Acute Otitis Externa: an Update PAUL SCHAEFER, MD, Phd, and REGINALD F
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Instruction Sheet: Otitis Externa
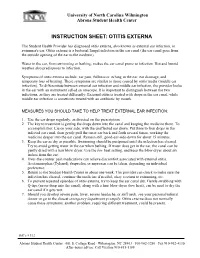
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

Chronic Otitis Media: Histopathological Changes a Post Mortem Study on Temporal Bones
European Review for Medical and Pharmacological Sciences 1999; 3: 175-178 Chronic otitis media: histopathological changes A post mortem study on temporal bones F. SALVINELLI, M. TRIVELLI, F. GRECO, F.H. LINTHICUM JR* Institute of Otolaryngology, “Campus Bio-Medico” University - Rome (Italy) *Department of Histopathology, “House Ear Institute” - Los Angeles, CA (USA) Abstract. – The temporal bones of 4 Materials and Methods deceased individuals, with concomitant chronic otitis media are studied. The various histopathological changes in the middle ear We have studied the histopathological cleft are examined: suppuration, polyps, changes in temporal bones of 4 deceased in- granulation tissue. The possibilities of spon- dividuals, with concomitant chronic OM. taneous healing of a perforated TM and the These patients were donors and agreed indications of surgical treatment are dis- during their life to donate post mortem their cussed. temporal bones to the House Ear Institute as Key Words: a contribution to a better knowledge of tem- Temporal bone, Middle ear, Infection, Chronic in- poral bone diseases. flammation, Metaplasia, Complications. We have removed the temporal bones in our usual way9. Introduction Results Otitis media (OM) is an infection localized Clinical features in the middle ear: mastoid, middle ear cavity, The inflammation, while often indolent, eustachian tube. The classification of OM in- may at times give rise to serious complica- cludes: tions and even cause death. The hearing loss that is a constant concomitant also con- tributes to the immense socio-economic problem. Chronic OM sometimes, but not al- • OM with effusion1-3, without perforation ways, follows an attack of the acute disease. of the tympanic membrane (TM)4-6, due The major feature is discharge from the mid- to an increase of fluid in the middle ear dle ear. -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Inner Ear Infection (Otitis Interna) in Dogs
Hurricane Harvey Client Education Kit Inner Ear Infection (Otitis Interna) in Dogs My dog has just been diagnosed with an inner ear infection. What is this? Inflammation of the inner ear is called otitis interna, and it is most often caused by an infection. The infectious agent is most commonly bacterial, although yeast and fungus can also be implicated in an inner ear infection. If your dog has ear mites in the external ear canal, this can ultimately cause a problem in the inner ear and pose a greater risk for a bacterial infection. Similarly, inner ear infections may develop if disease exists in one ear canal or when a benign polyp is growing from the middle ear. A foreign object, such as grass seed, may also set the stage for bacterial infection in the inner ear. Are some dogs more susceptible to inner ear infection? Dogs with long, heavy ears seem to be predisposed to chronic ear infections that ultimately lead to otitis interna. Spaniel breeds, such as the Cocker spaniel, and hound breeds, such as the bloodhound and basset hound, are the most commonly affected breeds. Regardless of breed, any dog with a chronic ear infection that is difficult to control may develop otitis interna if the eardrum (tympanic membrane) is damaged as it allows bacteria to migrate down into the inner ear. "Dogs with long, heavy ears seem to bepredisposed to chronic ear infections that ultimately lead to otitis interna." Excessively vigorous cleaning of an infected external ear canal can sometimes cause otitis interna. Some ear cleansers are irritating to the middle and inner ear and can cause signs of otitis interna if the eardrum is damaged and allows some of the solution to penetrate too deeply. -

Inner Ear Fibrocytes This Information Is Current As of October 1, 2021
ERK2-Dependent Activation of c-Jun Is Required for Nontypeable Haemophilus influenzae-Induced CXCL2 Upregulation in Inner Ear Fibrocytes This information is current as of October 1, 2021. Sejo Oh, Jeong-Im Woo, David J. Lim and Sung K. Moon J Immunol published online 29 February 2012 http://www.jimmunol.org/content/early/2012/02/29/jimmun ol.1103182 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2012/02/29/jimmunol.110318 Material 2.DC1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on October 1, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published February 29, 2012, doi:10.4049/jimmunol.1103182 The Journal of Immunology ERK2-Dependent Activation of c-Jun Is Required for Nontypeable Haemophilus influenzae-Induced CXCL2 Upregulation in Inner Ear Fibrocytes Sejo Oh,*,1 Jeong-Im Woo,*,1 David J. Lim,*,† and Sung K. Moon* The inner ear, composed of the cochlea and the vestibule, is a specialized sensory organ for hearing and balance. -

Otitis Media and Interna
Otitis Media and Interna (Inflammation of the Middle Ear and Inner Ear) Basics OVERVIEW • Inflammation of the middle ear (known as “otitis media”) and inner ear (known as “otitis interna”), most commonly caused by bacterial infection SIGNALMENT/DESCRIPTION OF PET Species • Dogs • Cats Breed Predilections • Cocker spaniels and other long-eared breeds • Poodles with long-term (chronic) inflammation of the ears (known as “otitis”) or the throat (known as “pharyngitis”) associated with dental disease • Primary secretory otitis media (PSOM) is described in Cavalier King Charles spaniels SIGNS/OBSERVED CHANGES IN THE PET • Depend on severity and extent of the infection; range from no signs, to those related to middle ear discomfort and nervous system involvement • Pain when opening the mouth; reluctance to chew; shaking the head; pawing at the affected ear • Head tilt • Pet may lean, veer, or roll toward the side or direction of the affected ear • Pet's sense of balance may be altered (known as “vestibular deficits”)—persistent, transient or episodic • Involvement of both ears—wide movements of the head, swinging back and forth; wobbly or incoordinated movement of the body (known as “truncal ataxia”), and possible deafness • Vomiting and nausea—may occur during the sudden (acute) phase • Facial nerve damage—the “facial nerve” goes to the muscles of the face, where it controls movement and expression, as well as to the tongue, where it is involved in the sensation of taste; signs of facial nerve damage include saliva and food dropping from the -

An EANM Procedural Guideline
European Journal of Nuclear Medicine and Molecular Imaging https://doi.org/10.1007/s00259-018-4052-x GUIDELINES Clinical indications, image acquisition and data interpretation for white blood cells and anti-granulocyte monoclonal antibody scintigraphy: an EANM procedural guideline A. Signore1 & F. Jamar2 & O. Israel3 & J. Buscombe4 & J. Martin-Comin5 & E. Lazzeri6 Received: 27 April 2018 /Accepted: 6 May 2018 # The Author(s) 2018 Abstract Introduction Radiolabelled autologous white blood cells (WBC) scintigraphy is being standardized all over the world to ensure high quality, specificity and reproducibility. Similarly, in many European countries radiolabelled anti-granulocyte antibodies (anti-G-mAb) are used instead of WBC with high diagnostic accuracy. The EANM Inflammation & Infection Committee is deeply involved in this process of standardization as a primary goal of the group. Aim The main aim of this guideline is to support and promote good clinical practice despite the complex environment of a national health care system with its ethical, economic and legal aspects that must also be taken into consideration. Method After the standardization of the WBC labelling procedure (already published), a group of experts from the EANM Infection & Inflammation Committee developed and validated these guidelines based on published evidences. Results Here we describe image acquisition protocols, image display procedures and image analyses as well as image interpre- tation criteria for the use of radiolabelled WBC and monoclonal antigranulocyte antibodies. Clinical application for WBC and anti-G-mAb scintigraphy is also described. Conclusions These guidelines should be applied by all nuclear medicine centers in favor of a highly reproducible standardized practice. Keywords Infection . -

Management of Acute Otitis Media: Update
Evidence Report/Technology Assessment Number 198 Management of Acute Otitis Media: Update Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290-2007-10056-I Prepared by: RAND Corporation, Santa Monica, CA 90407 Investigators Paul G. Shekelle, M.D., Ph.D. Glenn Takata, M.D., M.S. Sydne J. Newberry, Ph.D. Tumaini Coker, M.D. Mary Ann Limbos, M.D., M.P.H. Linda S. Chan, Ph.D. Martha M. Timmer, M.S. Marika J. Suttorp, M.S. Jason Carter, B.A. Aneesa Motala, B.A. Di Valentine, J.D. Breanne Johnsen, B.A. Roberta Shanman, M.L.S. AHRQ Publication No. 11-E004 November 2010 This report is based on research conducted by the RAND Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290-2007-10056-I). The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This report may be used, in whole or in part, as the basis for the development of clinical practice guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage policies. -

Chronic Otitis Media Is Initiated by a Bulla Cavitation Defect in The
Edinburgh Research Explorer Chronic otitis media is initiated by a bulla cavitation defect in the FBXO11 mouse model Citation for published version: Del-Pozo, J, Macintyre, N, Azar , A, Glover, J, Milne, E & Cheeseman, M 2019, 'Chronic otitis media is initiated by a bulla cavitation defect in the FBXO11 mouse model', Disease Models and Mechanisms, vol. 12, dmm038315, pp. 1-10. https://doi.org/10.1242/dmm.038315 Digital Object Identifier (DOI): 10.1242/dmm.038315 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Disease Models and Mechanisms Publisher Rights Statement: This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution and reproduction in any medium provided that the original work is properly attributed General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 07. Oct. 2021 © 2019. Published by The Company of Biologists Ltd | Disease Models & Mechanisms (2019) 12, dmm038315. -

Manifestation in Ankylosing Spondylitis?
Annals ofthe Rheumatic Diseases 1992; 51: 655-657 655 Chronic otitis media: a new extra-articular Ann Rheum Dis: first published as 10.1136/ard.51.5.655 on 1 May 1992. Downloaded from manifestation in ankylosing spondylitis? A E Camilleri, I R C Swan, E Murphy, R D Sturrock Abstract steroidal anti-inflammatory drugs (NSAIDs), Foliowing a study reporting a fourfold increase second line drug treatment, age of onset of in the occurrence of chronic otitis media in ankylosing spondylitis, duration of ankylosing patients with ankylosing spondylitis, this spondylitis, HLA-B27 status, peripheral joint prospective study examines this association disease, erythrocyte sedimentation rate, wall to with respect to severity, duration of disease, tragus distance, spondylometry, presence of and acute phase in ankylosing spondylitis. extra-articular manifestations (uveitis and aortic Forty two consecutive patients with classical incompetence), duration of early morning stiff- ankylosing spondylitis seen at the rheumato- ness, presence of rheumatoid factor, and serum logy clinic of a teaching hospital where the levels of C reactive protein, IgA, IgG, and IgM. features of ankylosing spondylitis were re- All serum levels and measurements were current corded had an otological examination by an or within the previous three months. Clinical otolaryngologist. The occurrence of chronic otological examination was carried out after otitis media (all categories) was 12/42 (29%). cleaning the external auditory canals where The acute phase serum markers (C reactive necessary to allow inspection of the whole protein and IgG) were increased in patients tympanic membrane. with active or inactive chronic otitis media. Chronic otitis media was categorised as active, Extra-articular manifestations were signifi- inactive, or healed.4 Active chronic otitis media candy more common in the chronic otitis was defined as a chronic perforation of the media group than in those with no history of tympanic membrane with signs ofinflammation, chronic otitis media. -

Differential Diagnosis and Treatment of Hearing Loss JON E
Differential Diagnosis and Treatment of Hearing Loss JON E. ISAACSON, M.D., and NEIL M. VORA, M.D., Milton S. Hershey Medical Center, Hershey, Pennsylvania Hearing loss is a common problem that can occur at any age and makes verbal communication difficult. The ear is divided anatomically into three sections (external, middle, and inner), and pathology contributing to hearing loss may strike one or more sections. Hearing loss can be cat- egorized as conductive, sensorineural, or both. Leading causes of conductive hearing loss include cerumen impaction, otitis media, and otosclerosis. Leading causes of sensorineural hear- ing loss include inherited disorders, noise exposure, and presbycusis. An understanding of the indications for medical management, surgical treatment, and amplification can help the family physician provide more effective care for these patients. (Am Fam Physician 2003;68:1125-32. Copyright© 2003 American Academy of Family Physicians) ore than 28 million Amer- tive, the sound will be heard best in the icans have some degree of affected ear. If the loss is sensorineural, the hearing impairment. The sound will be heard best in the normal ear. differential diagnosis of The sound remains midline in patients with hearing loss can be sim- normal hearing. Mplified by considering the three major cate- The Rinne test compares air conduction gories of loss. Conductive hearing loss occurs with bone conduction. The tuning fork is when sound conduction is impeded through struck softly and placed on the mastoid bone the external ear, the middle ear, or both. Sen- (bone conduction). When the patient no sorineural hearing loss occurs when there is a longer can hear the sound, the tuning fork is problem within the cochlea or the neural placed adjacent to the ear canal (air conduc- pathway to the auditory cortex. -

Tinnitus: Ringing in the SYMPTOMS Ears
Tinnitus: Ringing in the SYMPTOMS Ears By Vestibular Disorders Association TINNITUS WHAT IS TINNITUS? An abnormal noise perceived in one or both Tinnitus is abnormal noise perceived in one or both ears or in the head. ears or in the head. It Tinnitus (pronounced either “TIN-uh-tus” or “tin-NY-tus”) may be can be experienced as a intermittent, or it might appear as a constant or continuous sound. It can ringing, hissing, whistling, be experienced as a ringing, hissing, whistling, buzzing, or clicking sound buzzing, or clicking sound and can vary in pitch from a low roar to a high squeal. and can vary in pitch. Tinnitus is very common. Most studies indicate the prevalence in adults as falling within the range of 10% to 15%, with a greater prevalence at higher ages, through the sixth or seventh decade of life. 1 Gender distinctions ARTICLE are not consistently reported across studies, but tinnitus prevalence is significantly higher in pregnant than non-pregnant women. 2 The most common form of tinnitus is subjective tinnitus, which is noise that other people cannot hear. Objective tinnitus can be heard by an examiner positioned close to the ear. This is a rare form of tinnitus, 068 occurring in less than 1% of cases. 3 Chronic tinnitus can be annoying, intrusive, and in some cases devastating to a person’s life. Up to 25% of those with chronic tinnitus find it severe DID THIS ARTICLE enough to seek treatment. 4 It can interfere with a person’s ability to hear, HELP YOU? work, and perform daily activities.