Final Comments on Hras Pdf Icon[PDF, 3.5MB]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Killer UX Design Preface
Killer UX Design About Jodie Moule Jodie Moule is co-founder and director of Symplicit, an experience design consultancy based in Australia that focuses on research, strategy, and design services. With a background in psychology, her understanding of human behavior is central to helping businesses see their brands through the eyes of customers, influencing the way they approach the design of their products, systems, and processes. About SitePoint SitePoint specializes in publishing practical, rewarding, and approachable content for web professionals. Visit http://www.sitepoint.com/ to access our books, blogs, newsletters, videos, and community forums. Preface When I embarked on my career as a psychologist, I never imagined I’d end up designing technology products and services. Funny where you end up in life, and lucky for me all those years at university weren’t wasted: the business of understanding humans and the way they behave is critical to designing. With the digital and physical worlds merging more than ever before, it is vital to understand how technology can enhance the human experience, and not cause frustration or angst at every touchpoint. To create technology that seamlessly fits into our daily lives, there’s a simple formula. First, consider the person attached to your technology solution and the context in which they’ll be using your creation; then, design your solution and involve users in the process to refine your thinking. Today, technology is used to change attitudes and behavior, creating amazing challenges for designers. And if we want to create products and services that have the power to educate people so that they may live better lives, or help to reduce the time people take to do certain tasks—or even attract them to our products instead of our competitors—we need to first understand what makes them tick. -

Upcoming Album by the Cousins, Including a March 17Th Release and Full Track Listing
I’m having a rather ‘One and Only’ Valentine’s Day evening as I write this editorial but at least I had Jim and Kevin bring me a little ‘Sunshine’ fresh from the studio earlier; new tunes beat roses any day. The serpentine return of The Cousins from the mists of time has also got me thinking lately about another obscure, old family band who haven’t put out an album since 2004 called the Brothers Creeggan. We can live in hope... - Mil NEWS The Ladies have been in the studio all month working on new music! We’ve seen 14 new songs listed so far. Check ‘Features’ on page 3 for the full details. More dates and three shows with The Persuasions have been announced. More details and dates on pages 2 & 4. New details about Rattlesnake Love, the upcoming album by The Cousins, including a March 17th release and full track listing. All the details below. (Apologies for the incorrect date/single last issue. That was the info we had at the time of publication) BUpcoming The Cousins Are Ready to Rattle! Kevin and real-life cousin Harland Williams are set to release Rattlesnake Love into the world on March 17th. 11 songs have slithered their way out of The Purple Pineapple Studios with a sound described as ‘a mixture of the sensual, the occult, the poppy, the rocky.’ With enough interest the duo might do a live show so hit their site, subscribe to their mailing list and order Rattlesnake Love soon! Full Track List: Meet The Cousins! ♫ You can listen to 01. -

Plans for a Bigger Library Edward Cuddy: by Michelle Murphy the New Library Is to Make It Possible Their Own Requests Without Limitations
December 2003 ____ _ , MARIAN LIBRARY - DgiEMPN COU IND 101: Freshmen Speak Ou INDEX By Emmanuel Onyenyili The main purposes of IND, as After last year, the first year that IND explained by Professor Walsh, one of was featured, several changes were Dreamweaver Portfolio, Time the 17 IND teachers, is to introduce made to IND 101 in an effort to make it Magazine articles, Sam & Tom Disc, students to the college experience by a more informative, and effective Pgi large session lectures, Core competen helping students make the transition course. The amendments made includ cies, sustainability; these are all words into college, to explain to the students ed teaching more classes in small ses IND 101: and phrases that every 2003 incoming the purpose of the core curriculum, sions and limiting the number of large Freshmen Speak freshmen is familiar with. Why such a and to give students a taste of the dif sessions, as opposed to last year, when Out familiarity with these words? The ferent courses in the core curriculum. classes taught in both sessions were answer is simple. These are words that In this course, she says, “you’re equally divided. New Additions have been repeated countless times in exposed to a variety of different fields.” Another change implemented this in Wick the freshmen introductory course, IND Dr. Richard Knaub, the teacher of year was “an emphasis on the course as 101. the IND 101 class, reemphasized this defining individual sustainability, and IND 101 is a refined version of the theme of exposure when he said that making the transition into college,” Plans for A Bigger Liberal Arts Colloquium (LAC). -
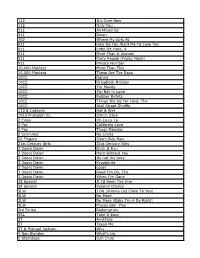
112 It's Over Now 112 Only You 311 All Mixed up 311 Down
112 It's Over Now 112 Only You 311 All Mixed Up 311 Down 702 Where My Girls At 911 How Do You Want Me To Love You 911 Little Bit More, A 911 More Than A Woman 911 Party People (Friday Night) 911 Private Number 10,000 Maniacs More Than This 10,000 Maniacs These Are The Days 10CC Donna 10CC Dreadlock Holiday 10CC I'm Mandy 10CC I'm Not In Love 10CC Rubber Bullets 10CC Things We Do For Love, The 10CC Wall Street Shuffle 112 & Ludacris Hot & Wet 1910 Fruitgum Co. Simon Says 2 Evisa Oh La La La 2 Pac California Love 2 Pac Thugz Mansion 2 Unlimited No Limits 20 Fingers Short Dick Man 21st Century Girls 21st Century Girls 3 Doors Down Duck & Run 3 Doors Down Here Without You 3 Doors Down Its not my time 3 Doors Down Kryptonite 3 Doors Down Loser 3 Doors Down Road I'm On, The 3 Doors Down When I'm Gone 38 Special If I'd Been The One 38 Special Second Chance 3LW I Do (Wanna Get Close To You) 3LW No More 3LW No More (Baby I'm A Do Right) 3LW Playas Gon' Play 3rd Strike Redemption 3SL Take It Easy 3T Anything 3T Tease Me 3T & Michael Jackson Why 4 Non Blondes What's Up 5 Stairsteps Ooh Child 50 Cent Disco Inferno 50 Cent If I Can't 50 Cent In Da Club 50 Cent In Da Club 50 Cent P.I.M.P. (Radio Version) 50 Cent Wanksta 50 Cent & Eminem Patiently Waiting 50 Cent & Nate Dogg 21 Questions 5th Dimension Aquarius_Let the sunshine inB 5th Dimension One less Bell to answer 5th Dimension Stoned Soul Picnic 5th Dimension Up Up & Away 5th Dimension Wedding Blue Bells 5th Dimension, The Last Night I Didn't Get To Sleep At All 69 Boys Tootsie Roll 8 Stops 7 Question -

All About Mentoring
ALL ABOUT MENTORINGA PUBLICATION OF SUNY EMPIRE STATE COLLEGE Issue 44 • Winter 2013 - 2014 ALL ABOUT MENTORING ABOUT ALL Issue 44 • Winter 2013 - 2014 - 2013 1 Union Ave. Saratoga Springs, NY 12866-4391 518-587-2100 www.esc.edu ISSN 2331-5431 Printed by SUNY Empire State College Print Shop ALL ABOUT ALL ABOUT MENTORING Submissions to All About Mentoring ISSUE 44 f you have a scholarly paper-in-progress or a talk that you have presented, All About Mentoring WINTER 2013 - 2014 would welcome it. If you developed materials for your students that may be of good use to others, or have a comment on any part of this issue, or on topics/concerns relevant to our Alan Mandell I mentoring community, please send them along. College Professor of Adult Learning and Mentoring If you have a short story, poem, drawings or photographs, or have reports on your reassignments Editor and sabbaticals, All About Mentoring would like to include them in an upcoming issue. Karen LaBarge Senior Staff Assistant for Send submissions to Alan Mandell (SUNY Empire State College, Metropolitan Center, 325 Hudson Faculty Development St., New York, NY 10013-1005) or via email at [email protected]. “The autocrat wishes docile followers; Associate Editor Submissions to All About Mentoring can be of varied length and take many forms. (Typically, he therefore wishes a type of education to Lorraine Klembczyk Graphic Designer materials are no longer than 7,500 words.) It is easiest if materials are sent via email to Mandell build docility and obedience. Democracy as WORD attachments. -

February 27, 1998 Eastern Illinois University
Eastern Illinois University The Keep February 1998 2-27-1998 Daily Eastern News: February 27, 1998 Eastern Illinois University Follow this and additional works at: http://thekeep.eiu.edu/den_1998_feb Recommended Citation Eastern Illinois University, "Daily Eastern News: February 27, 1998" (1998). February. 8. http://thekeep.eiu.edu/den_1998_feb/8 This is brought to you for free and open access by the 1998 at The Keep. It has been accepted for inclusion in February by an authorized administrator of The Keep. For more information, please contact [email protected]. RAIN Two in a high of 53º The INSIDE a row Daily Men’s track Eastern team looks to repeat as FRIDAY Eastern Illinois University OVC indoor Charleston, Ill. 61920 February 27, 1998 champions Vol. 83, No. 109 Four contestants to compete in 2 sections, 16 pages the 22nd annual Miss Black PAGE EIU pageant News 8A SECTION B “Tell the truth and don’t be afraid” Police fail to cite underage victim By JILL JEDLOWSKI Assoc. news editor One of five Eastern students who were Charleston police attacked Friday morning after leaving Mother’s Bar said he is not of legal drinking age and had to conduct photo been drinking, yet Charleston police officers did not issue him a citation for any underage drinking violations or false identification. lineup of suspects Jason Christeson, a freshman physical education major and Panther wrestler in the By JILL JEDLOWSKI 177-190 weight class, said Tuesday he was one Assoc. news editor of the last two students to leave the bar before he and four other students were attacked. -
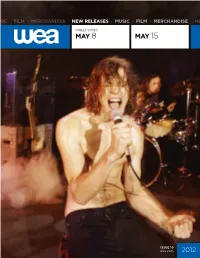
2012 May 8 May 15
NEW RELEASES • MUSIC • FILM • MERCHANDISE • NEW RELEASES • MUSIC • FILM • MERCHANDISE • NEW RELEASES • MUSIC • FILM • MERCHANDISE STREET DATES: MAY 8 MAY 15 ISSUE 10 wea.com 2012 5/8/12 AUDIO & VIDEO RECAP ORDERS ARTIST TITLE LBL CNF UPCSEL # SRP QTY DUE At The Skylines The Secrets To Life RRR CD 016861768720 176872 $9.94 4/18/12 Barenaked Ladies Stop Us If You've Heard This Before! RRW CD 081227975371 528908 $11.98 4/18/12 Donald Fagen The Nightfly WB A 093624952237 530187 $26.98 4/18/12 Group 1 Crew Outta Space Love: Bigger Love Edition FER CD 080688850722 888507 $13.99 4/18/12 Storm Corrosion Storm Corrosion RRR CD 016861764524 176452 $13.99 4/18/12 Storm Corrosion (Special Edition)(CD/Blu- Storm Corrosion RRR MX 016861764555 176455 $24.98 4/11/12 Ray) Tank This Is How I Feel ATL CD 075678825736 528524 $9.94 4/18/12 Tank This Is How I Feel (Amended) ATL CD 075678763144 531301 $9.94 4/18/12 Watkins, Sara Sun Midnight Sun NON CD 075597962048 530684 $16.98 4/18/12 BUMPED TO TBD Various Artists GCB: Music From Season One WNS CD 093624951681 530474 $18.98 Last Update: 03/28/12 For the latest up to date info on this release visit WEA.com. ARTIST: At The Skylines TITLE: The Secrets To Life Label: RRR/Roadrunner Records Config & Selection #: CD 176872 Street Date: 05/08/12 Order Due Date: 04/18/12 UPC: 016861768720 Box Count: 30 WEBSITES: Unit Per Set: 1 Facebook SRP: $9.94 Twitter Alphabetize Under: A Youtube File Under: At The Skylines VIDEOS TRACKS It's Cherried Compact Disc 1 01 Hush 06 Turbulence 02 It's Cherried 07 Chapter 7 03 Shady Dreamin' (Tension) 08 The Amazing Atom 04 143 Princess 09 Clear Eyes, Full Hearts 05 Let's Burn This 10 Forgiveness (Release) FEATURED TRACKS Shady Dreamin' (Tension) Turbulence ALBUM FACTS Genre: Rock Producers: Fredrik Nordström Radio Formats: Metal Radio Focus Markets: Hometown: Huntington Beach and LA market; Tour markets: Atlanta, GA Boston, MA Poughkeepsie, NY Philadelphia, PA New York, NY Buffalo, NY Pontiac, MI Chicago, IL St. -

Episode Descriptions Do
ACTIVITIES EPISODE DESCRIPTIONS DO READ CHILDREN’S PROGRAMMING STORYBOOKS READY TO LEARN TV THAT TEACHES JUNE 2005 VIEW WEDNESDAY, JUNE 1 6:30 AM BARNEY & FRIENDS (802) On Again, Off Again Barney, Baby Bop and the kids learn all about "on" and "off" by playing games together. 7:00 AM SESAME STREET (4050) Zoe's Tutu Gets Stuck in a Tree Zoe tutu gets blown away and ends up stuck in a tree. Telly and Zoe work hard, trying many different strategies in order to get it down. Telly keeps helping Zoe as they try to climb, jump, and boost each other up, and reach the tutu with a stick. Super Grover tries to help and, of course, ends up stuck in the tree with the tutu. Alan comes by and Zoe and Telly explain their problem. Alan suggests getting a ladder from Hooper's store. Just then, Big Bird comes by and Telly has an idea, a big, tall idea! Big Bird is very tall so he should be able to reach the tutu. Big Bird stands on his tippy toes and is able to reach the tutu. The problem is solved! 8:00 AM CYBERCHASE (114) Cool It Determined to destroy Motherboard in any way possible, Hacker cleverly clogs up her cooling system. Digit brings the kids into cyberspace to help fix her, but the special coolant Motherboard needs, cryoxide, is found only in Castleblanca - and the supply is closely monitored! To bring back exactly enough cryoxide for Motherboard, the kids have to figure out the exact volume of Motherboard's tank. -

Anders Åstrand: a Paragon of the Modern Musical Aesthetic
University of Kentucky UKnowledge Theses and Dissertations--Music Music 2017 Anders Åstrand: A Paragon of the Modern Musical Aesthetic Matthew Geiger University of Kentucky, [email protected] Digital Object Identifier: https://doi.org/10.13023/ETD.2017.069 Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Geiger, Matthew, "Anders Åstrand: A Paragon of the Modern Musical Aesthetic" (2017). Theses and Dissertations--Music. 81. https://uknowledge.uky.edu/music_etds/81 This Doctoral Dissertation is brought to you for free and open access by the Music at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Music by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained needed written permission statement(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine) which will be submitted to UKnowledge as Additional File. I hereby grant to The University of Kentucky and its agents the irrevocable, non-exclusive, and royalty-free license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. I agree that the document mentioned above may be made available immediately for worldwide access unless an embargo applies. -

Songs by Artist
Songs by Artist Karaoke Collection Title Title Title +44 18 Visions 3 Dog Night When Your Heart Stops Beating Victim 1 1 Block Radius 1910 Fruitgum Co An Old Fashioned Love Song You Got Me Simon Says Black & White 1 Fine Day 1927 Celebrate For The 1st Time Compulsory Hero Easy To Be Hard 1 Flew South If I Could Elis Comin My Kind Of Beautiful Thats When I Think Of You Joy To The World 1 Night Only 1st Class Liar Just For Tonight Beach Baby Mama Told Me Not To Come 1 Republic 2 Evisa Never Been To Spain Mercy Oh La La La Old Fashioned Love Song Say (All I Need) 2 Live Crew Out In The Country Stop & Stare Do Wah Diddy Diddy Pieces Of April 1 True Voice 2 Pac Shambala After Your Gone California Love Sure As Im Sitting Here Sacred Trust Changes The Family Of Man 1 Way Dear Mama The Show Must Go On Cutie Pie How Do You Want It 3 Doors Down 1 Way Ride So Many Tears Away From The Sun Painted Perfect Thugz Mansion Be Like That 10 000 Maniacs Until The End Of Time Behind Those Eyes Because The Night 2 Pac Ft Eminem Citizen Soldier Candy Everybody Wants 1 Day At A Time Duck & Run Like The Weather 2 Pac Ft Eric Will Here By Me More Than This Do For Love Here Without You These Are Days 2 Pac Ft Notorious Big Its Not My Time Trouble Me Runnin Kryptonite 10 Cc 2 Pistols Ft Ray J Let Me Be Myself Donna You Know Me Let Me Go Dreadlock Holiday 2 Pistols Ft T Pain & Tay Dizm Live For Today Good Morning Judge She Got It Loser Im Mandy 2 Play Ft Thomes Jules & Jucxi So I Need You Im Not In Love Careless Whisper The Better Life Rubber Bullets 2 Tons O Fun -

An Original Composition, Galleria Armonica, Theme and Variations For
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School 2007 An original composition, galleria armonica, theme and variations for piano, harpsichord, harp and orchestra and a comparative study between the pedagogical methodologies of Arnold Schoenberg and Nadia Boulanger regarding training the composer Barrett Ashley Johnson Louisiana State University and Agricultural and Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the Music Commons Recommended Citation Johnson, Barrett Ashley, "An original composition, galleria armonica, theme and variations for piano, harpsichord, harp and orchestra and a comparative study between the pedagogical methodologies of Arnold Schoenberg and Nadia Boulanger regarding training the composer" (2007). LSU Doctoral Dissertations. 1833. https://digitalcommons.lsu.edu/gradschool_dissertations/1833 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. AN ORIGINAL COMPOSITION, GALLERIA ARMONICA, THEME AND VARIATIONS FOR PIANO, HARPSICHORD, HARP AND ORCHESTRA AND A COMPARATIVE STUDY BETWEEN THE PEDAGOGICAL METHODOLOGIES OF ARNOLD SCHOENBERG AND NADIA BOULANGER REGARDING TRAINING THE COMPOSER A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and -
Staying Busy Strikes a Chord with Brian Maes
WEDNESDAY, JANUARY 23, 2019 Lynn plants pot shop on Oxford St. By Gayla Cawley ITEM STAFF LYNN — Recreational pot is coming to downtown Lynn. The City Council approved a proposal from Natural Selections to open a pot shop at 193 Oxford St., which would be next door to The Blue Ox, an upscale restau- rant. Natural Selections is the second compa- ny to receive approval from the City Coun- cil to operate a pot shop in Lynn. Apothca opened a medical marijuana facility on the Lynnway in November and plans to open its recreational component at the shop in March. ITEM 2017 FILE PHOTO | PAULA MULLER “We’re very excited about this relation- ship with the city and we’re ready to start building,” said Aidan O’Donovan, owner of Staying busy strikes Natural Selections, following the vote on Tuesday night. “We’re excited to be here.” Ward 4 Councilor Richard Colucci was the lone vote against the proposal. He a chord with Brian Maes said he voted “no” because he’s a member of East Coast International Church and and Ledger, both in Salem, at Rol- Brian Maes, agreed with its pastor, who spoke against the future shop. ly’s Tavern in Lynn, and Four Oaks keyboard, and Pastor Kurt Lange, of East Coast Inter- guitarist Barry Country Club in Dracut. His band national Church, located on the adjacent BY BILL BROTHERTON plays regularly at area clubs and he Goudreau Munroe Street, said downtown Lynn is not has a busy teaching schedule. perform at the right place for recreational pot in the LYNN — Brian Maes is one busy Apparently, that’s not enough.