Imaging of Sports Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -

Plantar Fascia-Specific Stretching Program for Plantar Fasciitis
Plantar Fascia-Specific Stretching Program For Plantar Fasciitis Plantar Fascia Stretching Exercise 1. Cross your affected leg over your other leg. 2. Using the hand on your affected side, take hold of your affected foot and pull your toes back towards shin. This creates tension/stretch in the arch of the foot/plantar fascia. 3. Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string. 4. Hold the stretch for a count of 10. A set is 10 repetitions. 5. Perform at least 3 sets of stretches per day. You cannot perform the stretch too often. The most important times to stretch are before taking the first step in the morning and before standing after a period of prolonged sitting. Plantar Fascia Stretching Exercise 1 2 3 4 URMC Orthopaedics º 4901 Lac de Ville Boulevard º Building D º Rochester, NY 14618 º 585-275-5321 www.ortho.urmc.edu Over, Please Anti-inflammatory Medicine Anti-inflammatory medicine will help decrease the inflammation in the arch and heel of your foot. These include: Advil®, Motrin®, Ibuprofen, and Aleve®. 1. Use the medication as directed on the package. If you tolerate it well, take it daily for 2 weeks then discontinue for 1 week. If symptoms worsen or return, then resume medicine for 2 weeks, then stop. 2. You should eat when taking these medications, as they can be hard on your stomach. Arch Support 1. -

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

The Pathomechanics of Plantar Fasciitis
Sports Med 2006; 36 (7): 585-611 REVIEW ARTICLE 0112-1642/06/0007-0585/$39.95/0 2006 Adis Data Information BV. All rights reserved. The Pathomechanics of Plantar Fasciitis Scott C. Wearing,1 James E. Smeathers,1 Stephen R. Urry,1 Ewald M. Hennig2 and Andrew P. Hills1 1 Institute of Health and Biomedical Innovation, Queensland University of Technology, Kelvin Grove, Queensland, Australia 2 Biomechanik Labor, University Duisburg-Essen, Essen, Germany Contents Abstract ....................................................................................585 1. Anatomy of the Plantar Fascia ............................................................586 1.1 Gross Anatomy of the Plantar Fascia...................................................586 1.2 Histological Anatomy of the Plantar Fascia .............................................589 1.2.1 Neuroanatomy ................................................................590 1.2.2 Microcirculation ...............................................................590 1.2.3 The Enthesis ...................................................................590 2. Mechanical Properties of the Plantar Fascia ................................................592 2.1 Structural Properties ..................................................................593 2.2 Material Properties ...................................................................593 3. Mechanical Function of the Plantar Fascia .................................................594 3.1 Quasistatic Models of Plantar Fascial Function ..........................................594 -

SLAP Repairs Versus Biceps Tenodesis in Athletes 15 Min Power Points
SLAP Repairs Versus Biceps Tenodesis in Athletes 15 min Power Points • Not all SLAP tears need surgery • Preservation of Native Anatomy GOAL • Not all labral repairs are equal • Kinetic chain MUST be addressed Power Points • Biceps DOES have a function • Tenodesis has consequences • Tenodesis relieves pain reliably BUT……long term effects uncertain ‘SLAPAHOLIC’ T. Romeo • One who fixes EVERY SLAP TEAR and anything that remotely looks like one! Not all SLAP Tears Need Surgery • SLAP tears way overdiagnosed • Beware of positive imaging study - negative exam • Slight labral separation may allow thrower to ‘get the slot’ MRI May OVERDIAGNOSE • Specificity ranges from 63% to 91% MRI and Anatomic Variants • Meniscoid labrum • Buford complex • Cord like MGHL • Age related attritional tear • ALL CAN LOOK LIKE SLAP TEARS ON MRI!! Meniscoid Labrum ‘Buford’ Complex Labral Tears are Part of the Aging Process! Pfahler et al JSES 2003 MANY LABRAL TEARS RESPOND TO REHAB!!!! Nonoperative Treatment of Superior Labrum Anterior Posterior Tears Improvements in Pain, Function, and Quality of Life Edwards et al • Approx. 50% of non operatively treated patients avoided surgery! Scapular strengthening, posterior capsular stretching Overtreat >>>> NIGHTMARE Make Sure History Consistent with SLAP “event” • Sudden loss of velocity (dead arm) • Large increase in pain • “mechanical symptoms” usually present • Rehab no longer effective Exam Hold Key!!! • Load Shift • Passive Distraction test • Mayo Shear • O’Brien’ Test (anterior) • Kim test • Relocation Test Mayo Shear -
THE MANAGEMENT of SLAP INJURIES in the OVERHEAD ATHLETE Michael G
THE MANAGEMENT of SLAP INJURIES in the OVERHEAD ATHLETE Michael G. Ciccotti, MD The Everett J. and Marian Gordon Professor of Orthopaedics Chief, Division of Sports Medicine Rothman Institute Thomas Jefferson University Head Team Physician, Philadelphia Phillies Faculty Disclosure Consultant – Stryker Endoscopy Consultant – Venture MD Research Support – Arthrex Board/Committee Membership – Orthopaedic Learning Center BOD MLB Medical Advisory Committee MLB Elbow Research Study Group AOSSM Fellowship Committee Rothman Institute of Orthopaedics at Thomas Jefferson University Shoulder Injury in the Athlete History Exam 27 y.o. RHD MLB 30 deg. less ABD, FF pitcher 25 deg. less INT ROT Chronic, progressive + Hawkin’s Test right shoulder pain + O’Brien’s & DLS while throwing Tests Worsened acutely + mild-mod supraspinatus Pain is deep and post weakness Unable to throw Rothman Institute of Orthopaedics at Thomas Jefferson University ShoulderDiagnosis: Injury SLAP in the Athlete Tear Rothman Institute of Orthopaedics at Thomas Jefferson University Superior Labrum is Important for the Overhead Athlete! Biceps attachment site Deepens glenoid Distributes contact pressure between humerus & glenoid Harryman, 1992 – Washer Effect Pagnani, 1995 Lee, 2005 Attachment site for glenohumeral Veeger, 2007 ligaments & capsule Lee, 2008 Kibler, 2011 Pressure sensor for proprioception Rothman Institute of Orthopaedics at Thomas Jefferson University Predictable Series of Events in Throwers Progressive Osseous changes Scapular and Cuff -
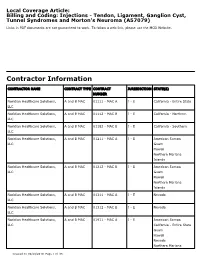
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Rehab for Bicep Tendon Problems
Rehabilitation for Biceps Tendon Disorders and SLAP Lesions 117 capsulitis will suffer long-term ROM defi cits that may arthroscopic release (5); or MUA and arthroscopic last more than 10 years. Clarke et al. (1975) reported hydrodistension (20). During the long-term follow-up that 42% of patients continued to have motion loss (mean 52.3 months) 59% of patients reported hav- after 6 years of follow-up. Likewise, Schaffer et al. ing normal or near-normal shoulders, 35% reported (1992) reported that 50% of patients managed non- persistent mild/moderate symptoms, and 6% still had operatively remained symptomatic during their long- severe symptoms. Persistent symptoms were reported term follow-up, which occurred 2–11 years after their as mild in 94% of patients, with pain being the most initial visit (mean = 7 years). Of these patients, 60% common complaint. Only 6% of patients complained had a measurable restriction of shoulder motion. of severe pain and/or functional loss. Patients with External rotation was the most chronically restricted the most severe symptoms at condition onset had the movement, providing further evidence that the rotator worst long-term prognosis. In general, patients with interval and coracohumeral ligament are particularly comorbid factors, particularly diabetes, hyperthyroid- affected by adhesive capsulitis. Hand et al. (2008) ism, hypothyroidism, hypoadrenalism, Parkinson's tracked outcomes in 269 shoulders affected by pri- disease, cardiac disease, pulmonary disease, or cere- mary adhesive capsulitis who received no treatment brovascular accident, tend to have more severe and (95); physical therapy (55); steroid injection (139); longer lasting symptoms and tend to be more recalci- manipulation under anesthesia (MUA) (5); MUA and trant to treatment. -

Conditions Related to Inflammatory Arthritis
Conditions Related to Inflammatory Arthritis There are many conditions related to inflammatory arthritis. Some exhibit symptoms similar to those of inflammatory arthritis, some are autoimmune disorders that result from inflammatory arthritis, and some occur in conjunction with inflammatory arthritis. Related conditions are listed for information purposes only. • Adhesive capsulitis – also known as “frozen shoulder,” the connective tissue surrounding the joint becomes stiff and inflamed causing extreme pain and greatly restricting movement. • Adult onset Still’s disease – a form of arthritis characterized by high spiking fevers and a salmon- colored rash. Still’s disease is more common in children. • Caplan’s syndrome – an inflammation and scarring of the lungs in people with rheumatoid arthritis who have exposure to coal dust, as in a mine. • Celiac disease – an autoimmune disorder of the small intestine that causes malabsorption of nutrients and can eventually cause osteopenia or osteoporosis. • Dermatomyositis – a connective tissue disease characterized by inflammation of the muscles and the skin. The condition is believed to be caused either by viral infection or an autoimmune reaction. • Diabetic finger sclerosis – a complication of diabetes, causing a hardening of the skin and connective tissue in the fingers, thus causing stiffness. • Duchenne muscular dystrophy – one of the most prevalent types of muscular dystrophy, characterized by rapid muscle degeneration. • Dupuytren’s contracture – an abnormal thickening of tissues in the palm and fingers that can cause the fingers to curl. • Eosinophilic fasciitis (Shulman’s syndrome) – a condition in which the muscle tissue underneath the skin becomes swollen and thick. People with eosinophilic fasciitis have a buildup of eosinophils—a type of white blood cell—in the affected tissue. -

A+ Mobile Ultrasound Services LLC Seattle, WA 206-799-3301 [email protected] Musculoskeletal (MSK)
A+ Mobile Ultrasound Services LLC Seattle, WA 206-799-3301 [email protected] Musculoskeletal (MSK) www.APlusUltrasound.com Shoulder Hip • Rotator Cuff Tear/Tedonosis • Bowel Hernia • Biceps Tendon Tear • Sports Hernia • Tendinitis/Tenosynovitis/Subluxation • Snapping Hip Syndrome • Shoulder Impingement • Effusion • AC joint separation • Gluteal or thigh muscle injury • Fluid Collections – Bursitis / Effusion Knee Elbow • MCL / LCL Injury • Tennis Elbow – Lateral Epicondylitis • Iliotibial Band Syndrome • Golfer’s Elbow – Medial Epicondylitis • Jumper’s Knee – Patellar Tendon Injury • Biceps Tendon Insertion • Lateral, Medial or Posterior Meniscus Tear • Ulnar Nerve Entrapment • Runner’s knee • (Cubital Tunnel Syndrome) • Fluid collection – Bursitis / Effusion / Baker’s • Ulnar Collateral Ligament (UCL) Injury Cyst • Triceps Tendon Tear/Tendonosis Ankle/Foot • Fluid Collection – Bursitis / Effusion • Achilles’ Tendon Tear/Tendinitis Wrist • Tibial Tendon Tear/Tendinitis/Tenosynovitis • Medial Nerve Entrapment • Peroneal • Carpal Tunnel Syndrome Tear/Tendinitis/Tenosynovitis/Subluxation • Extensor Tendonosis/Tenosynovitis • Ankle Sprain – Ligament Injury (ATFL) • De Quervain’s Syndrome • High Ankle Sprain – Tibiofibular Ligament Tear • Flexor Tendonosis/Tenosynovitis • Tibial Nerve Entrapment Hand/Finger • Fluid Collection – Bursitis / Effusion • Trigger Finger • Plantar Fasciitis • Avulsion • Morton’s Neuroma • Fracture • Turf Toe MSK Jaw and Neck Ultrasound MSK Extremity – Non Joint • Neck Pain • Muscle Sprain/Tear • Whiplash -

Advice and Exercises for Patients with Plantar Fasciitis
Advice and exercises for patients with plantar fasciitis This leaflet provides management advice and exercises for people diagnosed with plantar fasciitis, a condition causing pain in the heel, sole and /or arch of the foot. Structures of the foot The plantar fascia is a sheet or broad band of fibrous tissue that runs along the bottom of the foot. This tissue connects the heel to the base of the toes. Under normal circumstances, the plantar fascia supports the arch of the foot and acts as a shock absorbing “bow string” within the arch of the foot. With weight bearing, the foot flattens and the plantar fascia stretches, then springing you forward ready for the next step. While walking, the stresses placed on the foot can be one and a quarter times your body weight (this increases to two and three quarter times your body weight when running). Unsurprisingly then, that heel pain is common. If tension on this “bowstring” becomes too great, irritation or inflammation can occur causing pain. What is plantar fasciitis? Plantar fasciitis is a relatively common foot problem affecting up to 10-15% of the population. It can occur at any age. It is sometimes known as “policeman’s heel”. When placed under too much stress due to abnormal loading, the plantar fascia stretches causing micro tearing and degeneration of the tissue. It can lead to pain in the heel, across the sole of the foot and sometimes into the arch area of the foot too. These micro tears repair with scar tissue, which is less flexible than the fascia and can cause the problem to persist for many months. -

Plantar Fasciitis
Recent Advances in Orthotic Therapy for Plantar Fasciitis An Evidence Based Approach Lawrence Z. Huppin, D.P.M. Assistant Clinical Professor, Western University of Health Sciences, College of Podiatric Medicine Disclosures I disclose the following financial relationships with commercial entities that produce health care related products and services relevant to the content of this lecture: ◦ Employee (Medical Director) of ProLab Orthotics, manufacturer of foot orthoses Our Goals . Review Three Studies that Help Optimize Clinical Outcome of Custom Foot Orthoses Used to Treat Plantar Fasciitis • Cause of Plantar Fascial Tension • Forefoot Wedging Effect on Plantar Fascial Tension • Arch Contour Effect on Plantar Fascial Tension . Develop a “pathology specific” orthosis prescription to most effectively treat plantar fasciitis . Offloading Excessive Fascia Tension is Goal of Orthotic Therapy . What Causes Tension? Tissue Stress Theory McPoil, Hunt. Evaluation and Management of Foot and Ankle Disorders: Present Problems and Future Directions. Journal of Orthopaedic & Sports Physical Therapy, 1995 Effect of STJ Pronation on PF Strain . Cannot by itself cause strain of plantar fascia . Can only increase plantar fascia strain via the MTJ • (inversion of the forefoot on the rearfoot) Scherer. “Heel Pain Syndrome: Pathomechanics and Non-surgical Treatment. JAPMA 1991 Effect of Forefoot Inversion on Plantar Fascial Strain 73 patients with 118 painful heels 91% had foot deformity compensated by supination of long axis of MTJ Out of 118 painful heels 63 had forefoot valgus 33 had everted rearfoot 20 had plantarflexed first ray Scherer 1991 What foot types supinate the MTJ? . 47% forefoot valgus . 24% everted heel . 20% plantarflexed first ray Scherer 1991 What foot types supinate the MTJ? .