ASM 2016 Tox Mimics in the Critically Ill Patient Information on Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Propionic Acid on Fatty Acid Oxidation and U Reagenesis
Pediat. Res. 10: 683- 686 (1976) Fatty degeneration propionic acid hyperammonemia propionic acidemia liver ureagenesls Effect of Propionic Acid on Fatty Acid Oxidation and U reagenesis ALLEN M. GLASGOW(23) AND H. PET ER C HASE UniversilY of Colorado Medical Celller, B. F. SlOlillsky LaboralOries , Denver, Colorado, USA Extract phosphate-buffered salin e, harvested with a brief treatment wi th tryps in- EDTA, washed twice with ph os ph ate-buffered saline, and Propionic acid significantly inhibited "CO z production from then suspended in ph os ph ate-buffe red saline (145 m M N a, 4.15 [I-"ejpalmitate at a concentration of 10 11 M in control fibroblasts m M K, 140 m M c/, 9.36 m M PO" pH 7.4) . I n mos t cases the cells and 100 11M in methyl malonic fibroblasts. This inhibition was we re incubated in 3 ml phosph ate-bu ffered sa lin e cont aining 0.5 similar to that produced by 4-pentenoic acid. Methylmalonic acid I1Ci ll-I4Cj palm it ate (19), final concentration approximately 3 11M also inhibited ' 'C0 2 production from [V 'ejpalmitate, but only at a added in 10 II I hexane. Increasing the amount of hexane to 100 II I concentration of I mM in control cells and 5 mM in methyl malonic did not impair palmit ate ox id ation. In two experiments (Fig. 3) the cells. fibroblasts were in cub ated in 3 ml calcium-free Krebs-Ringer Propionic acid (5 mM) also inhibited ureagenesis in rat liver phosphate buffer (2) co nt ain in g 5 g/ 100 ml essent iall y fatty ac id slices when ammonia was the substrate but not with aspartate and free bovine se rum albumin (20), I mM pa lm itate, and the same citrulline as substrates. -
On the Protective Effect of Omega-3 Against Propionic Acid-Induced Neurotoxicity in Rat Pups Afaf K El-Ansary*, Sooad K Al-Daihan and Amina R El-Gezeery
El-Ansary et al. Lipids in Health and Disease 2011, 10:142 http://www.lipidworld.com/content/10/1/142 RESEARCH Open Access On the protective effect of omega-3 against propionic acid-induced neurotoxicity in rat pups Afaf K El-Ansary*, Sooad K Al-Daihan and Amina R El-Gezeery Abstract Backgrounds: The investigation of the environmental contribution for developmental neurotoxicity is very important. Many environmental chemical exposures are now thought to contribute to the development of neurological disorders, especially in children. Results from animal studies may guide investigations of human populations toward identifying environmental contaminants and drugs that produce or protect from neurotoxicity and may help in the treatment of neurodevelopmental disorders. Objective: To study the protective effects of omega-3 polyunsaturated fatty acid on brain intoxication induced by propionic acid (PPA) in rats. Methods: 24 young male Western Albino rats were enrolled in the present study. They were grouped into three equal groups; oral buffered PPA-treated group given a nuerotoxic dose of 250 mg/Kg body weight/day for 3 days; omega-3 - protected group given a dose of 100 mg/kg body weight/day omega-3 orally daily for 5 days followed by PPA for 3 days, and a third group as control given only phosphate buffered saline. Tumor necrosis factor-a, caspase-3, interlukin-6, gamma amino-buteric acid (GABA), serotonin, dopamine and phospholipids were then assayed in the rats brain’s tissue of different groups. Results: The obtained data showed that PPA caused multiple signs of brain toxicity as measured by depletion of gamaaminobyteric acid (GABA), serotonin (5HT) and dopamine (DA) as three important neurotransmitters that reflect brain function. -

Methods of Extraction, Refining and Concentration of Fish Oil As a Source of Omega-3 Fatty Acids
Corpoica Cienc Tecnol Agropecuaria, Mosquera (Colombia), 19(3):645-668 september - december / 2018 ISSN 0122-8706 ISSNe 2500-5308 645 Transformation and agro-industry Review article Methods of extraction, refining and concentration of fish oil as a source of omega-3 fatty acids Métodos de extracción, refinación y concentración de aceite de pescado como fuente de ácidos grasos omega 3 Jeimmy Rocío Bonilla-Méndez,1* José Luis Hoyos-Concha2 1 Researcher, Universidad del Cauca, Facultad de Ciencias Agrarias. Popayán, Colombia. Email: [email protected]. orcid.org/0000-0001-5362-5950 2 Lecturer, Universidad del Cauca, Facultad de Ciencias Agrarias. Popayán, Colombia. Email: [email protected]. orcid.org/0000-0001-9025-9734 Editor temático: Miguel Ángel Rincón Cervera (Instituto de Nutrición y Tecnología de los Alimentos [INTA]) Date of receipt: 05/07/2017 Date of approval: 15/03/2018 How to cite this article: Bonilla-Méndez, J. R., & Hoyos-Concha, J. L. (2018). Methods of extraction, refining and concentration of fish oil as a source of omega-3 fatty acids. Corpoica Ciencia y Tecnología Agropecuaria, 19(3), 645-668. DOI: https://doi.org/10.21930/rcta.vol19_num2_art:684 This license allows distributing, remixing, retouching, and creating from the work in a non-commercial manner, as long as credit is given and their new creations are licensed under the same conditions. * Corresponding author. Universidad del Cauca, Facultad de Ciencias Agrarias. Vereda Las Guacas, Popayán, Colombia. 2018 Corporación Colombiana de Investigación Agropecuaria Corpoica Cienc Tecnol Agropecuaria, Mosquera (Colombia), 19(3):645-668 september - december / 2018 ISSN 0122-8706 ISSNe 2500-5308 Abstract Fish oil is an industrial product of high nutritional methods, there are new technologies with potential value because of its Omega-3 polyunsaturated fatty to be applied on fish oil. -

Formic Acid Acetic Acid Propionic Acid Butyric Acid Valeric Acid Caproic
Organic Acids: Formic acid Citric acid Acetic acid Malic acid Propionic acid Benzoic acid Butyric acid Tartaric acid Valeric acid Caproic acid Oxalic acid Lactic acid Organic Bases: Pyridine Imidazole (solid) Benzimidazole Aniline TEA (tri-ethyl amine) Histidine Nitroaniline Imidazole (dissolved) Amino bases/ Nucleotides ממסים אורגניים (מכילים קשר פחמן-מימן): :(Organic Solvents (contains carbon-hydrogen bond Xylene DMF Hexane Parafine oil Ethylacetate Formamide IPA Piperidine Trizol/Trireagent Butanol SDS (solid) Acetone PMSF (Phenylmethanesulfonyl fluoride) Methanol Tween PFA RNA / DNA (kit parts that contains thioisocyanate) Toluene BME (beta mercaptoethanol) DMSO Ethylenglycol Ethanol Halogenated Organic Solvents (contains F, Cl, Br, I): ממסים אורגניים הלוגניים (מכילים F, Cl, Br, I) Chloroform (CHCl3) Methylene chloride Vinyl chloride Tetrafluoroethylene (CF2 =CF2) Trichloroethylene (CHCl=CCl2) Bromoethane Tert-Butyl bromide חומרים אנאורגניים (חומרים שהם לא חומצה/בסיס אנאורגני) Inorganic Materials (are not inorganic acid/base) LiCl Salts (such as MgCl2, CaCl) Hydrogen peroxide (H2O2) Metals (Cu, Pb, Na etc.) Ammonium thiocyanate (NH4SCN) Sodium Azide (NaN3) Ammonium azide (NH4N3) בסיסים אנאורגניים :Inorganic Bases NH3 NaOH NH4OH Ba(OH)2 NaOH (dissolved) Ca(OH)2 KOH (dissolved) CaCO3 KOH חומצות אנאורגניות: :Inorganic Acids Boric acid (H3BO3) Hydrochloric acid (HCl) Hydrofluoric acid (HF) Nitric acid (HNO3) Hydrobromic acid (HBr) Phosphoric acid (H3PO4) Perchloric acid (HClO4) Sulfuric acid (H2SO4) Hydroiodic acid (HI) Cytotoxic materials: -
Pervaporation Study of Propionic Acid with Ethanol Using Heterogeneous Catalyst in Integrated Esterification- Pervaporation System
International Journal of ChemTech Research CODEN (USA): IJCRGG, ISSN: 0974-4290, ISSN(Online):2455-9555 Vol.10 No.1 pp 148-162, 2017 Pervaporation study of Propionic Acid with Ethanol using heterogeneous catalyst in integrated Esterification- Pervaporation system AnuragTiwari*1, AmitKeshav1, ShubhankarBhowmick2 1Department of Chemical Engineering, National Institute of Technology, Raipur (C.G.) India. 2Department of Mechanical Engineering, National Institute of Technology, Raipur (C.G.) India. Abstract : Pervaporation can be used to enhance the yield of esterification reactions via selective removal of water from the product mixture. Esterification of propionic acid with ethanol over the ion exchange resin, Dowex 50Wx8-400 and sulfuric acid with and without pervaporation has been studied. Various parameters such as, catalyst loading (0.05 to 0.25 mL using H2SO4 and 7.11 to 27.11 g using Dowex 50 Wx8-400), effect of molar ratio (1:1 to 1:2.5), and temperature (40 to 70oC) were analyzed. The change in standard enthalpy and entropy of the reaction under same condition were estimated to be 36.07 kJ mol-1 and 127.53 J mol-1 K-1. Characterization analysis of ion exchange resin was performed using scanning electron microscope (SEM-EDEX) and X-ray differaction (XRD).Using pervaporation-assisted esterification 68% enhancement in the conversion of ethyl propionate was achieved. Keywords : Dowex 50Wx8-400, pervaporation, batch esterification, propionic acid, ethanol. Introduction Process intensification involves imperatives like make it small, combine and use of alternative driving forces. Pervaporation used as the emerging separation techniques based on the principles of process intensification. Phase change through membrane is employed for separation of components present in low concentration in the feed streams. -

Effects of Free Fatty Acids on Propionic Acid Bacteria P Boyaval, C Corre, C Dupuis, E Roussel
Effects of free fatty acids on propionic acid bacteria P Boyaval, C Corre, C Dupuis, E Roussel To cite this version: P Boyaval, C Corre, C Dupuis, E Roussel. Effects of free fatty acids on propionic acid bacteria. Le Lait, INRA Editions, 1995, 75 (1), pp.17-29. hal-00929416 HAL Id: hal-00929416 https://hal.archives-ouvertes.fr/hal-00929416 Submitted on 1 Jan 1995 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Lait (1995) 75, 17-29 17 © Elsevier/INRA Original article Effects of free fatty.acids on propionic acid bacteria P Boyaval 1, C Corre 1, C Dupuis 1, E Roussel 2 1 Laboratoire de Recherches de Technologie Laitière, INRA, 65, rue de St Brieuc, 35042 Rennes Cedex; 2 Standa-Industrie, 184, rue Maréchal-Galliéni, 14050 Caen, France (Received 10 May 1994; accepted 21 November 1994) Summary - The seasonal variations in milk fat composition, especially du ring the grazing period, often lead to poor eye formation in Swiss-type cheese. The influence of free fatty acids on the grow1h and metabolism of the dairy propionibacteria has been studied in this work. Linoleic (C1B:2), laurie (C12:0), myristic (C14:0) and oleic acids (C1B:1) inhibited the growth and acid production of P treudenreichii subsp shermanii in the reference medium. -

Utilization of Volatile Fatty Acids from Microalgae for the Production of High Added Value Compounds
fermentation Review Utilization of Volatile Fatty Acids from Microalgae for the Production of High Added Value Compounds Angelina Chalima 1, Laura Oliver 2, Laura Fernández de Castro 2, Anthi Karnaouri 1, Thomas Dietrich 2 and Evangelos Topakas 1,3,* ID 1 IndBioCat group, Biotechnology Laboratory, School of Chemical Engineering, National Technical University of Athens, 5 Iroon Polytechniou Str., Zografou Campus,15780 Athens, Greece; [email protected] (A.C.); [email protected] (A.K.) 2 Food & Health Group, Health Division, Tecnalia Research & Innovation, Parque Tecnológico de Álava, Leonardo Da Vinci, 11, E-01510 Miñano-Álava, Spain; [email protected] (L.O.); [email protected] (L.F.d.C.); [email protected] (T.D.) 3 Biochemical and Chemical Process Engineering, Division of Sustainable Process Engineering, Department of Civil Environmental and Natural Resources Engineering, Luleå University of Technology, SE-97187 Luleå, Sweden * Correspondence: [email protected]; Tel.: +30-210-772-3264 Received: 9 September 2017; Accepted: 9 October 2017; Published: 15 October 2017 Abstract: Volatile Fatty Acids (VFA) are small organic compounds that have attracted much attention lately, due to their use as a carbon source for microorganisms involved in the production of bioactive compounds, biodegradable materials and energy. Low cost production of VFA from different types of waste streams can occur via dark fermentation, offering a promising approach for the production of biofuels and biochemicals with simultaneous reduction of waste volume. VFA can be subsequently utilized in fermentation processes and efficiently transformed into bioactive compounds that can be used in the food and nutraceutical industry for the development of functional foods with scientifically sustained claims. -

Evidence of a DHA Signature in the Lipidome and Metabolome of Human Hepatocytes
Article Evidence of a DHA Signature in the Lipidome and Metabolome of Human Hepatocytes Veronica Ghini 1, Mattia Di Nunzio 2, Leonardo Tenori 3, Veronica Valli 4, Francesca Danesi 4, Francesco Capozzi 2,4, Claudio Luchinat 1,5,6 and Alessandra Bordoni 2,4,* 1 Center of Magnetic Resonance (CERM), University of Florence, Via Luigi Sacconi, 6-50019 Sesto Fiorentino (FI), Italy; [email protected] (V.G.); [email protected] (C.L.) 2 Interdepartmental Centre for Industrial Agri-Food Research, University of Bologna, Via Quinto Bucci, 336-47521 Cesena (FC), Italy; [email protected] (M.D.N.); [email protected] (F.C.) 3 Department of Experimental and Clinical Medicine, University of Florence, Largo Brambilla, 3-50134 Florence (FI), Italy; [email protected] 4 Department of Agri-Food Sciences and Technologies (DISTAL), University of Bologna, Piazza Goidanich, 60-47521 Cesena (FC), Italy; [email protected] (V.V.); [email protected] (F.D.) 5 Department of Chemistry, University of Florence, Via della Lastruccia, 3-50019 Sesto Fiorentino (FI), Italy 6 GIOTTO Biotech S.r.l., Via Madonna del Piano, 6-50019 Sesto Fiorentino (FI), Italy * Correspondence: [email protected]; Tel.: +39-0547-338955; Fax: +39-0547-382348 Academic Editors: David Arráez-Román and Vito Verardo Received: 7 November 2016; Accepted: 26 January 2017; Published: 8 February 2017 Abstract: Cell supplementation with bioactive molecules often causes a perturbation in the whole intracellular environment. Omics techniques can be applied for the assessment of this perturbation. In this study, the overall effect of docosahexaenoic acid (DHA) supplementation on cultured human hepatocyte lipidome and metabolome has been investigated using nuclear magnetic resonance (NMR) in combination with traditional techniques. -

Hazardous Substance Fact Sheet
Right to Know Hazardous Substance Fact Sheet Common Name: PROPIONIC ACID Synonyms: Ethylformic Acid; Methylacetic Acid CAS Number: 79-09-4 Chemical Name: Propanoic Acid RTK Substance Number: 1599 Date: April 2001 Revision: April 2010 DOT Number: UN 1848 Description and Use EMERGENCY RESPONDERS >>>> SEE LAST PAGE Propionic Acid is a colorless, oily liquid with a strong, Hazard Summary unpleasant odor. It is used as a preservative, fungicide, and Hazard Rating NJDOH NFPA antimicrobial agent. HEALTH - 3 FLAMMABILITY - 2 f ODOR THRESHOLD = 0.026 to 0.17 ppm REACTIVITY - 0 f Odor thresholds vary greatly. Do not rely on odor alone to determine potentially hazardous exposures. CORROSIVE COMBUSTIBLE POISONOUS GASES ARE PRODUCED IN FIRE Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; Reasons for Citation 4=severe f Propionic Acid is on the Right to Know Hazardous f Propionic Acid can affect you when inhaled and by passing Substance List because it is cited by ACGIH, DOT, NIOSH, through the skin. NFPA and EPA. f Propionic Acid is a CORROSIVE CHEMICAL and contact f This chemical is on the Special Health Hazard Substance can severely irritate and burn the skin and eyes with possible List. eye damage. f Inhaling Propionic Acid can irritate the nose, throat and lungs causing coughing, wheezing and/or shortness of breath. f Propionic Acid can cause headache, nausea, vomiting, diarrhea and abdominal pain. SEE GLOSSARY ON PAGE 5. FIRST AID Workplace Exposure Limits Eye Contact f Immediately flush with large amounts of water for at least 30 NIOSH: The recommended airborne exposure limit (REL) is minutes, lifting upper and lower lids. -

Bioactive Lipids and Their Derivatives in Biomedical Applications
Review Biomol Ther 29(5), 465-482 (2021) Bioactive Lipids and Their Derivatives in Biomedical Applications Jinwon Park, Jaehyun Choi, Dae-Duk Kim, Seunghee Lee, Bongjin Lee, Yunhee Lee, Sanghee Kim, Sungwon Kwon, Minsoo Noh, Mi-Ock Lee, Quoc-Viet Le* and Yu-Kyoung Oh* College of Pharmacy and Research Institute of Pharmaceutical Sciences, Seoul National University, Seoul 08826, Republic of Korea Abstract Lipids, which along with carbohydrates and proteins are among the most important nutrients for the living organism, have a variety of biological functions that can be applied widely in biomedicine. A fatty acid, the most fundamental biological lipid, may be classi- fied by length of its aliphatic chain, and the short-, medium-, and long-chain fatty acids and each have distinct biological activities with therapeutic relevance. For example, short-chain fatty acids have immune regulatory activities and could be useful against autoimmune disease; medium-chain fatty acids generate ketogenic metabolites and may be used to control seizure; and some metabolites oxidized from long-chain fatty acids could be used to treat metabolic disorders. Glycerolipids play important roles in pathological environments, such as those of cancers or metabolic disorders, and thus are regarded as a potential therapeutic tar- get. Phospholipids represent the main building unit of the plasma membrane of cells, and play key roles in cellular signaling. Due to their physical properties, glycerophospholipids are frequently used as pharmaceutical ingredients, in addition to being potential novel drug targets for treating disease. Sphingolipids, which comprise another component of the plasma membrane, have their own distinct biological functions and have been investigated in nanotechnological applications such as drug delivery systems. -
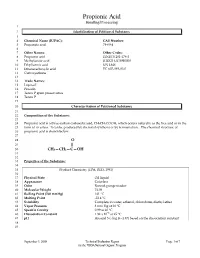
Propionic Acid
Propionic Acid Handling/Processing 1 2 Identification of Petitioned Substance 3 4 Chemical Name (IUPAC): CAS Number: 5 Propanoic acid 79-09-4 6 7 Other Names: Other Codes: 8 Propionic acid EINECS 201-176-3 9 Methylacetic acid RTECS UE 5950000 10 Ethylformic acid UN 1848 11 Ethanecarboxylic acid EC 607-089-00-0 12 Carboxyethane 13 14 Trade Names: 15 Luprosil 16 Prozoin 17 Tenox P grain preservative 18 Tenox P 19 20 Characterization of Petitioned Substance 21 22 Composition of the Substance: 23 24 Propionic acid is a three-carbon carboxylic acid, CH3CH2COOH, which occurs naturally as the free acid or in the 25 form of its esters. It can be produced by chemical synthesis or by fermentation. The chemical structure of 26 propionic acid is shown below: 27 28 O 29 || 30 CH3—CH2—C—OH 31 32 33 Properties of the Substance: 34 35 Product Chemistry (EPA, RED, 1991) 36 37 Physical State Oil liquid 38 Appearance Colorless 39 Odor Rancid, pungent odor 40 Molecular Weight 74.08 41 Boiling Point (760 mmHg) 141 ºC 42 Melting Point -22.4 ºC 43 Solubility Complete in water, ethanol, chloroform, diethyl ether 44 Vapor Pressure 3 mm Hg at 20 ºC 45 Specific Gravity 0.99 at 20 ºC 46 Dissociation Constant 1.32 x 10–5 at 25 ºC 47 pH Around 5 (- log K=4.87) based on the dissociation constant 48 49 September 3, 2008 Technical Evaluation Report Page 1 of 7 for the USDA National Organic Program Technical Evaluation Report Propionic Acid Handling/Processing 50 Specific Uses of the Substance: 51 52 Propionic acid is an active ingredient for use as fungicides and bactericides on stored grains, hay, storage 53 areas for silage and grains, poultry litter, and drinking water for poultry and livestock. -

Co-Administration of Propionate Or Protocatechuic Acid Does Not Affect
nutrients Article Co-Administration of Propionate or Protocatechuic Acid Does Not Affect DHA-Specific Transcriptional Effects on Lipid Metabolism in Cultured Hepatic Cells Francesca Danesi 1,2 , Bjørk D. Larsen 3, Mattia Di Nunzio 1,2, Ronni Nielsen 3, 4 1, 3 1,2, Dario de Biase , Veronica Valli y, Susanne Mandrup and Alessandra Bordoni * 1 Department of Agricultural and Food Sciences (DISTAL), University of Bologna, 47521 Cesena, Italy; [email protected] (F.D.); [email protected] (M.D.N.); [email protected] (V.V.) 2 Interdepartmental Center for Agri-food Industrial Research (CIRI Agrifood), University of Bologna, 47521 Cesena, Italy 3 Department of Biochemistry and Molecular Biology, University of Southern Denmark, Syddansk Universitet, 5230 Odense M, Denmark; [email protected] (B.D.L.); [email protected] (R.N.); [email protected] (S.M.) 4 Department of Pharmacy and Biotechnology (FABIT), University of Bologna, 40138 Bologna, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-0547-338955 Current address: Sociedad Española de Colorantes Naturales y Afines (SECNA), El Muladar, Chiva, y 46370 Valencia, Spain. Received: 10 August 2020; Accepted: 24 September 2020; Published: 26 September 2020 Abstract: Long-chain n-3 polyunsaturated fatty acids (n-3 LC-PUFAs) are collectively recognized triglyceride-lowering agents, and their preventive action is likely mediated by changes in gene expression. However, as most studies employ fish oil, which contains a mixture of n-3 LC-PUFAs, the docosahexaenoic acid (DHA)-specific transcriptional effects on lipid metabolism are still unclear. The aim of the present study was to further elucidate the DHA-induced transcriptional effects on lipid metabolism in the liver, and to investigate the effects of co-administration with other bioactive compounds having effects on lipid metabolism.