Charles Edward Schwartz JC Self Research
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CRASH Syndrome: Clinical Spectrum Vance Lemmon0 Guy Van Campa of Corpus Callosum Hypoplasia, Lieve Vitsa Retardation, Adducted Thumbs, Paul Couckea Patrick J
Review 1608178 Eur J Hum Genet 1995;3:273-284 Erik Fransen3' CRASH Syndrome: Clinical Spectrum Vance Lemmon0 Guy Van Campa of Corpus Callosum Hypoplasia, Lieve Vitsa Retardation, Adducted Thumbs, Paul Couckea Patrick J. Willemsa Spastic Paraparesis and a Department of Medical Genetics, Hydrocephalus Due to Mutations in University of Antwerp, Belgium; One Single Gene, L1 b Case Western Reserve University, Cleveland, Ohio, USA Keywords Abstract X-linked disorder LI is a neuronal cell adhesion molecule with important func Mental retardation tions in the development of the nervous system. The gene Hydrocephalus encoding LI is located near the telomere of the long arm of the MASA syndrome X chromosome in Xq28. We review here the evidence that Adducted thumbs several X-linked mental retardation syndromes including X- Corpus callosum agenesis linked hydrocephalus (HSAS), MASA syndrome, X-linked Spastic paraplegia complicated spastic paraparesis (SPI) and X-linked corpus LI callosum agenesis (ACC) are all due to mutations in the LI CRASH gene. The inter- and intrafamilial variability in families with Mutation analysis an LI mutation is very wide, and patients with HSAS, MASA, SPI and ACC can be present within the same family. There fore, we propose here to refer to this clinical syndrome with the acronym CRASH, for Corpus callosum hypoplasia, Retar dation, Adducted thumbs, Spastic paraplegia and Hydroceph alus. Clinical Aspects for Hydrocephalus due to Stenosis of the Aqueduct of Sylvius. This designation was X-Linked Hydrocephalus based upon the presence of aqueductal steno X-linked hydrocephalus (MIM No. sis in many HSAS patients [1]. However, later 307000) was originally described by Bickers studies reported several HSAS patients with and Adams in 1949. -

The Mutability and Repair of DNA
B.Sc (Hons) Microbiology (CBCS Structure) C-7: Molecular Biology Unit 2: Replication of DNA The Mutability and Repair of DNA Dr. Rakesh Kumar Gupta Department of Microbiology Ram Lal Anand College New Delhi - 110021 Reference – Molecular Biology of the Gene (6th Edition) by Watson et. al. Pearson education, Inc Principles of Genetics (8th Edition) by D. Peter Snustad, D. Snustad, Eldon Gardner, and Michael J. Simmons, Wiley publications Replication errors and their repair The Nature of Mutations: • Transitions: A kind of the simplest mutation which is pyrimidine-to-pyrimidine and purine-to- purine substitutions such as T to C and A to G • Transversions: The other kind of mutation which are pyrimidine-to-purine and purine-to- pyrimidine substitutions such as T to A or G and ATransitions to C or T. Transversions 8 types 4 types Synonymous substitution Non synonymous substitution • Point mutations: Mutations that alter a single nucleotide Other kinds of mutations (which cause more drastic changes in DNA): • Insertions • Deletions • Gross rearrangements of Thesechromosome mutations might be caused by insertion by transposon or by aberrant action of cellular recombination processes. Mutation • Substitution, deletion, or insertion of a base pair. • Chromosomal deletion, insertion, or rearrangement. Somatic mutations occur in somatic cells and only affect the individual in which the mutation arises. Germ-line mutations alter gametes and passed to the next generation. Mutations are quantified in two ways: 1. Mutation rate = probability of a particular type of mutation per unit time (or generation). 2. Mutation frequency = number of times a particular mutation occurs in a population of cells or individuals. -

Genetic Causes.Pdf
1 September 2015 Genetic causes of childhood apraxia of speech: Case‐based introduction to DNA, inheritance, and clinical management Beate Peter, Ph.D., CCC‐SLP Assistant Professor Dpt. of Speech & Hearing Science Arizona State University Adjunct Assistant Professor AG Dpt. of Communication Sciences & Disorders ATAGCT Saint Louis University T TAGCT Affiliate Assistant Professor Dpt. of Speech & Hearing Sciences University of Washington 1 Disclosure Statement Disclosure Statement Dr. Peter is co‐editor of a textbook on speech development and disorders (B. Peter & A. MacLeod, Eds., 2013), for which she may receive royalty payments. If she shares information about her ongoing research study, this may result in referrals of potential research participants. She has no financial interest or related personal interest of bias in any organization whose products or services are described, reviewed, evaluated or compared in the presentation. 2 Agenda Topic Concepts Why we should care about genetics. Case 1: A sporadic case of CAS who is missing a • Cell, nucleus, chromosomes, genes gene. Introduction to the language of genetics • From genes to proteins • CAS can result when a piece of DNA is deleted or duplicated Case 2: A multigenerational family with CAS • How the FOXP2 gene was discovered and why research in genetics of speech and language disorders is challenging • Pathways from genes to proteins to brain/muscle to speech disorder Case 3: One family's quest for answers • Interprofessional teams, genetic counselors, medical geneticists, research institutes • Early signs of CAS, parent education, early intervention • What about genetic testing? Q&A 3 “Genetic Causes of CAS: Case-Based Introduction to DNA, Inheritance and Clinical Management,” Presented by: Beate Peter, PhD, CCC-SLP, September 29, 2015, Sponsored by: CASANA 2 Why should you care about genetics? 4 If you are a parent of a child with childhood apraxia of speech … 5 When she was in preschool, He doesn’t have any friends. -

Mutation by Dr. Ty C.M. Hoffman
Mutation by Dr. Ty C.M. Hoffman Slide 1 Transcription features a one-to-one correspondence between DNA nucleotides in the gene and RNA nucleotides in the RNA transcript. However, the four nucleotide types used in RNA are insufficient to individually specify all twenty biological amino acids during translation. Instead, a sequence of three mRNA nucleotides (collectively called a codon) specifies a single amino acid. Since there are three nucleotide positions within a codon, and each position can be occupied by any of four types of nucleotide, there are sixty-four possible codons. This is more than enough to specify the twenty biological amino acids. Slide 2 The genetic code is universal in that all organisms (with very few exceptions) use the same code for specifying amino acids with mRNA codons. The genetic code is redundant in that more than one codon can specify the same amino acid. This is because there are more types of codons than there are types of amino acids used by organisms. The genetic code is not ambiguous, however, because each codon always specifies the same amino acid. Four of the codons serve special functions. One operates as a start codon (signaling initiation of translation), and three codons operate as stop codons (signaling the termination of translation). Slide 3 Mutation is a random change in the DNA sequence of nucleotides. Mutation can be purely accidental (by a mistake made during DNA replication), or mutation can result from exposure of DNA to a mutagen (something that causes mutation). Mutations can be classified into two major types: • Base-pair substitutions do not change the number of nucleotides in the DNA, because one base pair is substituted for another. -

Advances in Understanding the Genetics of Syndromes Involving Congenital Upper Limb Anomalies
Review Article Page 1 of 10 Advances in understanding the genetics of syndromes involving congenital upper limb anomalies Liying Sun1#, Yingzhao Huang2,3,4#, Sen Zhao2,3,4, Wenyao Zhong1, Mao Lin2,3,4, Yang Guo1, Yuehan Yin1, Nan Wu2,3,4, Zhihong Wu2,3,5, Wen Tian1 1Hand Surgery Department, Beijing Jishuitan Hospital, Beijing 100035, China; 2Beijing Key Laboratory for Genetic Research of Skeletal Deformity, Beijing 100730, China; 3Medical Research Center of Orthopedics, Chinese Academy of Medical Sciences, Beijing 100730, China; 4Department of Orthopedic Surgery, 5Department of Central Laboratory, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing 100730, China Contributions: (I) Conception and design: W Tian, N Wu, Z Wu, S Zhong; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: Y Huang; (V) Data analysis and interpretation: L Sun; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Wen Tian. Hand Surgery Department, Beijing Jishuitan Hospital, Beijing 100035, China. Email: [email protected]. Abstract: Congenital upper limb anomalies (CULA) are a common birth defect and a significant portion of complicated syndromic anomalies have upper limb involvement. Mostly the mortality of babies with CULA can be attributed to associated anomalies. The cause of the majority of syndromic CULA was unknown until recently. Advances in genetic and genomic technologies have unraveled the genetic basis of many syndromes- associated CULA, while at the same time highlighting the extreme heterogeneity in CULA genetics. Discoveries regarding biological pathways and syndromic CULA provide insights into the limb development and bring a better understanding of the pathogenesis of CULA. -

Hereditary Spastic Paraparesis: a Review of New Developments
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.69.2.150 on 1 August 2000. Downloaded from 150 J Neurol Neurosurg Psychiatry 2000;69:150–160 REVIEW Hereditary spastic paraparesis: a review of new developments CJ McDermott, K White, K Bushby, PJ Shaw Hereditary spastic paraparesis (HSP) or the reditary spastic paraparesis will no doubt Strümpell-Lorrain syndrome is the name given provide a more useful and relevant classifi- to a heterogeneous group of inherited disorders cation. in which the main clinical feature is progressive lower limb spasticity. Before the advent of Epidemiology molecular genetic studies into these disorders, The prevalence of HSP varies in diVerent several classifications had been proposed, studies. Such variation is probably due to a based on the mode of inheritance, the age of combination of diVering diagnostic criteria, onset of symptoms, and the presence or other- variable epidemiological methodology, and wise of additional clinical features. Families geographical factors. Some studies in which with autosomal dominant, autosomal recessive, similar criteria and methods were employed and X-linked inheritance have been described. found the prevalance of HSP/100 000 to be 2.7 in Molise Italy, 4.3 in Valle d’Aosta Italy, and 10–12 Historical aspects 2.0 in Portugal. These studies employed the In 1880 Strümpell published what is consid- diagnostic criteria suggested by Harding and ered to be the first clear description of HSP.He utilised all health institutions and various reported a family in which two brothers were health care professionals in ascertaining cases aVected by spastic paraplegia. The father was from the specific region. -

Bio 102 Practice Problems Genetic Code and Mutation
Bio 102 Practice Problems Genetic Code and Mutation Multiple choice: Unless otherwise directed, circle the one best answer: 1. Choose the one best answer: Beadle and Tatum mutagenized Neurospora to find strains that required arginine to live. Based on the classification of their mutants, they concluded that: A. one gene corresponds to one protein. B. DNA is the genetic material. C. "inborn errors of metabolism" were responsible for many diseases. D. DNA replication is semi-conservative. E. protein cannot be the genetic material. 2. Choose the one best answer. Which one of the following is NOT part of the definition of a gene? A. A physical unit of heredity B. Encodes a protein C. Segement of a chromosome D. Responsible for an inherited characteristic E. May be linked to other genes 3. A mutation converts an AGA codon to a TGA codon (in DNA). This mutation is a: A. Termination mutation B. Missense mutation C. Frameshift mutation D. Nonsense mutation E. Non-coding mutation 4. Beadle and Tatum performed a series of complex experiments that led to the idea that one gene encodes one enzyme. Which one of the following statements does not describe their experiments? A. They deduced the metabolic pathway for the synthesis of an amino acid. B. Many different auxotrophic mutants of Neurospora were isolated. C. Cells unable to make arginine cannot survive on minimal media. D. Some mutant cells could survive on minimal media if they were provided with citrulline or ornithine. E. Homogentisic acid accumulates and is excreted in the urine of diseased individuals. 5. -

MASA Syndrome in Twin Brothers: Case Report of Sixteen-Year Clinical Follow Up
Paediatr Croat. 2014;58:286-90 PRIKAZ BOLESNIKA / CASE REPORT www.paedcro.com http://dx.doi.org/10.13112/PC.2014.50 MASA syndrome in twin brothers: case report of sixteen-year clinical follow up Matilda Kovač Šižgorić1, Zlatko Sabol1, Filip Sabol2, Tonći Grmoja3, Svjetlana Bela Klancir1, Zdravka Gjergja1, Ljiljana Kipke Sabol1 MASA syndrome (OMIM 303350) is a rare X-linked recessive neurologic disorder, also called CRASH syndrome, spastic paraplegia 1 and Gareis-Mason syndrome. The acronym MASA describes four major signs: Mental retardation, Aphasia, Shuffl ing gait and Adducted thumbs. A more suitable name for this syndrome is L1 syndrome because the disorder has been associated with mutations in the neuronal cell adhesion molecule L1 (L1CAM) gene. The syndrome has severe symptoms in males, while females are carriers because only one X chromosome is aff ected. The aim of this report is to show similarities and diff erences in clinical manifestations between twins with the L1CAM gene mutation and to emphasize the importance of genetic counseling. Our patients were dizygotic twins born prematurely at 35 weeks of gestation. Pregnancy was complicated with early bleeding and gestational diabetes. Immediately after birth, hypertonia of lower extremities was observed in both twins. Sixteen-year clinical follow up showed spastic paraparetic form with shuffl ing gait, clumsiness, delayed speech development, lower intellectual functioning at the level of mild to moderate mental retarda- tion, primary nocturnal enuresis, behavioral and sleep disorder (more pronounced in the second twin). Magnetic resonance imaging of the brain showed complete agenesis of the corpus callosum, complete lack of the anterior commissure, and internal hydrocephalus. -

Level Estimates of Maternal Smoking and Nicotine Replacement Therapy During Pregnancy
Using primary care data to assess population- level estimates of maternal smoking and nicotine replacement therapy during pregnancy Nafeesa Nooruddin Dhalwani BSc MSc Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy November 2014 ABSTRACT Background: Smoking in pregnancy is the most significant preventable cause of poor health outcomes for women and their babies and, therefore, is a major public health concern. In the UK there is a wide range of interventions and support for pregnant women who want to quit. One of these is nicotine replacement therapy (NRT) which has been widely available for retail purchase and prescribing to pregnant women since 2005. However, measures of NRT prescribing in pregnant women are scarce. These measures are vital to assess its usefulness in smoking cessation during pregnancy at a population level. Furthermore, evidence of NRT safety in pregnancy for the mother and child’s health so far is nebulous, with existing studies being small or using retrospectively reported exposures. Aims and Objectives: The main aim of this work was to assess population- level estimates of maternal smoking and NRT prescribing in pregnancy and the safety of NRT for both the mother and the child in the UK. Currently, the only population-level data on UK maternal smoking are from repeated cross-sectional surveys or routinely collected maternity data during pregnancy or at delivery. These obtain information at one point in time, and there are no population-level data on NRT use available. As a novel approach, therefore, this thesis used the routinely collected primary care data that are currently available for approximately 6% of the UK population and provide longitudinal/prospectively recorded information throughout pregnancy. -
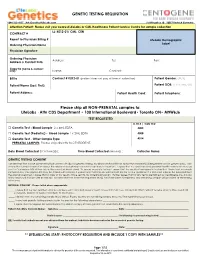
GENETIC TESTING REQUISITION Please Ship All
GENETIC TESTING REQUISITION 1-844-363-4357· [email protected] Schillingallee 68 · 18057 Rostock Germany Attention Patient: Please visit your nearest LifeLabs or CML Healthcare Patient Service Centre for sample collection LL: K012-01/ CML: CEN CONTRACT # Report to Physician Billing # LifeLabs Demographic Ordering Physician Name Label Physician Signature: Ordering Physician Address: Tel: Fax: Address & Contact Info: Copy to (name & contact info): Name: Contact: Bill to Contract # K012-01 (patient does not pay at time of collection) Patient Gender: (M/F) Patient Name (Last, First): Patient DOB: (YYYY/MM/DD) Patient Address: Patient Health Card: Patient Telephone: Please ship all NON-PRENATAL samples to: LifeLabs · Attn CDS Department • 100 International Boulevard• Toronto ON• M9W6J6 TEST REQUESTED LL TR # / CML TC# □ Genetic Test - Blood Sample 2 x 4mL EDTA 4005 □ Genetic Test (Pediatric) - Blood Sample 1 x 2mL EDTA 4008 □ Genetic Test - Other Sample Type 4014 PRENATAL SAMPLES: Please ship directly to CENTOGENE. Date Blood Collected (YYYY/MM/DD): ___________ Time Blood Collected (HH:MM)) :________ Collector Name: ___________________ GENETIC TESTING CONSENT I understand that a DNA specimen will be sent to LifeLabs for genetic testing. My physician has told me about the condition(s) being tested and its genetic basis. I am aware that correct information about the relationships between my family members is important. I agree that my specimen and personal health information may be sent to Centogene AG at their lab in Germany (address below). To ensure accurate testing, I agree that the results of any genetic testing that I have had previously completed by Centogene AG may be shared with LifeLabs. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Clinical and Genetic Characteristics and Prenatal Diagnosis of Patients
Lin et al. Orphanet J Rare Dis (2020) 15:317 https://doi.org/10.1186/s13023-020-01599-y RESEARCH Open Access Clinical and genetic characteristics and prenatal diagnosis of patients presented GDD/ID with rare monogenic causes Liling Lin1, Ying Zhang1, Hong Pan1, Jingmin Wang2, Yu Qi1 and Yinan Ma1* Abstract Background: Global developmental delay/intellectual disability (GDD/ID), used to be named as mental retardation (MR), is one of the most common phenotypes in neurogenetic diseases. In this study, we described the diagnostic courses, clinical and genetic characteristics and prenatal diagnosis of a cohort with patients presented GDD/ID with monogenic causes, from the perspective of a tertiary genetic counseling and prenatal diagnostic center. Method: We retrospectively analyzed the diagnostic courses, clinical characteristics, and genetic spectrum of patients presented GDD/ID with rare monogenic causes. We also conducted a follow-up study on prenatal diagnosis in these families. Pathogenicity of variants was interpreted by molecular geneticists and clinicians according to the guidelines of the American College of Medical Genetics and Genomics (ACMG). Results: Among 81 patients with GDD/ID caused by rare monogenic variants it often took 0.5–4.5 years and 2–8 referrals to obtain genetic diagnoses. Devlopmental delay typically occurred before 3 years of age, and patients usu- ally presented severe to profound GDD/ID. The most common co-existing conditions were epilepsy (58%), micro- cephaly (21%) and facial anomalies (17%). In total, 111 pathogenic variants were found in 62 diferent genes among the 81 pedigrees, and 56 variants were novel. The most common inheritance patterns in this outbred Chinese popula- tion were autosomal dominant (AD; 47%), following autosomal recessive (AR; 37%), and X-linked (XL; 16%).