Enhanced and Accelerated Lymphoproliferation in Fas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Shigekazu Nagata Is Better Known for His Work on Apoptosis
© 2001 Nature Publishing Group http://medicine.nature.com NEWS Having originally researched the activities of the potent hematopeotic stimulator of bone-marrow cells, granulocyte colony stimulating factor, Shigekazu Nagata is better known for his work on apoptosis. Here, one of Japan’s most renowned biomedical scientists outlines the path that has taken him full circle: from stimulating cells to grow, to finding out how they die, to tying the two processes together. Shigekazu Nagata For a man who spends most of his time clusively activated in apoptosis. He says Charles Weissmann. He took the job be- thinking about death, Shigekazu Nagata is there are several questions left to be an- cause at that time, “almost no one was remarkably upbeat. For over a decade, he swered concerning the Fas pathway. using recombinant DNA technology in has been making a name for himself with Central among them is, how does the onco- Japan.” He credits his experience in research on apoptosis, the mechanism of gene product Bcl-2 block apoptosis? Weissman’s lab with forming the basis for programmed cell death, and during that However, he has no personal plans to work his future studies and teaching him an “or- time he has watched the field come alive. on an answer to that question, perhaps be- derliness and logical procedure” to re- “Medline publications on apoptosis have cause he has become a victim of his own search. In 1982, he returned to IMS for a risen from only a couple of hundred in success at propagating interest in cell death. short time before moving to the OBI in 1990 to over 10,000 this year,” he says with “There are so many other 1987 and then to taking up a satisfied nod. -

A Sublethal ATP11A Mutation Associated with Neurological Deterioration Causes Aberrant Phosphatidylcholine Flipping in Plasma Membranes
A sublethal ATP11A mutation associated with neurological deterioration causes aberrant phosphatidylcholine flipping in plasma membranes Katsumori Segawa, … , Shigeo Kure, Shigekazu Nagata J Clin Invest. 2021. https://doi.org/10.1172/JCI148005. Research In-Press Preview Cell biology Metabolism Graphical abstract Find the latest version: https://jci.me/148005/pdf A sublethal ATP11A mutation associated with neurological deterioration causes aberrant phosphatidylcholine flipping in plasma membranes Katsumori Segawa,1,16,17 Atsuo Kikuchi,2,16 Tomoyasu Noji,3 Yuki Sugiura,4 Keita Hiraga,3 Chigure Suzuki,5,6 Kazuhiro Haginoya,7,8 Yasuko Kobayashi,7,9 Mitsuhiro Matsunaga,1 Yuki Ochiai,1 Kyoko Yamada,1 Takuo Nishimura,1,18 Shinya Iwasawa,2 Wataru Shoji,10 Fuminori Sugihara,11 Kohei Nishino,12 Hidetaka Kosako,12 Masahito Ikawa,13 Yasuo Uchiyama,5,6 Makoto Suematsu,4 Hiroshi Ishikita,3 Shigeo Kure,2,14 Shigekazu Nagata1, 15* 1Laboratory of Biochemistry & Immunology, World Premier International Research Center, Immunology Frontier Research Center, 11Central Instrumentation Laboratory, Research Institute for Microbial Diseases, 13Department of Experimental Genome Research, Research Institute for Microbial Diseases, 15Center for Infectious Disease Education and Research, Osaka University, Suita, Osaka, Japan. 2Department of Pediatrics, Tohoku University School of Medicine, 10Frontier Research Institute for Interdisciplinary Sciences, and 14Tohoku Medical Megabank Organization, Tohoku University, Sendai, Miyagi, Japan. 3Research Center for Advanced Science and Technology, The University of Tokyo, Tokyo, Japan. 4Department of Biochemistry, Keio University School of Medicine, Tokyo, Japan. 5Department of Cellular and Molecular Pharmacology, and 6Department of Cellular and Neuropathology, Juntendo University Graduate School of Medicine, Tokyo, Japan. 7Department of Pediatric Neurology, Takuto Rehabilitation Center for Children, Sendai, Miyagi, Japan. -

General Report on 8Th IDS
General Report on 8th IDS I) Local Organizing Committee Toshiaki Hanafusa (President, First Department of Internal Medicine, Osaka Medical College) Tetsuro Kobayashi (Vice President, Third Department of Internal Medicine, Yamanashi University) Hiroshi Ikegami (Osaka University) Akihisa Imagawa (Osaka Medical College) Yasuko Uchigata (Tokyo Women’s Medical University) Eiji Kawasaki (Nagasaki University) Kaichi Kida (Ehime University) Akira Shimada (Keio University) Kazuma Takahashi (Tohoku University) Masao Nagata (Kobe University) Eiichi Makino (Ehime University) Taro Maruyama (Saitama Social Insurance Hospital) II) Overseas Speakers GS. Eisenbarth (Barbara Davis Center UCHSC, USA) E. Gale (Southmead Hospital, Bristol, UK) DM. Harlan (National Institutes of Health, USA) LC. Harrison (The Walter and Eliza Hall Institute of Medical Research, Australia) YS. Park (Hanyang University, Korea) BO. Roep (Leiden University Medical Center, the Netherlands) L. Chatenoud (Paris, France) III) Local Speakers Tadatsugu Taniguchi (Tokyo University) Shigekazu Nagata (Osaka University) Shimon Sakaguchi (Kyoto University) Jun-ichi Miyazaki (Osaka University) Shizuo Akira (Osaka University) IV) Number of Participants 75 from Japan 145 from Overseas (12 accompanying persons) 1 IDS-8 participants list Accom. Country Subtotal Member Non-Member Person Australia 9 6 3 Belgium 1 0 1 Brazil 1 0 1 Canada 4 3 1 1 Denmark 2 1 1 Finland 21 13 8 France 2 2 0 Germany 3 3 0 India 1 0 1 Israel 1 1 0 1 Italy 2 1 1 1 Japan 75 46 29 3 Korea 9 2 7 New Zealand 2 2 0 Norway 2 2 0 1 Spain 2 1 1 Sweden 17 11 6 1 The Czech Republic 2 2 0 The Netherlands 4 3 1 U.K. -

World Premier International Research Center Initiative (WPI) FY2014 WPI Project Progress Report (Post-Interim Evaluation)
World Premier International Research Center Initiative (WPI) FY2014 WPI Project Progress Report (Post-Interim Evaluation) Host Institutio n Osaka University Host Institution Head Toshio Hirano Research Cente r Immunology Frontier Research Canter Center D ire ctor Shizuo Akira Common instructions: * Unless otherwise specified, prepare this report from the timeline of 31 March 2015. * So as to base this fiscal year’s follow-up review on the document ”Post-interim evaluation revised center project,” please prepare this report from the perspective of the revised project. * Use yen (¥) when writing monetary amounts in the report. If an exchange rate is used to calculate the yen amount, give the rate. Summary of State of WPI Center Project Progress (write within two pages) IFReC was established as a leading Institute in Immunology and Medicine in Osaka University through the support of WPI program. Our institute provides a highly equipped research platform for young next generation researchers and world premier scientists who have contributed greatly in studies of cytokines, molecular mechanisms of innate immunity, cell death, and regulation of immune system. Our mission in WPI is to accelerate immunology research as well as develop fusion studies with other fields, systems reform of the host institute, and globalization of university and our society. Research of the highest world level: IFReC has continued to publish high quality research activities in highly reputable academic journals during FY2014 in innate immunity, acquired immunity, and the immune regulatory mechanism under the prominent leadership of center director Shizuo Akira, with 195 “WPI papers”, whose author(s) can be identified as affiliated with the WPI program. -

Tumor Apoptosis, Respectively by Fas-Fas Ligand- and Perforin-Induced Recombinant IL-12 Are Mediated Primarily Administration Of
Differential Antitumor Effects of Administration of Recombinant IL-18 or Recombinant IL-12 Are Mediated Primarily by Fas-Fas Ligand- and Perforin-Induced Tumor Apoptosis, Respectively1 Wataru Hashimoto,* Tadashi Osaki,2* Haruki Okamura,‡ Paul D. Robbins,† Masashi Kurimoto,§ Shigekazu Nagata,¶ Michael T. Lotze,*† and Hideaki Tahara3*† Systemic administration of rIL-18 protein to mice significantly suppresses the growth of murine tumor cell lines. The antitumor effect of IL-18 appears to be primarily mediated by asialo GM11 cells. Since IL-18 enhances Fas ligand (FasL) expression on NK cell lines, the IL-18 antitumor effects could be mediated by FasL-induced cross-linking of Fas and subsequent tumor apoptosis. To address this question, rIL-18 or rIL-12 was administered to animals bearing the CL8-1 melanoma inoculated intradermally into wild type (wt), lymphoproliferation gene (lpr) (Fas deficient), or generalized lymphoproliferative disease gene (gld) (FasL deficient) mice. Although rIL-12 treatment retained significant antitumor effects in gld and lpr mice, those of rIL-18 administration were completely abrogated in gld but not lpr or wt mice. In vitro cytotoxicity was significantly enhanced against NK-sensitive YAC-1 cells and CL8-1 cells by rIL-18 administration to wt mice, but not to gld mice. Furthermore, rIL-18 administration augmented the cytotoxicity of liver lymphocytes harvested from perforin-deficient mice, whereas rIL-12 administration did not. Consistent with the role of this pathway, rIL-18 administration also up-regulates the expression of FasL mRNA in splenocytes. Lysis of CL8-1 cells induced by anti-Fas agonistic Ab was enhanced about 1.4-fold by IFN-g, a cytokine that is induced by IL-18 in vitro and in vivo. -
Functional Expression of the P2X7 ATP
Functional Expression of the P2X7 ATP Receptor Requires Eros Yuta Ryoden, Toshihiro Fujii, Katsumori Segawa and Shigekazu Nagata This information is current as of September 27, 2021. J Immunol published online 20 December 2019 http://www.jimmunol.org/content/early/2019/12/20/jimmun ol.1900448 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2019/12/20/jimmunol.190044 Material 8.DCSupplemental Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 27, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2019 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published December 20, 2019, doi:10.4049/jimmunol.1900448 The Journal of Immunology Functional Expression of the P2X7 ATP Receptor Requires Eros Yuta Ryoden, Toshihiro Fujii,1 Katsumori Segawa, and Shigekazu Nagata In response to extracellular ATP, the purinergic receptor P2X7 mediates various biological processes, including phosphatidylserine (PtdSer) exposure, phospholipid scrambling, dye uptake, ion transport, and IL-1b production. A genome-wide CRISPR screen for molecules responsible for ATP-induced PtdSer exposure identified a transmembrane protein, essential for reactive oxygen species (Eros), as a necessary component for P2X7 expression. -
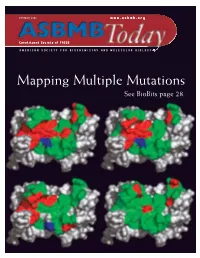
Mapping Multiple Mutations See Biobits Page 28
OCTOBER 2006 www.asbmb.org Constituent Society of FASEB AMERICAN SOCIETY FOR BIOCHEMISTRY AND MOLECULAR BIOLOGY Mapping Multiple Mutations See BioBits page 28. Why Choose 21 st Century Biochemicals For Custom Peptides and Antibodies? “…the dual phosphospecific antibody you “…of the 15 custom antibodies we ordered from your company, 13 worked. “…our in-house QC lab confirmed the Thanks for the great work!” high purity of the peptide.” Over 70 years combined experience manufacturing peptides and anti- bodies Put our expertise to work for you in a collaborative atmosphere The Pinnacle – Affinity Purified Antibodies >85% Success Rate! Peptide Sequencing Included for 100% Guaranteed Peptide Fidelity Complete 2 rabbit protocol with PhD technical support and $ 1675 epitope design ◆ From HPLC purified peptide to affinity purified antibody with no hidden charges!..........$1895 Special pricing through December 3 1, 2006 Phosphospecific Antibody Experts ◆ Custom Phosphospecific Ab’s as low as $2395 Come speak with our scientists at Neuroscience in Atlanta, GA - Booth 2127 and HUPO in Long Beach, CA - Booth 231 www.21stcenturybio.com 33 Locke Drive, Marlboro, MA 01752 Made in the P: 508.303.8222 Toll-free: 877.217.8238 U.S.A. F: 508.303.8333 E: [email protected] www.asbmb.org AMERICAN SOCIETY FOR BIOCHEMISTRY AND MOLECULAR BIOLOGY OCTOBER 2006 Volume 5, Issue 7 features 8 Osaka Bioscience Institute: A World Leader in Scientific Research 11 JLR Looks at Systems Biology 12 Education and Professional Development ON THE COVER: Human growth hormone 14 Judith Klinman to Receive ASBMB-Merck Award residues colored by contribution to receptor 15 Scott Emr Selected for ASBMB-Avanti Award recognition: red, favorable; 16 The Chromosome Cycle green, neutral; blue, unfavorable. -

Engulfment of Apoptotic Cells Locus-1 in a Subset of Macrophages for Expression of Developmental Endothelial
Expression of Developmental Endothelial Locus-1 in a Subset of Macrophages for Engulfment of Apoptotic Cells This information is current as Rikinari Hanayama, Masato Tanaka, Keiko Miwa and of September 29, 2021. Shigekazu Nagata J Immunol 2004; 172:3876-3882; ; doi: 10.4049/jimmunol.172.6.3876 http://www.jimmunol.org/content/172/6/3876 Downloaded from References This article cites 49 articles, 16 of which you can access for free at: http://www.jimmunol.org/content/172/6/3876.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 29, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2004 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Expression of Developmental Endothelial Locus-1 in a Subset of Macrophages for Engulfment of Apoptotic Cells1 Rikinari Hanayama,* Masato Tanaka,*† Keiko Miwa,*‡ and Shigekazu Nagata2*‡§ A major function of macrophages is to engulf apoptotic cells to prevent them from releasing noxious materials as they die. -

DNA-Mediated Cyclic GMP−AMP Synthase− Dependent and −Independent Regulation of Innate Immune Responses
DNA-Mediated Cyclic GMP−AMP Synthase− Dependent and −Independent Regulation of Innate Immune Responses This information is current as Kou Motani, Shinji Ito and Shigekazu Nagata of September 28, 2021. J Immunol 2015; 194:4914-4923; Prepublished online 8 April 2015; doi: 10.4049/jimmunol.1402705 http://www.jimmunol.org/content/194/10/4914 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2015/04/08/jimmunol.140270 Material 5.DCSupplemental References This article cites 57 articles, 19 of which you can access for free at: http://www.jimmunol.org/ http://www.jimmunol.org/content/194/10/4914.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 28, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2015 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology DNA-Mediated Cyclic GMP–AMP Synthase–Dependent and –Independent Regulation of Innate Immune Responses Kou Motani,*,† Shinji Ito,‡ and Shigekazu Nagata* Cytoplasmic DNA activates cyclic GMP–AMP synthase (cGAS) to produce cyclic 29-5939-59GMP–AMP dinucleotide (295 9cGAMP). -

Swiss-Kyoto Symposium 21–22 November 2013 ETH Zurich and the University of Zurich Switzerland
Swiss-Kyoto Symposium 21–22 November 2013 ETH Zurich and the University of Zurich Switzerland Conference Booklet ETH Global 1 Swiss-Kyoto Symposium 2013 2 Swiss-Kyoto Symposium 2013 Table of Contents Introduction 5 Welcome from Organising Institutions 6 Welcome from the Ambassador of Japan 8 Institutional Portraits 9 Programme 13 Overview of Parallel Scientific Sessions 15 Keynote Speakers’ Profiles 16 Executive Speakers’ Profiles 17 Parallel Scientific Session Programmes and Participants’ Profiles H1 Molecular and Cellular Basis of Development, Tissue Repair and Disease 21 H2 Magnetic Resonance 31 H3 Condensed Matter Physics 39 H4 Nanoelectronics and Nanophotonics 57 H5 Organic Chemistry and Materials Chemistry 67 Z1 Product Development and Manufacturing 73 Z2 Advanced Nano-/Biotechnology 81 Z3 Energy 87 Z4 Astrophysics 97 Z5 AI and Robotics 103 Z6 Natural Hazards and Disaster Prevention Research 109 U1 Virtual Ape 117 U2 Plants and Environment 123 U3 Finance and Risk 133 U4 Extentialismus heute 139 U5 Materials for Energy, Environment, and Life 145 Maps 151 General Information 154 Participants List 155 3 Swiss-Kyoto Symposium 2013 4 Swiss-Kyoto Symposium 2013 Swiss-Kyoto Symposium 2013 Introduction In 2014 Switzerland and Japan are celebrating the 150th anniversary of diplomatic relations between the two countries. Around the anniversary several cultural and scientific events are planned to foster cooperation and initiate new joint activities building on the long standing friendship. The Japanese-Swiss partnership extends to many levels with science and technology playing an important role. Building on the high innovation power, the quality of their research institutions and the strong investment in science and technology, Switzerland and Japan have established a strategic bilateral Science and Technology cooperation. -

Necrotic Death Pathway in Fas Receptor Signaling
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Necrotic Death Pathway in Fas Receptor Signaling Hirotaka Matsumura,* Yusuke Shimizu,* Yoshiyuki Ohsawa,‡ Atsuo Kawahara,* Yasuo Uchiyama,‡ and Shigekazu Nagata*§ *Department of Genetics and ‡Department of Cell Biology and Anatomy, Osaka University Medical School, Osaka 565-0871, Japan; and §Core Research for Evolutional Science and Technology, Japan Science and Technology Corporation, Osaka 565-0871, Japan Abstract. A caspase 8–deficient subline (JB6) of hu- with Fas ligand or anti–mouse Fas antibodies, the cells man Jurkat cells can be killed by the oligomerization of died, showing characteristics of apoptosis. A broad Fas-associated protein with death domain (FADD). caspase inhibitor (z-VAD–fmk) blocked the apoptotic This cell death process is not accompanied by caspase morphological changes and the release of cytochrome activation, but by necrotic morphological changes. c. However, the cells still died, and this cell death pro- Here, we show that the death effector domain of cess was accompanied by a strong reduction in ⌬⌿m, as FADD is responsible for the FADD-mediated necrotic well as necrotic morphological changes. The presence pathway. This process was accompanied by a loss of mi- of z-VAD–fmk and pyrrolidine dithiocarbamate to- tochondrial transmembrane potential (⌬⌿m), but not gether blocked cell death, suggesting that both apop- by the release of cytochrome c from mitochondria. Pyr- totic and necrotic pathways can be activated through rolidine dithiocarbamate, a metal chelator and antioxi- the Fas death receptor. dant, efficiently inhibited the FADD-induced reduction of ⌬⌿m and necrotic cell death. -

ASBMB FELLOWS Planning a Scientific Conference? the ASBMB Is Here to Help
Vol. 20 / No. 5 / May 2021 FIRST CLASS Meet the inaugural ASBMB FELLOWS Planning a scientific conference? The ASBMB is here to help. LEARN MORE: asbmb.org/meetings-events/propose-event CONTENTS NEWS FEATURES PERSPECTIVES 2 32 44 EDITOR’S NOTE TARGETING 20,000 PROTEINS WINNERS OF THE ‘AHA MOMENTS’ Planning a scientific conference? ‘Share your aha moments!’ BY 2035 ESSAY CONTEST 44 Finding a common ancestor 4 38 45 Dreaming of Western blots MEMBER UPDATE EXPLORING UNDERAPPRECIATED 46 Beauty in brown The ASBMB is here to help. MOLECULES AND NEW CITIES 47 Fringe inspiration 8 47 A life filled with aha moments IN MEMORIAM 48 The first to know 49 The right experiment 9 49 Prepared mind leads to life-saving RETROSPECTIVE medical advice Remembering Curtiss, former JLR associate editor 50 Superhero science 51 Not quite out of the box 10 MEMBER NEWS 52 First class: Meet the inaugural FIVE QUESTIONS ASBMB fellows Alanna Mitsopoulos: “I could be happy doing other things” 20 LIPID NEWS Ceramides’ role in liver disease 10 16 JOURNAL NEWS 21 JLR names new junior associate editors 23 Study reveals experimental targets for lymphoma research 24 Researchers target cell membrane for cancer research 25 Parasitic secretions create 32 microenvironment for survival 44 26 From the journals LEARN MORE: 20 38 asbmb.org/meetings-events/propose-event 52 MAY 2021 ASBMB TODAY 1 EDITOR’S NOTE Vol. 20 / No. 5 / May 2021 THE MEMBER MAGAZINE OF THE AMERICAN SOCIETY FOR BIOCHEMISTRY AND MOLECULAR BIOLOGY ‘Share your aha moments!’ THE MEMBER MAGAZINE OF THE AMERICAN SOCIETY FOR BIOCHEMISTRYOFFICERS ANDCOUNCIL MOLECULAR MEMBERS BIOLOGY Suzanne Barbour Toni M.