7 May 2020; Accepted: 27 May 2020; Published: 29 May 2020 Abstract: West Nile virus (WNV) is an emerging neurotropic flavivirus that naturally circulates between mosquitoes and birds. However, WNV has a broad host range and can be transmitted from mosquitoes to several mammalian species, including humans, through infected saliva during a blood meal. Although WNV infections are mostly asymptomatic, 20% to 30% of cases are symptomatic and can occasionally lead to severe symptoms, including fatal meningitis or encephalitis. Over the past decades, WNV-carrying mosquitoes have become increasingly widespread across new regions, including North America and Europe, which constitutes a public health concern. Nevertheless, mosquito and human innate immune defenses can detect WNV infection and induce the expression of antiviral effectors, so-called viral restriction factors, to control viral propagation. Conversely, WNV has developed countermeasures to escape these host defenses, thus establishing a constant arms race between the virus and its hosts. Our review intends to cover most of the current knowledge on viral restriction factors as well as WNV evasion strategies in mosquito and human cells in order to bring an updated overview on WNV–host interactions. Keywords: West Nile virus; restriction factors; interferon; innate immunity; mosquito; viral countermeasures; viral evasion 1. Introduction 1.1. West Nile Virus Incidence West Nile virus (WNV) belongs to the Flaviviridae family, from the Flavivirus genus, which also comprises Zika virus (ZIKV), dengue virus (DENV), tick-borne encephalitis virus (TBEV), and yellow fever virus (YFV). -

Find the Right Sample: a Study on the Versatility of Saliva and Urine
Niedrig et al. BMC Infectious Diseases (2018) 18:707 https://doi.org/10.1186/s12879-018-3611-x REVIEW Open Access Find the right sample: A study on the versatility of saliva and urine samples for the diagnosis of emerging viruses Matthias Niedrig1* , Pranav Patel2, Ahmed Abd El Wahed3, Regina Schädler1 and Sergio Yactayo4 Abstract Background: The emergence of different viral infections during the last decades like dengue, West Nile, SARS, chikungunya, MERS-CoV, Ebola, Zika and Yellow Fever raised some questions on quickness and reliability of laboratory diagnostic tests for verification of suspected cases. Since sampling of blood requires medically trained personal and comprises some risks for the patient as well as for the health care personal, the sampling by non- invasive methods (e.g. saliva and/ or urine) might be a very valuable alternative for investigating a diseased patient. Main body: To analyse the usefulness of alternative noninvasive samples for the diagnosis of emerging infectious viral diseases, a literature search was performed on PubMed for alternative sampling for these viral infections. In total, 711 papers of potential relevance were found, of which we have included 128 in this review. Conclusions: Considering the experience using non-invasive sampling for the diagnostic of emerging viral diseases, it seems important to perform an investigation using alternative samples for routine diagnostics. Moreover, during an outbreak situation, evaluation of appropriate sampling and further processing for laboratory analysis on various diagnostic platforms are very crucial. This will help to achieve optimal diagnostic results for a good and reliable case identification. Keywords: Sample type, Emerging diseases, Viruses, Diagnostics Background by PCR or for testing the presence of specific antibodies. -

West Nile Fever in Tunisia 16 14
Weekly Epidemiological Monitor ISSN 2224-4220 Volume 11; Issue no 41; 14 October 2018 West Nile fever cases reported in Tunisia from week 1 to week 40, 2018 Current major event West Nile fever in Tunisia 16 14 As of 8 October 2018, the Ministry of 12 Health of Tunisia reported 177 sus- 10 pected cases of West Nile fever 8 (WNF). Out of these, 22 are probable 6 and 17 are laboratory confirmed cas- 4 Number of suspected cassesuspected of Number es. One death has also been reported 2 in a 27 year male who was hospital- 0 ized for meningo-encephalitis in 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 September 2018. Epidemiological weeks (date of onset of symptoms) Editorial note West Nile fever cases reported from Update on outbreaks in the West Nile Virus (WNV) is a member Tunisia Eastern Mediterranean Region of the flavivirus genus and belongs to Year Cases Deaths MERS in Saudi Arabia; cholera in Somalia; the Japanese encephalitis antigenic 1997 111 8 complex of the family Flaviviridae. cholera in Yemen; Dengue in Yemen. WNV infection is a non-contagious 2003 112 9 Current public health events of disease, primarily transmitted by the 2012 123* 12 international concern bite of infected mosquitoes of the [cumulative No of cases (deaths), CFR %] genus Culex. The infection is often Government has already enhanced asymptomatic (80%) but, when clini- surveillance and standardized case Avian influenza: 2006-2017 cally apparent, symptoms range from management through distribution of an influenza like symptom to more guidelines and protocols in health Egypt (A/H5N1) [359 (122), 34%] severe neurological disorders and care facilities. -

West Nile Virus Infection Lineages by Including Koutango Virus, a Related Virus That America
West Nile Virus Importance West Nile virus (WNV) is a mosquito-borne virus that circulates among birds, Infection but can also affect other species, particularly humans and horses. Many WNV strains are thought to be maintained in Africa; however, migrating birds carry these viruses to other continents each year, and some strains have become established outside West Nile Fever, Africa. At one time, the distribution of WNV was limited to the Eastern Hemisphere, and it was infrequently associated with serious illness. Clinical cases usually occurred West Nile Neuroinvasive Disease, sporadically in humans and horses, or as relatively small epidemics in rural areas. West Nile Disease, Most human infections were asymptomatic, and if symptoms occurred, they were Near Eastern Equine Encephalitis, typically mild and flu-like. Severe illnesses, characterized by neurological signs, Lordige seemed to be uncommon in most outbreaks. Birds appeared to be unaffected throughout the Eastern Hemisphere, possibly because they had become resistant to the virus through repeated exposure. Since the 1990s, this picture has changed, and WNV has emerged as a significant Last Updated: August 2013 human and veterinary pathogen in the Americas, Europe, the Middle East and other areas. Severe outbreaks, with an elevated case fatality rate, were initially reported in Algeria, Romania, Morocco, Tunisia, Italy, Russia and Israel between 1994 and 1999. While approximately 80% of the people infected with these strains were still asymptomatic, 20% had flu-like signs, and a small but significant percentage (<1%) developed neurological disease. One of these virulent viruses entered the U.S. in 1999. Despite control efforts, it became established in much of North America, and spread to Central and South America and the Caribbean.