Alteration of Galectin-3 in Tears of Patients with Dry Eye Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cloning and Expression of Leishmanolysin Gene from Leishmania Major in Primate Cell Lines
J. Sci. I. R. Iran Vol. 12, No. 2, Spring 2001 CLONING AND EXPRESSION OF LEISHMANOLYSIN GENE FROM LEISHMANIA MAJOR IN PRIMATE CELL LINES M. R. Razavi-Deligani1, M. Reza Sadaie2, V. Richinsky3, M. R. Noori- Daloii4, M. Azizi5, A. Amanzadeh6 and M. Assmar1* 1 Department of Parasitology, Pasteur Institute of Iran, Tehran, Islamic Republic of Iran 2 NovoMed Pharmaceuticals, Inc., Germantown, Maryland 20875, USA 3 Engelhardt Institute of Molecular Biology, Russian Academy of Science, Moscow, Russia 4 Department of Medical Genetic, Faculty of Medicine, Tehran University of Medical Sciences, Tehran, Islamic Republic of Iran 5 Department of Biotechnology, Pasteur Institute of Iran, Tehran, Islamic Republic of Iran 6 National Cell Bank, Pasteur Institute of Iran, Tehran, Islamic Republic of Iran Abstract Leishmanolysin is a worldwide disease that is caused by different species of the genus Leishmania. Leishmanolysin, One of the genes expressed by Leishmania, appears to be an ideal candidate for genetic vaccination. In this study, a full length sequence, which encodes Leishmanolysin functionally critical regions (amino acids 100-579), was cloned from a Leishmania strain endemic to Iran. Analysis by restriction enzyme digestion and DNA sequencing in pUC 19 based T-Vector showed that the cloned gene contained the conserved segments of the Leishmanolysin. The identified segments in predicted protein sequence of our clone contained the important domains that have been known to function at the attachment and internalization steps of the parasite life cycle. The cloned gene was expressed in human transformed muscle (Rhabdomyosarcoma TE671/RD) and African green monkey epithelial (COS-7) cell lines under cytomegalovirus (CMV) promoter, and the expressed protein was detected by enzyme linked immunosorbent assay. -

Handbook of Proteolytic Enzymes Second Edition Volume 1 Aspartic and Metallo Peptidases
Handbook of Proteolytic Enzymes Second Edition Volume 1 Aspartic and Metallo Peptidases Alan J. Barrett Neil D. Rawlings J. Fred Woessner Editor biographies xxi Contributors xxiii Preface xxxi Introduction ' Abbreviations xxxvii ASPARTIC PEPTIDASES Introduction 1 Aspartic peptidases and their clans 3 2 Catalytic pathway of aspartic peptidases 12 Clan AA Family Al 3 Pepsin A 19 4 Pepsin B 28 5 Chymosin 29 6 Cathepsin E 33 7 Gastricsin 38 8 Cathepsin D 43 9 Napsin A 52 10 Renin 54 11 Mouse submandibular renin 62 12 Memapsin 1 64 13 Memapsin 2 66 14 Plasmepsins 70 15 Plasmepsin II 73 16 Tick heme-binding aspartic proteinase 76 17 Phytepsin 77 18 Nepenthesin 85 19 Saccharopepsin 87 20 Neurosporapepsin 90 21 Acrocylindropepsin 9 1 22 Aspergillopepsin I 92 23 Penicillopepsin 99 24 Endothiapepsin 104 25 Rhizopuspepsin 108 26 Mucorpepsin 11 1 27 Polyporopepsin 113 28 Candidapepsin 115 29 Candiparapsin 120 30 Canditropsin 123 31 Syncephapepsin 125 32 Barrierpepsin 126 33 Yapsin 1 128 34 Yapsin 2 132 35 Yapsin A 133 36 Pregnancy-associated glycoproteins 135 37 Pepsin F 137 38 Rhodotorulapepsin 139 39 Cladosporopepsin 140 40 Pycnoporopepsin 141 Family A2 and others 41 Human immunodeficiency virus 1 retropepsin 144 42 Human immunodeficiency virus 2 retropepsin 154 43 Simian immunodeficiency virus retropepsin 158 44 Equine infectious anemia virus retropepsin 160 45 Rous sarcoma virus retropepsin and avian myeloblastosis virus retropepsin 163 46 Human T-cell leukemia virus type I (HTLV-I) retropepsin 166 47 Bovine leukemia virus retropepsin 169 48 -

The Kinesin Spindle Protein Inhibitor Filanesib Enhances the Activity of Pomalidomide and Dexamethasone in Multiple Myeloma
Plasma Cell Disorders SUPPLEMENTARY APPENDIX The kinesin spindle protein inhibitor filanesib enhances the activity of pomalidomide and dexamethasone in multiple myeloma Susana Hernández-García, 1 Laura San-Segundo, 1 Lorena González-Méndez, 1 Luis A. Corchete, 1 Irena Misiewicz- Krzeminska, 1,2 Montserrat Martín-Sánchez, 1 Ana-Alicia López-Iglesias, 1 Esperanza Macarena Algarín, 1 Pedro Mogollón, 1 Andrea Díaz-Tejedor, 1 Teresa Paíno, 1 Brian Tunquist, 3 María-Victoria Mateos, 1 Norma C Gutiérrez, 1 Elena Díaz- Rodriguez, 1 Mercedes Garayoa 1* and Enrique M Ocio 1* 1Centro Investigación del Cáncer-IBMCC (CSIC-USAL) and Hospital Universitario-IBSAL, Salamanca, Spain; 2National Medicines Insti - tute, Warsaw, Poland and 3Array BioPharma, Boulder, Colorado, USA *MG and EMO contributed equally to this work ©2017 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2017.168666 Received: March 13, 2017. Accepted: August 29, 2017. Pre-published: August 31, 2017. Correspondence: [email protected] MATERIAL AND METHODS Reagents and drugs. Filanesib (F) was provided by Array BioPharma Inc. (Boulder, CO, USA). Thalidomide (T), lenalidomide (L) and pomalidomide (P) were purchased from Selleckchem (Houston, TX, USA), dexamethasone (D) from Sigma-Aldrich (St Louis, MO, USA) and bortezomib from LC Laboratories (Woburn, MA, USA). Generic chemicals were acquired from Sigma Chemical Co., Roche Biochemicals (Mannheim, Germany), Merck & Co., Inc. (Darmstadt, Germany). MM cell lines, patient samples and cultures. Origin, authentication and in vitro growth conditions of human MM cell lines have already been characterized (17, 18). The study of drug activity in the presence of IL-6, IGF-1 or in co-culture with primary bone marrow mesenchymal stromal cells (BMSCs) or the human mesenchymal stromal cell line (hMSC–TERT) was performed as described previously (19, 20). -

In Silico Characterization of Meloidogyne Genus Nematode Cellulose Binding Proteins Alana Manoela Fraga Menezes1
Vol.62: e19180120, 2019 http://dx.doi.org/10.1590/1678-4324-2019180120 ISSN 1678-4324 Online Edition Article - Agriculture, Agribusiness and Biotechnology In Silico Characterization of Meloidogyne Genus Nematode Cellulose Binding Proteins Alana Manoela Fraga Menezes1 https://orcid.org/0000-0002-7057-8620 Edilton de Albuquerque Cavalcanti Junior1,3 Luiza Suely Semen Martins2,3 Rômulo Maciel de Moraes Filho1,3 https://orcid.org/0000-0003-3988-4379 1Affiliation: Departamento de Agronomia, Universidade Federal Rural de Pernambuco 2Affiliation: Departamento de Biologia, Universidade Federal Rural de Pernambuco 3Affiliation: Programa de Pós-Graduação em Agronomia: Melhoramento Genético de Plantas, Universidade Federal Rural de Pernambuco; Received: 2018.03.05; Accepted: 2019.03.19. HIGHLIGHTS • CBPs are remarkably conserved between Meloidogyne species • CBPs exhibit two to three functional domains related to signal binding and cellulose hydrolase activities Abstract: Root-knot nematodes are a group of endoparasites species that induce the formation of giant cells in the hosts, by which they guarantee their feeding and development. Meloidogyne species infect over 2000 plant species, and are highly destructive, causing damage to many crops around the world. M. enterolobii is considered the most aggressive species in tropical regions, such as Africa and South America. Phytonematodes are able to penetrate and migrate within plant tissues, establishing a sophisticated interaction with their hosts through parasitism factors, which include a series of cell wall degradation enzymes and plant cell modification. Among the parasitism factors documented in the M. enterolobii species, cellulose binding protein (CBP), a nematode excretion protein that appears to be associated with the breakdown of cellulose present in the plant cell wall. -

The Crystal Structure of the Leishmania Major Surface Proteinase Leishmanolysin (Gp63) Edith Schlagenhauf†, Robert Etges‡ and Peter Metcalf*
Research Article 1035 The crystal structure of the Leishmania major surface proteinase leishmanolysin (gp63) Edith Schlagenhauf†, Robert Etges‡ and Peter Metcalf* Background: Despite their medical importance, there is little available Address: EMBL Heidelberg, Biological Structures structural information for the surface antigens of infectious protozoa. Diseases and Biocomputing Programme, Meyerhofstrasse1, Postfach 10.2209, D-69012 Heidelberg, Germany. caused by the protozoan parasite Leishmania are common in many developing countries. Human infection occurs during the bite of infected sandflies, when Present addresses: †Institute of Plant Biology, Leishmania promastigote cells from the insect gut enter the bloodstream. University of Zurich, CH-8008 Zurich, Switzerland Promastigotes in the blood parasitize macrophages, often causing serious and ‡Institut fuer Biomedizinsche Forschung und Beratung (IBFB) GmbH, Arthur-Hoffman Strasse 7, disease. Leishmanolysin is the predominant protein surface antigen of D-04107 Leipzig, Germany. promastigotes, and is assumed to have a key role during infection. Leishmanolysin is a membrane-bound zinc proteinase, active in situ. Similar *Corresponding author. molecules exist in other trypanomastid protozoa. E-mail: [email protected] Key words: crystal structure, gp63, Leishmania, Results: Two crystal forms of leishmanolysin were obtained from protein leishmanolysin purified from promastigote membranes. A single lead derivative in both crystal forms was used to solve the structure. The structure reveals three domains, two Received: 19 February 1998 of which have novel folds. The N-terminal domain has a similar structure to the Revisions requested: 27 March 1998 Revisions received: 30 June 1998 catalytic modules of zinc proteinases. The structure clearly shows that Accepted: 2 July 1998 leishmanolysin is a member of the metzincin class of zinc proteinases. -
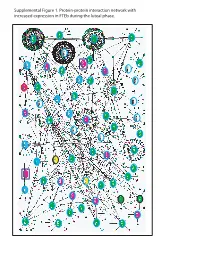
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

Architecture and Function of Metallopeptidase Catalytic Domains
Cerdà-Costa et al. 1 !"#$%&'#&("')*+,)-(+#&%.+).-)/'&*00.1'1&%,*2')#*&*03&%#) ,./*%+2) ) 45"%*)6'",786.2&*)9):;)<*=%'")>./%28?@&$)A)) ) ) B".&'.032%2)C*DE)F'1*"&/'+&).-)G&"(#&("*0)H%.0.I3E)J.0'#(0*")H%.0.I3)K+2&%&(&').-) H*"#'0.+*L)6GK6E)H*"#'0.+*)G#%'+#')B*"ME)N'0%O)H(%0,%+IE)#P)H*0,%"%)?'%O*#L)QR8SQE)T8 UVUSV)H*"#'0.+*)WG1*%+X;) ) A)6.""'21.+,'+#'Y)'8/*%0Y)-OI"Z%D/D;#2%#;'2L)1$.+'Y)W[\]X)^\])USU)QV_L)-*OY)W[\]X)^\]) U\])^`^;) ) a$')*(&$."2)2&*&')&$'3)$*=')+.)#./1'&%+I)-%+*+#%*0)%+&'"'2&;) ) b'3c.",2Y)G&"(#&("*0)D%.#$'/%2&"3L)/'&d%+#%+)#0*+L)#*&*03&%#),./*%+2L)*#&%='82%&')#0'-&L) $3,".03&%#)'+d3/'2L)/*&"%O)/'&*00.1".&'*2'2L)*2&*#%+2L)!F!JL)*,*/*032%+2L)2'""*032%+2L) /'&*00.1".&'*2'L)/'&*00.1".&'%+*2';) ! Cerdà-Costa et al. 2 "#$%&"'%! a$')#0'*=*I').-)1'1&%,')D.+,2)D3)/'&*00.1'1&%,*2'2)WJB2X)%2)'22'+&%*0)-.")0%-';)a$'2')(D%e(%&.(2)'+d3/'2) 1*"&%#%1*&')%+)*00)/*f.")1$32%.0.I%#*0)1".#'22'2L)*+,)2.)&$'%"),'"'I(0*&%.+)0'*,2)&.),%2'*2'2)"*+I%+I)-"./)#*+#'") *+,)/'&*2&*2%2L)%+-0*//*&%.+L)*+,)/%#".D%*0)%+-'#&%.+)&.)+'(".0.I%#*0)%+2(0&2)*+,)#*",%.=*2#(0*"),%2.",'"2;)JB2) #0'*=')&$'%")2(D2&"*&'2)c%&$.(&)#.=*0'+&)%+&'"/',%*&')%+)*)2%+I0'82&'1)"'*#&%.+)%+=.0=%+I)*)2.0='+&)/.0'#(0'L)*) I'+'"*0) D*2'P*#%,L) *+,) *) /.+.8) .") ,%+(#0'*") #*&*03&%#) /'&*0) 2%&';) J.2&) /.+./'&*00%#) JB2) #./1"%2') *) 2$."&) /'&*08D%+,%+I)/.&%-)WNT<<NXL)c$%#$)%+#0(,'2)&c.)/'&*08D%+,%+I)$%2&%,%+'2)*+,)*)I'+'"*0)D*2'P*#%,)I0(&*/*&'L) *+,)&$'3)*"')I".(1',)%+&.)&$')d%+#%+)&"%D').-)JB2;)a$')0*&&'"),%=%,'2)/*%+03)%+&.)&$')I0(d%+#%+)*+,)/'&d%+#%+) #0*+2;) J'&d%+#%+2) #.+2%2&) -

(12) United States Patent (10) Patent No.: US 8,561,811 B2 Bluchel Et Al
USOO8561811 B2 (12) United States Patent (10) Patent No.: US 8,561,811 B2 Bluchel et al. (45) Date of Patent: Oct. 22, 2013 (54) SUBSTRATE FOR IMMOBILIZING (56) References Cited FUNCTIONAL SUBSTANCES AND METHOD FOR PREPARING THE SAME U.S. PATENT DOCUMENTS 3,952,053 A 4, 1976 Brown, Jr. et al. (71) Applicants: Christian Gert Bluchel, Singapore 4.415,663 A 1 1/1983 Symon et al. (SG); Yanmei Wang, Singapore (SG) 4,576,928 A 3, 1986 Tani et al. 4.915,839 A 4, 1990 Marinaccio et al. (72) Inventors: Christian Gert Bluchel, Singapore 6,946,527 B2 9, 2005 Lemke et al. (SG); Yanmei Wang, Singapore (SG) FOREIGN PATENT DOCUMENTS (73) Assignee: Temasek Polytechnic, Singapore (SG) CN 101596422 A 12/2009 JP 2253813 A 10, 1990 (*) Notice: Subject to any disclaimer, the term of this JP 2258006 A 10, 1990 patent is extended or adjusted under 35 WO O2O2585 A2 1, 2002 U.S.C. 154(b) by 0 days. OTHER PUBLICATIONS (21) Appl. No.: 13/837,254 Inaternational Search Report for PCT/SG2011/000069 mailing date (22) Filed: Mar 15, 2013 of Apr. 12, 2011. Suen, Shing-Yi, et al. “Comparison of Ligand Density and Protein (65) Prior Publication Data Adsorption on Dye Affinity Membranes Using Difference Spacer Arms'. Separation Science and Technology, 35:1 (2000), pp. 69-87. US 2013/0210111A1 Aug. 15, 2013 Related U.S. Application Data Primary Examiner — Chester Barry (62) Division of application No. 13/580,055, filed as (74) Attorney, Agent, or Firm — Cantor Colburn LLP application No. -

Structural Features of Angiotensin-I Converting Enzyme Catalytic Sites
Current Topics in Medicinal Chemistry 2004, 4, 403-429 403 Structural Features of Angiotensin-I Converting Enzyme Catalytic Sites: Conformational Studies in Solution, Homology Models and Comparison with Other Zinc Metallopeptidases Georgios A. Spyroulias*,1, Athanassios S. Galanis1, George Pairas1, Evy Manessi-Zoupa2 and Paul Cordopatis*,1 Departments of Pharmacy1 and Chemistry2, University of Patras, GR-26504, Patras, GREECE Abstract: Angiotensin-I Converting Enzyme (ACE) is a Zinc Metallopeptidase of which the three-dimensional stucture was unknown until recently, when the Xray structure of testis isoform (C-terminal domain of somatic) was determined. ACE plays an important role in the regulation of blood pressure due to its action in the frame of the Renin-Angiotensin System. Efforts for the specific inhibition of the catalytic function of this enzyme have been made on the basis of the X- ray structures of other enzymes with analogous efficacy in the hydrolytic cleavage of peptide substrate terminal fragments. Angiotensin-I Converting Enzyme bears the sequence and topology characteristics of the well-known gluzincins, a sub-family of zincins metallopeptidases and these similarities are exploited in order to reveal common structural elements among these enzymes. 3D homology models are also built using the X-ray structure of Thermolysin as template and peptide models that represent the amino acid sequence of the ACE’s two catalytic, zinc-containing sites are designed and synthesized. Conformational analysis of the zinc-free and zinc-bound peptides through high resolution 1H NMR Spectroscopy provides new insights into the solution structure of ACE catalytic centers. Structural properties of these peptides could provide valuable information towards the design and preparation of new potent ACE inhibitors. -

Drugs for the Future: Infectious Diseases Antimicrobial Drug Discovery : Challenges and Perspectives
DFID-2014 International Conference on Drugs for the Future: Infectious Diseases Antimicrobial Drug Discovery : Challenges and Perspectives DFID-2014 March 27 - 28, 2014 Souvenir National Institute of Pharmaceutical Education and Research (NIPER) Dept. of Pharmaceuticals, Ministry of Chemicals & Fertilizers, Govt. of India Balanagar, Hyderabad - 500 037, A.P, India 1 DFID 2014 Chairman: Dr Ahmed Kamal Convener: Dr Srinivas Nanduri Advisory Committee: Prof N. Satyanarayana, Dr R. Srinivas, Dr Y.V.D. Nageshwar Registrations Programme & Floor Administrative secretaries Dr. Y.V. Madhavi management Mrs. M. Swapna Devi Dr. M. Mallika Dr. Bathini Nagendra babu Mrs. Sai Vishali Dr. D Sujatha Dr. Ashutosh kumar Dr. VGM. Naidu Ms. B Laxmi Dr M.V.Rao Logistics Dr. D Swapna Dr. Shraddha Chowdhary Dr. Arifuddin Mr. Sujendra swami Dr G Srinivas Catering Mrs. Sujatha Rao Abstracts & Posters Dr. V.G.M. Naidu Mr. Venky Dr. Ashutosh kumar Dr. Gananadhamu Mr. Praveen Dr. Wahid khan Dr. Satheesh kumar Ms. Rama Devi Dr. G Chandraiah Mr. Ch.Naveen Mr Mahesh Dr. Nalini shastri Mr Manohar Dr. N Shankaraiah Administration, Finance & Mr. Rajesh Jha Dr. P.K. Dubey Purchase Mr. Narsaiah Mr. Venu gopal Shri Y. Ramakrishna (COA, IICT) Mr. D. Krishna Kishore Transportation & Smt. N. Padma (COFA , IICT) Ms. U. Jayalakshmi Accommodation Shri R. K. Rao (COSP, IICT) Mr. G. Chandrakanth Dr. N. Shankaraiah Shri Badarinath Mr. G. C. Brahma Reddy Dr. Gananadhamu Shri M.S.N.Murthy Mr. Ch. Veerrabhadra Swamy Dr. M.V.N kumar Talluri Ms. B. Naga Priya Ms. N. Haritha Dr. S. Sunitha Printing & Publicity Dr. Satheesh kumar Mr. K. -

Peptide Sequence
Peptide Sequence Annotation AADHDG CAS-L1 AAEAISDA M10.005-stromelysin 1 (MMP-3) AAEHDG CAS-L2 AAEYGAEA A01.009-cathepsin D AAGAMFLE M10.007-stromelysin 3 (MMP-11) AAQNASMW A06.001-nodavirus endopeptidase AASGFASP M04.003-vibriolysin ADAHDG CAS-L3 ADAPKGGG M02.006-angiotensin-converting enzyme 2 ADATDG CAS-L5 ADAVMDNP A01.009-cathepsin D ADDPDG CAS-21 ADEPDG CAS-L11 ADETDG CAS-22 ADEVDG CAS-23 ADGKKPSS S01.233-plasmin AEALERMF A01.009-cathepsin D AEEQGVTD C03.007-rhinovirus picornain 3C AETFYVDG A02.001-HIV-1 retropepsin AETWYIDG A02.007-feline immunodeficiency virus retropepsin AFAHDG CAS-L24 AFATDG CAS-25 AFDHDG CAS-L26 AFDTDG CAS-27 AFEHDG CAS-28 AFETDG CAS-29 AFGHDG CAS-30 AFGTDG CAS-31 AFQHDG CAS-32 AFQTDG CAS-33 AFSHDG CAS-L34 AFSTDG CAS-35 AFTHDG CAS-L36 AGERGFFY Insulin B-chain AGLQRGGG M14.004-carboxypeptidase N AGSHLVEA Insulin B-chain AIDIDG CAS-L37 AIDPDG CAS-38 AIDTDG CAS-39 AIDVDG CAS-L40 AIEHDG CAS-L41 AIEIDG CAS-L42 AIENDG CAS-43 AIEPDG CAS-44 AIEQDG CAS-45 AIESDG CAS-46 AIETDG CAS-47 AIEVDG CAS-48 AIFQGPID C03.007-rhinovirus picornain 3C AIGHDG CAS-49 AIGNDG CAS-L50 AIGPDG CAS-L51 AIGQDG CAS-52 AIGSDG CAS-53 AIGTDG CAS-54 AIPMSIPP M10.051-serralysin AISHDG CAS-L55 AISNDG CAS-L56 AISPDG CAS-57 AISQDG CAS-58 AISSDG CAS-59 AISTDG CAS-L60 AKQRAKRD S08.071-furin AKRQGLPV C03.007-rhinovirus picornain 3C AKRRAKRD S08.071-furin AKRRTKRD S08.071-furin ALAALAKK M11.001-gametolysin ALDIDG CAS-L61 ALDPDG CAS-62 ALDTDG CAS-63 ALDVDG CAS-L64 ALEIDG CAS-L65 ALEPDG CAS-L66 ALETDG CAS-67 ALEVDG CAS-68 ALFQGPLQ C03.001-poliovirus-type picornain -

Multiple Architectures and Mechanisms of Latency in Metallopeptidase Zymogens
Arolas et al. 1 Multiple architectures and mechanisms of latency in metallopeptidase zymogens Joan L. Arolas a,1, Theodoros Goulas 1, Anna Cuppari and F. Xavier Gomis-Rüth * Proteolysis Laboratory; Structural Biology Unit ("María-de-Maeztu" Unit of Excellence); Molecular Biology Institute of Barcelona (CSIC); Barcelona Science Park; c/Baldiri Reixac, 15-21; 08028 Barcelona (Catalonia, Spain). a Present address: Max F. Perutz Laboratories; University of Vienna; Campus Vienna Biocenter 5; 1030 Vienna (Austria). * Corresponding author: Tel.:(+34) 934 020 186; E-mail: [email protected]. 1 These authors contributed equally and share first authorship. ABSTRACT Metallopeptidases cleave polypeptides bound in the active-site cleft of catalytic domains through a general base/acid- mechanism. This involves a solvent molecule bound to a catalytic zinc and general regulation of the mechanism through zymogen-based latency. Sixty reported structures from eleven metallopeptidase families reveal that pro-segments, mostly N-terminally of the catalytic domain, block the cleft regardless of their size. Pro-segments may be peptides (5-14 residues), which are only structured within the zymogens, or large moieties (<227 residues) of one or two folded domains. While some pro-segments globally shield the catalytic domain through a few contacts, others specifically run across the cleft in the same or opposite direction of a substrate, making numerous interactions. Some pro-segments block the zinc by replacing the solvent with particular side chains, others use terminal α-amino or carboxylate groups. Overall, metallopeptidase zymogens employ disparate mechanisms that diverge even within families, which supports that latency is less conserved than catalysis. CONTENTS 1.