Use of Calretinin, CD56, and CD34 for Differential Diagnosis of Schwannoma and Neurofibroma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplemental Information to Mammadova-Bach Et Al., “Laminin Α1 Orchestrates VEGFA Functions in the Ecosystem of Colorectal Carcinogenesis”
Supplemental information to Mammadova-Bach et al., “Laminin α1 orchestrates VEGFA functions in the ecosystem of colorectal carcinogenesis” Supplemental material and methods Cloning of the villin-LMα1 vector The plasmid pBS-villin-promoter containing the 3.5 Kb of the murine villin promoter, the first non coding exon, 5.5 kb of the first intron and 15 nucleotides of the second villin exon, was generated by S. Robine (Institut Curie, Paris, France). The EcoRI site in the multi cloning site was destroyed by fill in ligation with T4 polymerase according to the manufacturer`s instructions (New England Biolabs, Ozyme, Saint Quentin en Yvelines, France). Site directed mutagenesis (GeneEditor in vitro Site-Directed Mutagenesis system, Promega, Charbonnières-les-Bains, France) was then used to introduce a BsiWI site before the start codon of the villin coding sequence using the 5’ phosphorylated primer: 5’CCTTCTCCTCTAGGCTCGCGTACGATGACGTCGGACTTGCGG3’. A double strand annealed oligonucleotide, 5’GGCCGGACGCGTGAATTCGTCGACGC3’ and 5’GGCCGCGTCGACGAATTCACGC GTCC3’ containing restriction site for MluI, EcoRI and SalI were inserted in the NotI site (present in the multi cloning site), generating the plasmid pBS-villin-promoter-MES. The SV40 polyA region of the pEGFP plasmid (Clontech, Ozyme, Saint Quentin Yvelines, France) was amplified by PCR using primers 5’GGCGCCTCTAGATCATAATCAGCCATA3’ and 5’GGCGCCCTTAAGATACATTGATGAGTT3’ before subcloning into the pGEMTeasy vector (Promega, Charbonnières-les-Bains, France). After EcoRI digestion, the SV40 polyA fragment was purified with the NucleoSpin Extract II kit (Machery-Nagel, Hoerdt, France) and then subcloned into the EcoRI site of the plasmid pBS-villin-promoter-MES. Site directed mutagenesis was used to introduce a BsiWI site (5’ phosphorylated AGCGCAGGGAGCGGCGGCCGTACGATGCGCGGCAGCGGCACG3’) before the initiation codon and a MluI site (5’ phosphorylated 1 CCCGGGCCTGAGCCCTAAACGCGTGCCAGCCTCTGCCCTTGG3’) after the stop codon in the full length cDNA coding for the mouse LMα1 in the pCIS vector (kindly provided by P. -

Neurofibromatosis Type 2 (NF2)
International Journal of Molecular Sciences Review Neurofibromatosis Type 2 (NF2) and the Implications for Vestibular Schwannoma and Meningioma Pathogenesis Suha Bachir 1,† , Sanjit Shah 2,† , Scott Shapiro 3,†, Abigail Koehler 4, Abdelkader Mahammedi 5 , Ravi N. Samy 3, Mario Zuccarello 2, Elizabeth Schorry 1 and Soma Sengupta 4,* 1 Department of Genetics, Cincinnati Children’s Hospital, Cincinnati, OH 45229, USA; [email protected] (S.B.); [email protected] (E.S.) 2 Department of Neurosurgery, University of Cincinnati, Cincinnati, OH 45267, USA; [email protected] (S.S.); [email protected] (M.Z.) 3 Department of Otolaryngology, University of Cincinnati, Cincinnati, OH 45267, USA; [email protected] (S.S.); [email protected] (R.N.S.) 4 Department of Neurology, University of Cincinnati, Cincinnati, OH 45267, USA; [email protected] 5 Department of Radiology, University of Cincinnati, Cincinnati, OH 45267, USA; [email protected] * Correspondence: [email protected] † These authors contributed equally. Abstract: Patients diagnosed with neurofibromatosis type 2 (NF2) are extremely likely to develop meningiomas, in addition to vestibular schwannomas. Meningiomas are a common primary brain tumor; many NF2 patients suffer from multiple meningiomas. In NF2, patients have mutations in the NF2 gene, specifically with loss of function in a tumor-suppressor protein that has a number of synonymous names, including: Merlin, Neurofibromin 2, and schwannomin. Merlin is a 70 kDa protein that has 10 different isoforms. The Hippo Tumor Suppressor pathway is regulated upstream by Merlin. This pathway is critical in regulating cell proliferation and apoptosis, characteristics that are important for tumor progression. -

Information About Mosaic Neurofibromatosis Type 2 (NF2)
Information about mosaic Neurofibromatosis type 2 (NF2) NF2 occurs because of a mutation (change) in the NF2 gene. When this change is present at the time of conception the changed gene will be present in all the cells of the baby. When this mutation occurs later in the development of the forming embryo, the baby will go on to have a mix of cells: some with the “normal” genetic information and some with the changed information. This mix of cells is called mosaicism. Approximately half the people who have a diagnosis of NF2 have inherited the misprinted NF2 gene change from their mother or father who will also have NF2. They will have that misprinted gene in all the cells of their body. When they have their children, there will be a 1 in 2 chance of passing on NF2 to each child they have. However about half of people with NF2 are the first person in the family to be affected. They have no family history and have not inherited the condition from a parent. When doctors studied this group of patients more closely they noticed certain characteristics. Significantly they observed that fewer children had inherited NF2 than expected some people in this group had relatively mild NF2 NF2 tumours in some patients tended to grow on one side of their body rather than both sides that when a blood sample was tested to identify the NF2 gene, the gene change could not be found in 30-40% of people This lead researchers to conclude that this group of people were most likely to be mosaic for NF2 i.e. -

Simultaneous Neurofibroma and Schwannoma of the Sciatic Nerve
Simultaneous Neurofibroma and Schwannoma of the Sciatic Nerve 1 4 1 1 2 3 1 S. A. Sintzoff, Jr.,I.5 W . 0. Bank, · P. A. Gevenois, C. Matos, J. Noterman, J. Flament-Durand, and J. Struyven Summary: The authors report a case of simultaneously occur MR imaging was performed on a 0.5-T system (Gyro ring neurofibroma and schwannoma of the sciatic nerve and scan T5, Philips Medical Systems, Eindhoven, The Neth discuss the complementary aspects of MR and OS. The Schwan erlands) using a wrap-around knee surface coil in order to norna was well-defined and showed distal enhancement on better define the relationships between the tumors and the sonographic evaluation, whereas the neurofibroma was ill-de nerve. Each tumor was isointense to the normal nerve on fined; both tumors were hypoechoic. Tl- and T2-weighted MR T1-weighted images and hyperintense to it on proton Images revealed similar signal characteristics of the two tumors, density and T2-weighted images (Fig. 2A-2C). After intra but Intense enhancement following administration of gadolin venous gadolinium-DTPA injection, the distal mass showed ium-DTPA distinguished the schwannoma from the neurofi intense enhancement, conserving a thin hypointense border broma. (Fig. 2D). Physical and neurologic examination, MR of the central nervous system and skeletal radiographs failed to Index terms: Nerves, sciatic; Neuroma; Schwannoma demonstrate any additional lesions, permitting the reason able exclusion of neurofibromatosis types 1 and 2. Schwannomas and neurofibromas are com Surgical exposure demonstrated the two tumors on the external popliteal nerve (Fig. 3). The distal tumor could be (1, mon peripheral nerve neoplasms 2). -

Central Nervous System Tumors General ~1% of Tumors in Adults, but ~25% of Malignancies in Children (Only 2Nd to Leukemia)
Last updated: 3/4/2021 Prepared by Kurt Schaberg Central Nervous System Tumors General ~1% of tumors in adults, but ~25% of malignancies in children (only 2nd to leukemia). Significant increase in incidence in primary brain tumors in elderly. Metastases to the brain far outnumber primary CNS tumors→ multiple cerebral tumors. One can develop a very good DDX by just location, age, and imaging. Differential Diagnosis by clinical information: Location Pediatric/Young Adult Older Adult Cerebral/ Ganglioglioma, DNET, PXA, Glioblastoma Multiforme (GBM) Supratentorial Ependymoma, AT/RT Infiltrating Astrocytoma (grades II-III), CNS Embryonal Neoplasms Oligodendroglioma, Metastases, Lymphoma, Infection Cerebellar/ PA, Medulloblastoma, Ependymoma, Metastases, Hemangioblastoma, Infratentorial/ Choroid plexus papilloma, AT/RT Choroid plexus papilloma, Subependymoma Fourth ventricle Brainstem PA, DMG Astrocytoma, Glioblastoma, DMG, Metastases Spinal cord Ependymoma, PA, DMG, MPE, Drop Ependymoma, Astrocytoma, DMG, MPE (filum), (intramedullary) metastases Paraganglioma (filum), Spinal cord Meningioma, Schwannoma, Schwannoma, Meningioma, (extramedullary) Metastases, Melanocytoma/melanoma Melanocytoma/melanoma, MPNST Spinal cord Bone tumor, Meningioma, Abscess, Herniated disk, Lymphoma, Abscess, (extradural) Vascular malformation, Metastases, Extra-axial/Dural/ Leukemia/lymphoma, Ewing Sarcoma, Meningioma, SFT, Metastases, Lymphoma, Leptomeningeal Rhabdomyosarcoma, Disseminated medulloblastoma, DLGNT, Sellar/infundibular Pituitary adenoma, Pituitary adenoma, -
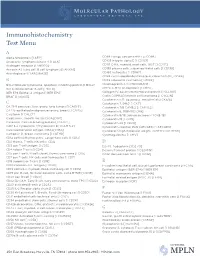
IHC Test Menu
Immunohistochemistry Test Menu A Alpha fetoprotein [I AFP] CD99 Ewings sarcoma PNET [I CD99] Anaplastic lymphoma kinase -1 [I ALK] CD103 Integrin alpha E [I CD103] Androgen receptor [I ANDRO]* CD117 C-Kit, myeloid, mast cells, GIST [I CD117] Annexin A1, hairy cell, B cell lymphoma [I ANXA1] CD138 plasma cells, subset epithelial cells [I CD138] Anti-Arginase-1 [I ARGINASE] CD163 histiocytes [I CD163] CDK4 cyclin-depdendent kinase-4, clone DCS-31 [I CDK4] B CDX2 colorectal carcinoma [I CDX2] BCL2 follicular lymphoma, apoptosis inhibiting protein [I BCL2] Chromogranin A [I CHROGRAN] BCL6 follicle center B-cell [I BCL6] CMYC C-MYC oncoprotein [I CMYC] BER EP4 Epithelial antigen [I BER EP4] Collagen IV, basement membrane protein [I CLLGIV] BRAF [I V600E] Cyclin D1/PRAD1 mantle cell lymphoma [I CYCLIN] Cytokeratin 5/6, squamous, mesothelial [I CK5/6] C Cytokeratin 7, 54kD [I CK7] CA 19-9 pancreas, liver, ovary, lung tumors [I CA19 9] Cytokeratin 7/8 CAM5.2 [I CAM 5.2] CA 125 epitheliod malignancies ovary, breast [I CA125] Cytokeratin 8, 35BH11 [I CK8] Calcitonin [I CALCT] Cytokeratin 8/18, adenocarcinoma [I CK8/18] Caldesmon, smooth muscle [I CALDSM] Cytokeratin 19 [I CK19] Calretinin; Calcium binding protein [I CALRT] Cytokeratin 20 [I CK20] CAM 5.2 Cytokeratin 7/Cytokeratin 8 [I CAM 5.2] Cytokeratin cocktail, PAN (AE1/AE3) [I AE1/AE3] Carcinoembryonic antigen (CEA) [I CEA] Cytokeratin high molecular weight; 34BE12 [I CK HMW] Cathepsin D, breast carcinoma [I CATHD] Cytomegalovirus [I CMV] CD1a cortical thymocyctes, Langerhans cells [I CD1a] -

This Electronic Thesis Or Dissertation Has Been Downloaded from Explore Bristol Research
This electronic thesis or dissertation has been downloaded from Explore Bristol Research, http://research-information.bristol.ac.uk Author: Al Ahdal, Hadil Title: Investigating the role of miR-21 in adult neurogenesis General rights Access to the thesis is subject to the Creative Commons Attribution - NonCommercial-No Derivatives 4.0 International Public License. A copy of this may be found at https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode This license sets out your rights and the restrictions that apply to your access to the thesis so it is important you read this before proceeding. Take down policy Some pages of this thesis may have been removed for copyright restrictions prior to having it been deposited in Explore Bristol Research. However, if you have discovered material within the thesis that you consider to be unlawful e.g. breaches of copyright (either yours or that of a third party) or any other law, including but not limited to those relating to patent, trademark, confidentiality, data protection, obscenity, defamation, libel, then please contact [email protected] and include the following information in your message: •Your contact details •Bibliographic details for the item, including a URL •An outline nature of the complaint Your claim will be investigated and, where appropriate, the item in question will be removed from public view as soon as possible. Investigating the role of miR-21 in adult neurogenesis Hadil Mohammad Al Ahdal Faculty of Health Sciences Bristol Medical School A dissertation submitted to the University of Bristol in accordance with the requirements for award of the degree of Doctor of Philosophy in the Faculty of Health Sciences, Bristol Medical School 64,598 words Abstract MicroRNAs (miRNAs) are a class of small non-coding RNAs that act as post- transcriptional regulators and play important roles in neurodegenerative diseases and brain disorders (Nelson et al. -

Immunohistochemistry Stain Offerings
immunohistochemistry stain offerings TRUSTED PATHOLOGISTS. INVALUABLE ANSWERS.™ MARCHMAY 20172021 www.aruplab.com/ap-ihcaruplab.com/ap-ihc InformationInformation in this brochurein this brochure is current is current as of as May of March 2021. 2017. All content All content is subject is subject to tochange. change. Please contactPlease ARUPcontact ClientARUP Services Client Services at 800-522-2787 at (800) 522-2787 with any with questions any questions or concerns.or concerns. ARUP LABORATORIES As a nonprofit, academic institution of the University of Utah and its Department We believe in of Pathology, ARUP believes in collaborating, sharing and contributing to laboratory science in ways that benefit our clients and their patients. collaborating, Our test menu is one of the broadest in the industry, encompassing more sharing and than 3,000 tests, including highly specialized and esoteric assays. We offer comprehensive testing in the areas of genetics, molecular oncology, pediatrics, contributing pain management, and more. to laboratory ARUP’s clients include many of the nation’s university teaching hospitals and children’s hospitals, as well as multihospital groups, major commercial science in ways laboratories, and group purchasing organizations. We believe that healthcare should be delivered as close to the patient as possible, which is why we support that provide our clients’ efforts to be the principal healthcare provider in the communities they serve by offering highly complex assays and accompanying consultative support. the best value Offering analytics, consulting, and decision support services, ARUP provides for the patient. clients with the utilization management tools necessary to prosper in this time of value-based care. -

Calbindin-D28k and Its Role in Apoptosis: Inhibition of Caspase-3 Activity and Interaction with Pro-Caspase-3 Investigated by In-Situ FRET Microscopy
Dissertation Aus dem Physiologischen Institut Lehrstuhl: Physiologie – Zelluläre Physiologie (Biomedizinisches Zentrum München) der Ludwig-Maximilians-Universität München Vorstand: Prof. Dr. Claudia Veigel Calbindin-D28k and its role in apoptosis: Inhibition of Caspase-3 activity and interaction with Pro-Caspase-3 investigated by in-situ FRET microscopy. Dissertation zum Erwerb des Doktorgrades der Medizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München vorgelegt von Johannes Lohmeier aus Bong Town, Liberia 2018 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. Michael Meyer Prof. Dr. Alexander Faussner Mitberichterstatter: Prof. Dr. Nikolaus Plesnila Prof. Dr. Dr. Bernd Sutor Dekan: Prof. Dr. med. dent. Reinhard Hickel Tag der mündlichen Prüfung: 14.06.2018 Eidesstattliche Versicherung Lohmeier, Johannes Name, Vorname Ich erkläre hiermit an Eides statt, dass ich die vorliegende Dissertation mit dem Thema Calbindin-D28k and its role in apoptosis: Inhibition of Caspase-3 activity and interaction with Pro-Caspase-3 investigated by in-situ FRET microscopy. selbständig verfasst, mich außer der angegebenen keiner weiteren Hilfsmittel bedient und alle Erkenntnisse, die aus dem Schrifttum ganz oder annähernd übernommen sind, als solche kenntlich gemacht und nach ihrer Herkunft unter Bezeichnung der Fundstelle einzeln nachgewiesen habe. Ich erkläre des Weiteren, dass die hier vorgelegte Dissertation nicht in gleicher oder in ähnlicher Form bei einer anderen Stelle zur Erlangung -

Chemical Agent and Antibodies B-Raf Inhibitor RAF265
Supplemental Materials and Methods: Chemical agent and antibodies B-Raf inhibitor RAF265 [5-(2-(5-(trifluromethyl)-1H-imidazol-2-yl)pyridin-4-yloxy)-N-(4-trifluoromethyl)phenyl-1-methyl-1H-benzp{D, }imidazol-2- amine] was kindly provided by Novartis Pharma AG and dissolved in solvent ethanol:propylene glycol:2.5% tween-80 (percentage 6:23:71) for oral delivery to mice by gavage. Antibodies to phospho-ERK1/2 Thr202/Tyr204(4370), phosphoMEK1/2(2338 and 9121)), phospho-cyclin D1(3300), cyclin D1 (2978), PLK1 (4513) BIM (2933), BAX (2772), BCL2 (2876) were from Cell Signaling Technology. Additional antibodies for phospho-ERK1,2 detection for western blot were from Promega (V803A), and Santa Cruz (E-Y, SC7383). Total ERK antibody for western blot analysis was K-23 from Santa Cruz (SC-94). Ki67 antibody (ab833) was from ABCAM, Mcl1 antibody (559027) was from BD Biosciences, Factor VIII antibody was from Dako (A082), CD31 antibody was from Dianova, (DIA310), and Cot antibody was from Santa Cruz Biotechnology (sc-373677). For the cyclin D1 second antibody staining was with an Alexa Fluor 568 donkey anti-rabbit IgG (Invitrogen, A10042) (1:200 dilution). The pMEK1 fluorescence was developed using the Alexa Fluor 488 chicken anti-rabbit IgG second antibody (1:200 dilution).TUNEL staining kits were from Promega (G2350). Mouse Implant Studies: Biopsy tissues were delivered to research laboratory in ice-cold Dulbecco's Modified Eagle Medium (DMEM) buffer solution. As the tissue mass available from each biopsy was limited, we first passaged the biopsy tissue in Balb/c nu/Foxn1 athymic nude mice (6-8 weeks of age and weighing 22-25g, purchased from Harlan Sprague Dawley, USA) to increase the volume of tumor for further implantation. -

A Case of Cerebral Astroblastoma with Rhabdoid Features : a Cytological, Histological, and Immunohistochemical Study
Title A case of cerebral astroblastoma with rhabdoid features : a cytological, histological, and immunohistochemical study Yuzawa, Sayaka; Nishihara, Hiroshi; Tanino, Mishie; Kimura, Taichi; Moriya, Jun; Kamoshima, Yuuta; Nagashima, Author(s) Kazuo; Tanaka, Shinya Brain tumor pathology, 33(1), 63-70 Citation https://doi.org/10.1007/s10014-015-0241-5 Issue Date 2016-01 Doc URL http://hdl.handle.net/2115/63975 Rights The final publication is available at link.springer.com Type article (author version) File Information Astroblastoma_yuzawa_HUSCAP.pdf Instructions for use Hokkaido University Collection of Scholarly and Academic Papers : HUSCAP Case report A case of cerebral astroblastoma with rhabdoid features: a cytological, histological, and immunohistochemical study Sayaka Yuzawa1, Hiroshi Nishihara2, 3, Mishie Tanino1, Taichi Kimura2, 3, Jun Moriya1, Yuuta Kamoshima4, 5, Kazuo Nagashima6, and Shinya Tanaka1, 2. 1Department of Cancer Pathology, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo, 060-8638, Japan. 2Department of Translational Pathology, Hokkaido University Graduate School of Medicine, Sapporo, Japan. 3Translational Research Laboratory, Hokkaido University Hospital, Clinical Research and Medical Innovation Center, Sapporo, Japan. 4Sapporo Azabu Neurosurgical Hospital, Sapporo, Japan. 5Department of Neurosurgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan. 6Higashi Tokushukai Hospital, Sapporo, Japan. Correspondence: Shinya Tanaka Department of Cancer Pathology, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo, 060-8638, Japan. Tel: +81-11-706-5053 Fax: +81-11-706-5902 E-mail: [email protected] 1 Abstract Astroblastoma is a rare neuroepithelial neoplasm of unknown origin, usually occurring in children and young adults. Here we report a case of astroblastoma with uncommon features in an 18-year-old female. -

Impact of Actin Filament Stabilization on Adult Hippocampal and Olfactory Bulb Neurogenesis
The Journal of Neuroscience, March 3, 2010 • 30(9):3419–3431 • 3419 Development/Plasticity/Repair Impact of Actin Filament Stabilization on Adult Hippocampal and Olfactory Bulb Neurogenesis Golo Kronenberg,1,2,5* Karen Gertz,1,2* Tina Baldinger,1 Imke Kirste,5 Sarah Eckart,3 Ferah Yildirim,1 Shengbo Ji,1 Isabella Heuser,5 Helmut Schro¨ck,6 Heide Ho¨rtnagl,4 Reinhard Sohr,4 Pierre Chryso Djoufack,7 Rene´Ju¨ttner,8 Rainer Glass,8 Ingo Przesdzing,1 Jitender Kumar,8 Dorette Freyer,1 Rainer Hellweg,3 Helmut Kettenmann,8 Klaus Benno Fink,7 and Matthias Endres1,2 1Klinik und Poliklinik fu¨r Neurologie, 2Center for Stroke Research Berlin, 3Klinik fu¨r Psychiatrie und Psychotherapie, and 4Institut fu¨r Pharmakologie und Toxikologie, Charite´-Universita¨tsmedizin Berlin, D-10117 Berlin, Germany, 5Klinik und Hochschulambulanz fu¨r Psychiatrie und Psychotherapie, Charite´- Universita¨tsmedizin Berlin, D-14050 Berlin, Germany, 6Institut fu¨r Neurophysiologie, Medizinische Fakulta¨t Mannheim, Universita¨t Heidelberg, D-68167 Mannheim, Germany, 7Institut fu¨r Pharmakologie und Toxikologie, Universita¨t Bonn, D-53113 Bonn, Germany, and 8Max Delbru¨ck Center for Molecular Medicine, D-13092 Berlin, Germany Rearrangement of the actin cytoskeleton is essential for dynamic cellular processes. Decreased actin turnover and rigidity of cytoskeletal structures have been associated with aging and cell death. Gelsolin is a Ca 2ϩ-activated actin-severing protein that is widely expressed throughout the adult mammalian brain. Here, we used gelsolin-deficient (Gsn Ϫ/Ϫ) mice as a model system for actin filament stabiliza- tion. In Gsn Ϫ/Ϫ mice, emigration of newly generated cells from the subventricular zone into the olfactory bulb was slowed.