Investigation of the Impact of Streptococcus Pneumoniae on A549 Pneumocytes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nosocomial Co-Transmission of Avian Influenza A(H7N9)
SYNOPSIS Nosocomial Co-Transmission of Avian Influenza A(H7N9) and A(H1N1)pdm09 Viruses between 2 Patients with Hematologic Disorders Huazhong Chen,1 Shelan Liu,1 Jun Liu,1 Chengliang Chai, Haiyan Mao, Zhao Yu, Yuming Tang, Geqin Zhu, Haixiao X. Chen, Chengchu Zhu, Hui Shao, Shuguang Tan, Qianli Wang, Yuhai Bi, Zhen Zou, Guang Liu, Tao Jin, Chengyu Jiang, George F. Gao, Malik Peiris,2 Hongjie Yu,2 Enfu Chen2 A nosocomial cluster induced by co-infections with avian in- s of January 4, 2016, a novel avian influenza A vi- fluenza A(H7N9) and A(H1N1)pdm09 (pH1N1) viruses oc- Arus, A(H7N9), first identified in China in March curred in 2 patients at a hospital in Zhejiang Province, China, 2013 (1), had caused 676 laboratory-confirmed cases of in January 2014. The index case-patient was a 57-year-old influenza in humans and 275 influenza-associated deaths man with chronic lymphocytic leukemia who had been occu- in mainland China (Chinese Center for Disease Control pationally exposed to poultry. He had co-infection with H7N9 and Prevention, unpub. data). Most H7N9 virus infections and pH1N1 viruses. A 71-year-old man with polycythemia vera who was in the same ward as the index case-patient for have been acquired through exposure to live poultry mar- 6 days acquired infection with H7N9 and pH1N1 viruses. The kets (LPMs) in urban settings (2) and have been sporadic, incubation period for the second case-patient was estimated but a few have occurred in clusters of >2 epidemiologi- to be <4 days. -
![Directors, Supervisors and Parties Involved in the [Redacted]](https://docslib.b-cdn.net/cover/5931/directors-supervisors-and-parties-involved-in-the-redacted-195931.webp)
Directors, Supervisors and Parties Involved in the [Redacted]
THIS DOCUMENT IS IN DRAFT FORM, INCOMPLETE AND SUBJECT TO CHANGE AND THAT THE INFORMATION MUST BE READ IN CONJUNCTION WITH THE SECTION HEADED “WARNING” ON THE COVER OF THIS DOCUMENT DIRECTORS, SUPERVISORS AND PARTIES INVOLVED IN THE [REDACTED] DIRECTORS Name Residential Address Nationality Executive Directors Mr. Yan Chuanhua (顏傳華) 105#, No. 79 South Junyuan Chinese Xijin Yuyuan Jiaojiang District Taizhou, Zhejiang Province PRC Mr. Zhang Junzhou (章君周) Room 2501, Unit 1, Building 6 Chinese Lakeview International Dayang Street Linhai, Zhejiang Province PRC Non-executive Directors Mr. Wang Haiping (王海平) 103#, Building 8 Chinese Jinshuiwan Small Community Jiaojiang District Taizhou, Zhejiang Province PRC Mr. Wang Haibo (王海波) Room 901, Unit 1, Building 8 Chinese Haitang Huayuan Jiaojiang District Taizhou, Zhejiang Province PRC Ms. Fang Ya (方亞) Room 1001, Unit 1, Building 6 Chinese West Street Small Community Xicheng Street Huangyan District Taizhou, Zhejiang Province PRC Mr. Yu Yangbin (余陽斌) Room 301, Unit 2, Building 15 Chinese Wanxiang International Small Community Qianjiang North Road Shanqian Administrative Village Datian Street Linhai, Zhejiang Province PRC –59– THIS DOCUMENT IS IN DRAFT FORM, INCOMPLETE AND SUBJECT TO CHANGE AND THAT THE INFORMATION MUST BE READ IN CONJUNCTION WITH THE SECTION HEADED “WARNING” ON THE COVER OF THIS DOCUMENT DIRECTORS, SUPERVISORS AND PARTIES INVOLVED IN THE [REDACTED] Name Residential Address Nationality Mr. Ye Jianhua (葉建華) Room 2101, Building 1 Chinese Huanghou Road Baiyun Community Gucheng Street Linhai, Zhejiang Province PRC Ms. Huang Yuyan (黃玉燕) Room 303, Unit 2, Building 6 Chinese Xinming Peninsula Small District Jiaojiang Xinjing Community Taizhou, Zhejiang Province PRC Mr. Yang Yide (楊義德) No. -

National Textiles & Garment Quality Supervision Inspection Centre (Zhejiang) Test Report
National Textiles & Garment Quality Supervision Inspection Centre (Zhejiang) Test Report ADDRESS: No.300 XIASHA ROAD HANGZHOU CHINA Tel: (0571) 85122669 NUMBER:YJ202004588E Fax: (0571) 85125121 DATE: 2020-04-08 Postcode: 310018 APPLICANT: Zhejiang TAISILK Fashion Co. Ltd SAMPLE DESCRIPTION: Disposable Protective Mask ADDRESS: 157Yunxi Road,Jiaojiang District,Taizhou City,Zhejiang Province [签章] STANDARD ITEM RESULT RATING (D GRADE) 1. FORMALDEHYDE (INNER LAYER) (GB/T 32610-2016、GB/T 2912.1-2009)(mg/kg) NOT - ≤20 PASS DETECTED 2. pH VALUE (INNER LAYER) (GB/T 32610-2016、GB/T 7573-2009) - 4.0~8.5 6.5 PASS 3. AZO (OUTER LAYER) (GB/T 32610-2016、GB/T 17592-2011) (mg/kg) NOT - FORBIDDEN PASS DETECTED 4. FILTER EFFICIENCY(SALT MEDIUM) (GB/T32610-2016)(%) - ≥90 93.5 PASS 5. PARTICLE PROTECTIVE PERFORMANCE (GB/T32610-2016)(%) - ≥65 65.2 PASS 6. RESPIRATORY RESISTANCE (GB/T32610-2016)(Pa) -INSPIRATORY RESISTANCE ≤175 73 PASS -EXPIRATORY RESISTANCE ≤145 61 PASS Remarks:1.The protection effect grade is not marked on the sample mark, and it is judged according to the lowest standard requirement D grade. 2. The sample is not pretreated and the result is for reference. PREPARED AND CHECKED BY YU JIE PAGE 1 OF 3 National Textiles & Garment Quality Supervision Inspection Centre (Zhejiang) Test Report ADDRESS: No.300 XIASHA ROAD HANGZHOU CHINA Tel: (0571) 85122669 NUMBER:YJ202004588E Fax: (0571) 85125121 DATE: 2020-04-08 Postcode: 310018 ITEM STANDARD RESULT RATING 7.COLOUR FASTNESS TO RUBBING (GB/T 32610-2016、GB/T 3920-2008) (GRADE) - DRY ≥4 4-5 PASS - WET ≥4 4-5 PASS 8.APPEARANCE (GB/T 32610-2016) Meet the The appearance requirements of quality of 10 - PASS GB/T masks conforms 32610-2016standard to the standard 9. -

Shop Direct Factory List Dec 18
Factory Factory Address Country Sector FTE No. workers % Male % Female ESSENTIAL CLOTHING LTD Akulichala, Sakashhor, Maddha Para, Kaliakor, Gazipur, Bangladesh BANGLADESH Garments 669 55% 45% NANTONG AIKE GARMENTS COMPANY LTD Group 14, Huanchi Village, Jiangan Town, Rugao City, Jaingsu Province, China CHINA Garments 159 22% 78% DEEKAY KNITWEARS LTD SF No. 229, Karaipudhur, Arulpuram, Palladam Road, Tirupur, 641605, Tamil Nadu, India INDIA Garments 129 57% 43% HD4U No. 8, Yijiang Road, Lianhang Economic Development Zone, Haining CHINA Home Textiles 98 45% 55% AIRSPRUNG BEDS LTD Canal Road, Canal Road Industrial Estate, Trowbridge, Wiltshire, BA14 8RQ, United Kingdom UK Furniture 398 83% 17% ASIAN LEATHERS LIMITED Asian House, E. M. Bypass, Kasba, Kolkata, 700017, India INDIA Accessories 978 77% 23% AMAN KNITTINGS LIMITED Nazimnagar, Hemayetpur, Savar, Dhaka, Bangladesh BANGLADESH Garments 1708 60% 30% V K FASHION LTD formerly STYLEWISE LTD Unit 5, 99 Bridge Road, Leicester, LE5 3LD, United Kingdom UK Garments 51 43% 57% AMAN GRAPHIC & DESIGN LTD. Najim Nagar, Hemayetpur, Savar, Dhaka, Bangladesh BANGLADESH Garments 3260 40% 60% WENZHOU SUNRISE INDUSTRIAL CO., LTD. Floor 2, 1 Building Qiangqiang Group, Shanghui Industrial Zone, Louqiao Street, Ouhai, Wenzhou, Zhejiang Province, China CHINA Accessories 716 58% 42% AMAZING EXPORTS CORPORATION - UNIT I Sf No. 105, Valayankadu, P. Vadugapal Ayam Post, Dharapuram Road, Palladam, 541664, India INDIA Garments 490 53% 47% ANDRA JEWELS LTD 7 Clive Avenue, Hastings, East Sussex, TN35 5LD, United Kingdom UK Accessories 68 CAVENDISH UPHOLSTERY LIMITED Mayfield Mill, Briercliffe Road, Chorley Lancashire PR6 0DA, United Kingdom UK Furniture 33 66% 34% FUZHOU BEST ART & CRAFTS CO., LTD No. 3 Building, Lifu Plastic, Nanshanyang Industrial Zone, Baisha Town, Minhou, Fuzhou, China CHINA Homewares 44 41% 59% HUAHONG HOLDING GROUP No. -

Situation Update
** NOT FOR GENERAL DISTRIBUTION ** H7N9 situation update FAO / EMPRES – Animal Health 15 October 2013, 1700 hours; Rome Overview Situation: Avian influenza A(H7N9) virus with pandemic potential Country: People’s Republic of China Number of human cases: 136 confirmed; 45 deaths Provinces/municipalities: Beijing and Shanghai; Anhui, Fujian, Guangdong, Hebei, Henan, Hunan, Jiangsu, Jiangxi, Shandong, Zhejiang and Taiwan Province of China; Findings in animals: H7N9 confirmed in chickens, ducks, pigeons and environmental samples: 54 positive samples mainly from live bird markets and vendors FAO actions: liaise with China and partners, monitor situation, explore and assess virus characteristics, conduct market chain analysis, risk assessment, surveillance guidance and communication. Situation update Animals Virologically positive samples confirmed by national authorities Province Duck Pigeon Chicken Environmental Total Shanghai 0 3 10 7 20 Jiangsu 0 2 11 0 13 Anhui 1 0 0 0 1 Henan 0 0 0 2 2 Shandong 0 0 0 3 3 Jiangxi 0 0 1 0 1 Guangdong 0 0 2 0 2 Zhejiang 2 0 8 0 10 Fujian 0 0 0 1 1 TOTAL 3 5 32 13 53 Virologically positive samples reported in peer-reviewed articles Province Duck Pigeon Chicken Environmental Total Zhejiang 0 0 0 61* 61 Shandong 0 8** 0 0 8 TOTAL 0 0 0 0 69 *Eurosurveillance: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20481 **Nature: http://www.nature.com/nature/journal/vaop/ncurrent/full/nature12515.html Humans . Zhejiang province: a 35-year-old man in Shaoxin County was diagnosed with H7N9 avian influenza and is in serious condition. This is the first human case reported since 10 August 2013. -

寶業集團股份有限公司 Baoye Group Company Limited
IMPORTANT If you are in any doubt about this prospectus, you should consult your stockbroker, bank manager, solicitor, professional accountant or other professional adviser. 寶 業 BAOYE 寶業集團股份有限公司 BAOYE GROUP COMPANY LIMITED* (a joint stock limited company incorporated in the People’s Republic of China with limited liability) PUBLIC OFFER AND INTERNATIONAL PLACING Number of Offer Shares : 180,684,000 H Shares (subject to the Over-allotment Option) Number of International Placing Shares : 162,612,000 H Shares (subject to reallocation and the Over-allotment Option) Number of Public Offer Shares : 18,072,000 H Shares (subject to reallocation) Offer Price : not more than HK$1.99 per H Share and expected to be not less than HK$1.25 per H Share Nominal Value : RMB1.00 per H Share Stock Code : 2355 Sponsor FIRST SHANGHAI CAPITAL LIMITED Sole Bookrunner and Joint Lead Manager FIRST SHANGHAI SECURITIES LIMITED Joint Lead Manager GC Capital (Asia) Limited Co-Lead Managers CM-CCS Securities Limited CITIC Capital Markets Limited Worldwide Finance (Securities) Limited The Stock Exchange of Hong Kong Limited and Hong Kong Securities Clearing Company Limited take no responsibility for the contents of this prospectus, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this prospectus. A copy of this prospectus, having attached thereto the documents specified in the paragraph headed “Documents delivered to the Registrar of Companies” in Appendix V to this prospectus, has been registered by the Registrar of Companies in Hong Kong as required by section 342C of the Companies Ordinance. -

Table of Codes for Each Court of Each Level
Table of Codes for Each Court of Each Level Corresponding Type Chinese Court Region Court Name Administrative Name Code Code Area Supreme People’s Court 最高人民法院 最高法 Higher People's Court of 北京市高级人民 Beijing 京 110000 1 Beijing Municipality 法院 Municipality No. 1 Intermediate People's 北京市第一中级 京 01 2 Court of Beijing Municipality 人民法院 Shijingshan Shijingshan District People’s 北京市石景山区 京 0107 110107 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Haidian District of Haidian District People’s 北京市海淀区人 京 0108 110108 Beijing 1 Court of Beijing Municipality 民法院 Municipality Mentougou Mentougou District People’s 北京市门头沟区 京 0109 110109 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Changping Changping District People’s 北京市昌平区人 京 0114 110114 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Yanqing County People’s 延庆县人民法院 京 0229 110229 Yanqing County 1 Court No. 2 Intermediate People's 北京市第二中级 京 02 2 Court of Beijing Municipality 人民法院 Dongcheng Dongcheng District People’s 北京市东城区人 京 0101 110101 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Xicheng District Xicheng District People’s 北京市西城区人 京 0102 110102 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Fengtai District of Fengtai District People’s 北京市丰台区人 京 0106 110106 Beijing 1 Court of Beijing Municipality 民法院 Municipality 1 Fangshan District Fangshan District People’s 北京市房山区人 京 0111 110111 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Daxing District of Daxing District People’s 北京市大兴区人 京 0115 -

Tier 1 Manufacturing Sites
TIER 1 MANUFACTURING SITES - Produced January 2021 SUPPLIER NAME MANUFACTURING SITE NAME ADDRESS PRODUCT TYPE No of EMPLOYEES Albania Calzaturificio Maritan Spa George & Alex 4 Street Of Shijak Durres Apparel 100 - 500 Calzificio Eire Srl Italstyle Shpk Kombinati Tekstileve 5000 Berat Apparel 100 - 500 Extreme Sa Extreme Korca Bul 6 Deshmoret L7Nr 1 Korce Apparel 100 - 500 Bangladesh Acs Textiles (Bangladesh) Ltd Acs Textiles & Towel (Bangladesh) Tetlabo Ward 3 Parabo Narayangonj Rupgonj 1460 Home 1000 - PLUS Akh Eco Apparels Ltd Akh Eco Apparels Ltd 495 Balitha Shah Belishwer Dhamrai Dhaka 1800 Apparel 1000 - PLUS Albion Apparel Group Ltd Thianis Apparels Ltd Unit Fs Fb3 Road No2 Cepz Chittagong Apparel 1000 - PLUS Asmara International Ltd Artistic Design Ltd 232 233 Narasinghpur Savar Dhaka Ashulia Apparel 1000 - PLUS Asmara International Ltd Hameem - Creative Wash (Laundry) Nishat Nagar Tongi Gazipur Apparel 1000 - PLUS Aykroyd & Sons Ltd Taqwa Fabrics Ltd Kewa Boherarchala Gila Beradeed Sreepur Gazipur Apparel 500 - 1000 Bespoke By Ges Unip Lda Panasia Clothing Ltd Aziz Chowdhury Complex 2 Vogra Joydebpur Gazipur Apparel 1000 - PLUS Bm Fashions (Uk) Ltd Amantex Limited Boiragirchala Sreepur Gazipur Apparel 1000 - PLUS Bm Fashions (Uk) Ltd Asrotex Ltd Betjuri Naun Bazar Sreepur Gazipur Apparel 500 - 1000 Bm Fashions (Uk) Ltd Metro Knitting & Dyeing Mills Ltd (Factory-02) Charabag Ashulia Savar Dhaka Apparel 1000 - PLUS Bm Fashions (Uk) Ltd Tanzila Textile Ltd Baroipara Ashulia Savar Dhaka Apparel 1000 - PLUS Bm Fashions (Uk) Ltd Taqwa -

Association of Myopia in Elementary School Students in Jiaojiang District, Taizhou City, China
Hindawi Journal of Ophthalmology Volume 2021, Article ID 3504538, 7 pages https://doi.org/10.1155/2021/3504538 Research Article Association of Myopia in Elementary School Students in Jiaojiang District, Taizhou City, China XinLu ,1 CongcongGuo ,1 BinXu ,1 ChenweiHou ,1 XiaomingHuang ,2 HuiXu ,1 and Zhichun Weng 3 1Jiaojiang Center for Disease Control and Prevention, Taizhou, Zhejiang Province, China 2Eye Hospital (Taizhou Branch), WMU International Eye Hospital of Taizhou, Taizhou, Zhejiang Province, China 3Jiaojiang Education Bureau, Taizhou, Zhejiang Province, China Correspondence should be addressed to Xin Lu; [email protected] Received 18 July 2020; Revised 13 January 2021; Accepted 20 January 2021; Published 27 February 2021 Academic Editor: Alessandro Meduri Copyright © 2021 Xin Lu et al. +is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background. +e aim of our study was to evaluate the prevalence of myopia in elementary school students and to assess the risk factors for myopia. Methods. +is school-based cross-sectional study was performed on students from two elementary schools in Jiaojiang, Taizhou City, China. A total of 556 students, whose age ranged from 9 to 12 years, were included. +e uncorrected visual acuity and noncycloplegic refractive error tests were performed to determine the myopia. Each student was asked to fulfill the questionnaire about the possible factors associated with myopia. Multivariate logistic analyses of risk factors were conducted. Results. +e overall prevalence of myopia among those students was 63.7%, ranged from 53.4% in grade 4 to 72.5% in grade 6. -

Interim Report 2019
INTERIM REPORT 2019 2019 INTERIM REPORT www.cs.ecitic.com I M P O R T A N T N O T I C E The Board and the Supervisory Committee of the Company and the Directors, Supervisors and Senior Management warrant the truthfulness, accuracy and completeness of contents of this interim report and that there is no false representation, misleading statement contained herein or material omission from this interim report, for which they will assume joint and several liabilities. This interim report was considered and approved at the 44th Meeting of the Sixth Session of the Board. All Directors attended the meeting. No Director raised any objection to this interim report. The 2019 interim financial statements of the Company were unaudited. PricewaterhouseCoopers Zhong Tian LLP and PricewaterhouseCoopers issued review opinions in accordance with the China and international review standards, respectively. Mr. ZHANG Youjun, head of the Company, Mr. LI Jiong, the person-in-charge of accounting affairs and Ms. KANG Jiang, head of the Company’s accounting department, warrant that the financial statements set out in this interim report are true, accurate and complete. There was no profit distribution plan or plan of conversion of the capital reserve into the share capital of the Company for the first half of 2019. Forward looking statements, including future plans and development strategies, contained in this interim report do not constitute a substantive commitment to investors by the Company. Investors should be aware of investment risks. There was no appropriation of funds of the Company by the related/connected parties for non-operating purposes. -

List of Main Production Facilities of ALDI Nord's Suppliers for Apparel
List of Main Production Facilities of ALDI Nord‘s Suppliers for Apparel, Home Textiles and Shoes Version: April 2021 Produktionsstättenliste | März 2018 | Seite 0/17 Name Address Number of Employees Commodity Group Bangladesh AB Apparels Ltd. 225, Singair Road, Tetuljhora, Hemayetpur 2001 - 5000 Garment textiles Ador Composite Ltd. 1, C & B Bazar, Gilarchala, Sreepur 1001 - 2000 Garment textiles AKH Eco Apparels Ltd. 495, Balitha, Shahbelishwar, Dhamrai 5001 - 10000 Garment textiles Angshuk Ltd. 133-134, Hamayetpur, Savar 501 - 1000 Garment textiles Apparels Village Ltd. Khagan, Birulia, Savar 2001 - 5000 Garment textiles Aspire Garments Ltd. 491, Dhalla, Singair 2001 - 5000 Garment textiles B.H.I.S. Apparels Ltd. 671, Datta Para, Hossain Market, Tongi 2001 - 5000 Garment textiles Blue Planet Knitwear Ltd. Mulaid, P.O.: Tengra, Sreepur 1001 - 2000 Garment textiles Chaity Composite Ltd. Chotto Silmondi, Tripurdi, Sonargaon 5001 - 10000 Garment textiles Chantik Garments Ltd. Kumkumari, Gouripur, Ashulia, Savar 2001 - 5000 Garment textiles Chorka Textile Ltd. Kajirchor, Danga Bazar, Polash 2001 - 5000 Garment textiles Citadel Apparels Ltd. Joy Bangla Road, Kunia, K.B. Bazar, Gazipur Sadar 501 - 1000 Garment textiles Cotton Dyeing & Finishing Mills Ltd. Vill: Amtoli, Union: 10 No. Habirbari, P.O-Seedstore Bazar, P.S.-Valuka 1001 - 2000 Garment textiles Crossline Factory (Pvt) Ltd. 25, Vadam, Uttarpara, Nishatnagar, Tongi 1001 - 2000 Garment textiles Plot No. 45, 48, 49, 51 & 52; Holding No.: 3/C, Vadam, P.O.: Crossline Knit Fabrics Ltd. 1001 - 2000 Garment textiles Nishatnagar, Tongi, Gazipur-1711, Gazipur Crown Exclusive Wears Ltd. Mawna, Sreepur 2001 - 5000 Garment textiles Crown Fashion & Sweater Industries Ltd. Plot No. 781-782, Vogra, Joydebpur, Gazipur-1704 2001 - 5000 Garment textiles Denim Fashions Ltd. -
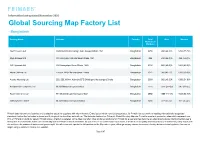
Primark Does Not Own Any Factories and Is Selective About the Suppliers with Whom We Work
Information last updated November 2020 Global Sourcing Map Factory List - Bangladesh Factory Name Address Country Total Men Women Number of Workers A&A Trousers Ltd Haribaritek Pubail College Gate Gazipur Dhaka 1721 Bangladesh 2250 996 (44.3)% 1254 (55.7)% Afiya Knitwear Ltd 10/ 2 Durgapur Ashulia Savar Dhaka 1341 Bangladesh 496 232 (46.8)% 264 (53.2)% AKH Apparels Ltd 128 Hemayetpur Savar Dhaka 1340 Bangladesh 2136 855 (40.0)% 1281 (60.0)% Alpha Clothing Ltd Tenguri, BKSP Ashulia Savar Dhaka Bangladesh 1971 968 (49.1)% 1003 (50.9)% Ananta Huaxiang Ltd 222, 223, H2-H4, Adamjee EPZ Shiddirgonj Narayanganj Dhaka Bangladesh 2038 982 (48.2)% 1056 (51.8)% Anowara Knit Composite Ltd Mulaid Mawna Sreepur Gazipur Bangladesh 2276 1329 (58.4)% 947 (41.6)% Aspire Garments Ltd 491 Dhalla Singair Manikganj 1822 Bangladesh 2992 1389 (46.4)% 1603 (53.6)% ASR Sweater Limited Mulaied Maona Sreepur Gazipur Bangladesh 1458 927 (63.6)% 531 (36.4)% Primark does not own any factories and is selective about the suppliers with whom we work. Every factory which manufactures product for Primark has to commit to meeting internationally recognised standards, before the first order is placed and throughout the time they work with us. The factories featured on Primark’s Global Sourcing Map are Primark’s suppliers’ production sites which represent over 95% of Primark products for sale in Primark stores. A factory is detailed on the Map only after it has produced products for Primark for a year and has become an established supplier. During the first year a factory has to demonstrate that it can consistently work to Primark’s ethical standards, as well as meet our commercial requirements in areas such as quality and timely delivery.