Improving Breast Cancer Sensitivity to Paclitaxel by Increasing Aneuploidy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kinesin Family Member 18B Regulates the Proliferation and Invasion Of
Wu et al. Cell Death and Disease (2021) 12:302 https://doi.org/10.1038/s41419-021-03582-2 Cell Death & Disease ARTICLE Open Access Kinesin family member 18B regulates the proliferation and invasion of human prostate cancer cells Yu-Peng Wu 1,Zhi-BinKe 1, Wen-Cai Zheng 1, Ye-Hui Chen 1,Jun-MingZhu 1,FeiLin 1,Xiao-DongLi 1, Shao-Hao Chen 1,HaiCai 1, Qing-Shui Zheng 1, Yong Wei 1, Xue-Yi Xue 1 and Ning Xu 1 Abstract Expression of kinesin family member 18B (KIF18B), an ATPase with key roles in cell division, is deregulated in many cancers, but its involvement in prostate cancer (PCa) is unclear. Here, we investigated the expression and function of KIF18B in human PCa specimens and cell lines using bioinformatics analyses, immunohistochemical and immunofluorescence microscopy, and RT-qPCR and western blot analyses. KIF18B was overexpressed in PCa specimens compared with paracancerous tissues and was associated with poorer disease-free survival. In vitro, KIF18B knockdown in PCa cell lines promoted cell proliferation, migration, and invasion, and inhibited cell apoptosis, while KIF18B overexpression had the opposite effects. In a mouse xenograft model, KIF18B overexpression accelerated and promoted the growth of PCa tumors. Bioinformatics analysis of control and KIF18B-overexpressing PCa cells showed that genes involved in the PI3K–AKT–mTOR signaling pathway were significantly enriched among the differentially expressed genes. Consistent with this observation, we found that KIF18B overexpression activates the PI3K–AKT–mTOR signaling pathway in PCa cells both in vitro and in vivo. Collectively, our results suggest that KIF18B plays a crucial role – – 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; in PCa via activation of the PI3K AKT mTOR signaling pathway, and raise the possibility that KIF18B could have utility as a novel biomarker for PCa. -
0.5) in Stat3∆/∆ Compared with Stat3flox/Flox
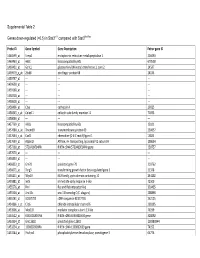
Supplemental Table 2 Genes down-regulated (<0.5) in Stat3∆/∆ compared with Stat3flox/flox Probe ID Gene Symbol Gene Description Entrez gene ID 1460599_at Ermp1 endoplasmic reticulum metallopeptidase 1 226090 1460463_at H60c histocompatibility 60c 670558 1460431_at Gcnt1 glucosaminyl (N-acetyl) transferase 1, core 2 14537 1459979_x_at Zfp68 zinc finger protein 68 24135 1459747_at --- --- --- 1459608_at --- --- --- 1459168_at --- --- --- 1458718_at --- --- --- 1458618_at --- --- --- 1458466_at Ctsa cathepsin A 19025 1458345_s_at Colec11 collectin sub-family member 11 71693 1458046_at --- --- --- 1457769_at H60a histocompatibility 60a 15101 1457680_a_at Tmem69 transmembrane protein 69 230657 1457644_s_at Cxcl1 chemokine (C-X-C motif) ligand 1 14825 1457639_at Atp6v1h ATPase, H+ transporting, lysosomal V1 subunit H 108664 1457260_at 5730409E04Rik RIKEN cDNA 5730409E04Rik gene 230757 1457070_at --- --- --- 1456893_at --- --- --- 1456823_at Gm70 predicted gene 70 210762 1456671_at Tbrg3 transforming growth factor beta regulated gene 3 21378 1456211_at Nlrp10 NLR family, pyrin domain containing 10 244202 1455881_at Ier5l immediate early response 5-like 72500 1455576_at Rinl Ras and Rab interactor-like 320435 1455304_at Unc13c unc-13 homolog C (C. elegans) 208898 1455241_at BC037703 cDNA sequence BC037703 242125 1454866_s_at Clic6 chloride intracellular channel 6 209195 1453906_at Med13l mediator complex subunit 13-like 76199 1453522_at 6530401N04Rik RIKEN cDNA 6530401N04 gene 328092 1453354_at Gm11602 predicted gene 11602 100380944 1453234_at -

Differential Gene Expression in Oligodendrocyte Progenitor Cells, Oligodendrocytes and Type II Astrocytes
Tohoku J. Exp. Med., 2011,Differential 223, 161-176 Gene Expression in OPCs, Oligodendrocytes and Type II Astrocytes 161 Differential Gene Expression in Oligodendrocyte Progenitor Cells, Oligodendrocytes and Type II Astrocytes Jian-Guo Hu,1,2,* Yan-Xia Wang,3,* Jian-Sheng Zhou,2 Chang-Jie Chen,4 Feng-Chao Wang,1 Xing-Wu Li1 and He-Zuo Lü1,2 1Department of Clinical Laboratory Science, The First Affiliated Hospital of Bengbu Medical College, Bengbu, P.R. China 2Anhui Key Laboratory of Tissue Transplantation, Bengbu Medical College, Bengbu, P.R. China 3Department of Neurobiology, Shanghai Jiaotong University School of Medicine, Shanghai, P.R. China 4Department of Laboratory Medicine, Bengbu Medical College, Bengbu, P.R. China Oligodendrocyte precursor cells (OPCs) are bipotential progenitor cells that can differentiate into myelin-forming oligodendrocytes or functionally undetermined type II astrocytes. Transplantation of OPCs is an attractive therapy for demyelinating diseases. However, due to their bipotential differentiation potential, the majority of OPCs differentiate into astrocytes at transplanted sites. It is therefore important to understand the molecular mechanisms that regulate the transition from OPCs to oligodendrocytes or astrocytes. In this study, we isolated OPCs from the spinal cords of rat embryos (16 days old) and induced them to differentiate into oligodendrocytes or type II astrocytes in the absence or presence of 10% fetal bovine serum, respectively. RNAs were extracted from each cell population and hybridized to GeneChip with 28,700 rat genes. Using the criterion of fold change > 4 in the expression level, we identified 83 genes that were up-regulated and 89 genes that were down-regulated in oligodendrocytes, and 92 genes that were up-regulated and 86 that were down-regulated in type II astrocytes compared with OPCs. -

Microrna-7-5P Mediates the Signaling of Hepatocyte Growth
www.nature.com/scientificreports OPEN MicroRNA-7-5p mediates the signaling of hepatocyte growth factor to suppress oncogenes in the Received: 30 August 2017 Accepted: 2 November 2017 MCF-10A mammary epithelial cell Published: xx xx xxxx Dawoon Jeong1, Juyeon Ham1, Sungbin Park1, Seungyeon Lee 1, Hyunkyung Lee1, Han-Sung Kang2 & Sun Jung Kim1 MicroRNA-7 (miR-7) is a non-coding RNA of 23-nucleotides that has been shown to act as a tumor suppressor in various cancers including breast cancer. Although there have been copious studies on the action mechanisms of miR-7, little is known about how the miR is controlled in the mammary cell. In this study, we performed a genome-wide expression analysis in miR-7-transfected MCF-10A breast cell line to explore the upstream regulators of miR-7. Analysis of the dysregulated target gene pool predicted hepatocyte growth factor (HGF) as the most plausible upstream regulator of miR-7. MiR-7 was upregulated in MCF-10A cells by HGF, and subsequently downregulated upon treatment with siRNA against HGF. However, the expression of HGF did not signifcantly change through either an upregulation or downregulation of miR-7 expression, suggesting that HGF acts upstream of miR-7. In addition, the target genes of miR-7, such as EGFR, KLF4, FAK, PAK1 and SET8, which are all known oncogenes, were downregulated in HGF-treated MCF-10A; in contrast, knocking down HGF recovered their expression. These results indicate that miR-7 mediates the activity of HGF to suppress oncogenic proteins, which inhibits the development of normal cells, at least MCF-10A, into cancerous cells. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Impaired Angiogenesis and Tumor Development by Inhibition of the Mitotic Kinesin Eg5
Oncotarget, December, Vol.4, No 12 Impaired angiogenesis and tumor development by inhibition of the mitotic kinesin Eg5 Prisca Exertier1,2, Sophie Javerzat1,2, Baigang Wang3,8, Mélanie Franco1,2, John Herbert4, Natalia Platonova1,2, Marie Winandy5, Nadège Pujol1,2, Olivier Nivelles6, Sandra Ormenese7, Virginie Godard1,2, Jürgen Becker8, Roy Bicknell4, Raphael Pineau9, Jörg Wilting8*, Andreas Bikfalvi1,2*, Martin Hagedorn1,2* 1 Univ. Bordeaux, LAMC, UMR 1029, F-33405 Talence, France 2 INSERM, LAMC, UMR 1029, F-33405 Talence, France 3 Ruhr-Universität Bochum, Medizinische Fakultät; Abt. f. Anatomie und Embryologie, D-44780 Bochum, Germany 4 Molecular Angiogenesis Group, Institute of Biomedical Research, Univ Birmingham, Medical School, Edgbaston, Birmingham, UK 5 GIGA, Zebrafish Facility, Tour B34, Université de Liège, Belgium 6 GIGA, Unité de Biologie Moléculaire et Génie Génétique, Tour B34, Université de Liège, Belgium 7 GIGA, Imaging and Flow Cytometry Facility, Tour B34, Université de Liege, Belgium 8 Zentrum Anatomie, Abteilung Anatomie und Zellbiologie, Georg-August-Universität Goettingen, Germany 9 Animalerie mutualisée, University of Bordeaux I, Talence, France * Co-PIs Correspondence to: Martin Hagedorn, email: [email protected] Keywords: Angiogenesis, Eg5 kinesin, Mklp2 kinesin, VEGF, ispinesib Received: October 11, 2013 Accepted: October 24, 2013 Published: October 26, 2013 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT: Kinesin motor proteins exert essential cellular functions in all eukaryotes. They control mitosis, migration and intracellular transport through interaction with microtubules. Small molecule inhibitors of the mitotic kinesin KiF11/Eg5 are a promising new class of anti-neoplastic agents currently evaluated in clinical cancer trials for solid tumors and hematological malignancies. -

Molecular Features of Triple Negative Breast Cancer Cells by Genome-Wide Gene Expression Profiling Analysis
478 INTERNATIONAL JOURNAL OF ONCOLOGY 42: 478-506, 2013 Molecular features of triple negative breast cancer cells by genome-wide gene expression profiling analysis MASATO KOMATSU1,2*, TETSURO YOSHIMARU1*, TAISUKE MATSUO1, KAZUMA KIYOTANI1, YASUO MIYOSHI3, TOSHIHITO TANAHASHI4, KAZUHITO ROKUTAN4, RUI YAMAGUCHI5, AYUMU SAITO6, SEIYA IMOTO6, SATORU MIYANO6, YUSUKE NAKAMURA7, MITSUNORI SASA8, MITSUO SHIMADA2 and TOYOMASA KATAGIRI1 1Division of Genome Medicine, Institute for Genome Research, The University of Tokushima; 2Department of Digestive and Transplantation Surgery, The University of Tokushima Graduate School; 3Department of Surgery, Division of Breast and Endocrine Surgery, Hyogo College of Medicine, Hyogo 663-8501; 4Department of Stress Science, Institute of Health Biosciences, The University of Tokushima Graduate School, Tokushima 770-8503; Laboratories of 5Sequence Analysis, 6DNA Information Analysis and 7Molecular Medicine, Human Genome Center, Institute of Medical Science, The University of Tokyo, Tokyo 108-8639; 8Tokushima Breast Care Clinic, Tokushima 770-0052, Japan Received September 22, 2012; Accepted November 6, 2012 DOI: 10.3892/ijo.2012.1744 Abstract. Triple negative breast cancer (TNBC) has a poor carcinogenesis of TNBC and could contribute to the develop- outcome due to the lack of beneficial therapeutic targets. To ment of molecular targets as a treatment for TNBC patients. clarify the molecular mechanisms involved in the carcino- genesis of TNBC and to identify target molecules for novel Introduction anticancer drugs, we analyzed the gene expression profiles of 30 TNBCs as well as 13 normal epithelial ductal cells that were Breast cancer is one of the most common solid malignant purified by laser-microbeam microdissection. We identified tumors among women worldwide. Breast cancer is a heteroge- 301 and 321 transcripts that were significantly upregulated neous disease that is currently classified based on the expression and downregulated in TNBC, respectively. -

Supplementary Data
Supplementary Fig. 1 A B Responder_Xenograft_ Responder_Xenograft_ NON- NON- Lu7336, Vehicle vs Lu7466, Vehicle vs Responder_Xenograft_ Responder_Xenograft_ Sagopilone, Welch- Sagopilone, Welch- Lu7187, Vehicle vs Lu7406, Vehicle vs Test: 638 Test: 600 Sagopilone, Welch- Sagopilone, Welch- Test: 468 Test: 482 Responder_Xenograft_ NON- Lu7860, Vehicle vs Responder_Xenograft_ Sagopilone, Welch - Lu7558, Vehicle vs Test: 605 Sagopilone, Welch- Test: 333 Supplementary Fig. 2 Supplementary Fig. 3 Supplementary Figure S1. Venn diagrams comparing probe sets regulated by Sagopilone treatment (10mg/kg for 24h) between individual models (Welsh Test ellipse p-value<0.001 or 5-fold change). A Sagopilone responder models, B Sagopilone non-responder models. Supplementary Figure S2. Pathway analysis of genes regulated by Sagopilone treatment in responder xenograft models 24h after Sagopilone treatment by GeneGo Metacore; the most significant pathway map representing cell cycle/spindle assembly and chromosome separation is shown, genes upregulated by Sagopilone treatment are marked with red thermometers. Supplementary Figure S3. GeneGo Metacore pathway analysis of genes differentially expressed between Sagopilone Responder and Non-Responder models displaying –log(p-Values) of most significant pathway maps. Supplementary Tables Supplementary Table 1. Response and activity in 22 non-small-cell lung cancer (NSCLC) xenograft models after treatment with Sagopilone and other cytotoxic agents commonly used in the management of NSCLC Tumor Model Response type -

Downregulation of KIF21B by Mir-132-3P Suppresses Cellular Functions in Gastric Cancer Via Regulating Wnt/Β-Catenin Signaling Pathway
Downregulation of KIF21B by miR-132-3p suppresses cellular functions in gastric cancer via regulating Wnt/β-catenin signaling pathway Bingtian Liu Shandong University Cheeloo College of Medicine Ling Qiang Shandong Cancer Hospital: Shandong Cancer Hospital and Institute Bingxin Guan Shandong University Cheeloo College of Medicine Zhipeng Ji ( [email protected] ) Shandong University Cheeloo College of Medicine https://orcid.org/0000-0002-6052-0679 Research Article Keywords: Gastric cancer, KIF21B, miR-132-3p, Wnt/β-catenin signaling Posted Date: September 2nd, 2021 DOI: https://doi.org/10.21203/rs.3.rs-850811/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/18 Abstract Recently, kinesin family member 21B (KIF21B) has been reported to be an oncogene in non-small cell lung cancer and hepatocellular carcinoma. However, the functional role and related mechanisms underlying gastric cancer (GC) pathogenesis remain largely uncovered. Here, we rst found that the expression of KIF21B was upregulated in GC tissues compared with adjunct normal tissues by analysis of Oncomine microarray gene expression datasets and clinical specimens. Knockdown of KIF21B signicantly suppressed the proliferation, migration and invasion in GC cell lines using CCK-8 assay and transwell assay. By luciferase reporter assay, KIF21B was conrmed as the target of miR-132-3p in GC cells and suppressed after miR-132-3p overexpression. Moreover, miR-132-3p was down-regulated and inversely correlated with KIF21B expression in GC tissues. Further functional experiments demonstrated that overexpression of KIF21B remarkedly reversed the suppressive effects of miR-132-3p overexpression on GC cell proliferation, migration and invasion. -

Chemical Agent and Antibodies B-Raf Inhibitor RAF265
Supplemental Materials and Methods: Chemical agent and antibodies B-Raf inhibitor RAF265 [5-(2-(5-(trifluromethyl)-1H-imidazol-2-yl)pyridin-4-yloxy)-N-(4-trifluoromethyl)phenyl-1-methyl-1H-benzp{D, }imidazol-2- amine] was kindly provided by Novartis Pharma AG and dissolved in solvent ethanol:propylene glycol:2.5% tween-80 (percentage 6:23:71) for oral delivery to mice by gavage. Antibodies to phospho-ERK1/2 Thr202/Tyr204(4370), phosphoMEK1/2(2338 and 9121)), phospho-cyclin D1(3300), cyclin D1 (2978), PLK1 (4513) BIM (2933), BAX (2772), BCL2 (2876) were from Cell Signaling Technology. Additional antibodies for phospho-ERK1,2 detection for western blot were from Promega (V803A), and Santa Cruz (E-Y, SC7383). Total ERK antibody for western blot analysis was K-23 from Santa Cruz (SC-94). Ki67 antibody (ab833) was from ABCAM, Mcl1 antibody (559027) was from BD Biosciences, Factor VIII antibody was from Dako (A082), CD31 antibody was from Dianova, (DIA310), and Cot antibody was from Santa Cruz Biotechnology (sc-373677). For the cyclin D1 second antibody staining was with an Alexa Fluor 568 donkey anti-rabbit IgG (Invitrogen, A10042) (1:200 dilution). The pMEK1 fluorescence was developed using the Alexa Fluor 488 chicken anti-rabbit IgG second antibody (1:200 dilution).TUNEL staining kits were from Promega (G2350). Mouse Implant Studies: Biopsy tissues were delivered to research laboratory in ice-cold Dulbecco's Modified Eagle Medium (DMEM) buffer solution. As the tissue mass available from each biopsy was limited, we first passaged the biopsy tissue in Balb/c nu/Foxn1 athymic nude mice (6-8 weeks of age and weighing 22-25g, purchased from Harlan Sprague Dawley, USA) to increase the volume of tumor for further implantation. -

Pflugers Final
CORE Metadata, citation and similar papers at core.ac.uk Provided by Serveur académique lausannois A comprehensive analysis of gene expression profiles in distal parts of the mouse renal tubule. Sylvain Pradervand2, Annie Mercier Zuber1, Gabriel Centeno1, Olivier Bonny1,3,4 and Dmitri Firsov1,4 1 - Department of Pharmacology and Toxicology, University of Lausanne, 1005 Lausanne, Switzerland 2 - DNA Array Facility, University of Lausanne, 1015 Lausanne, Switzerland 3 - Service of Nephrology, Lausanne University Hospital, 1005 Lausanne, Switzerland 4 – these two authors have equally contributed to the study to whom correspondence should be addressed: Dmitri FIRSOV Department of Pharmacology and Toxicology, University of Lausanne, 27 rue du Bugnon, 1005 Lausanne, Switzerland Phone: ++ 41-216925406 Fax: ++ 41-216925355 e-mail: [email protected] and Olivier BONNY Department of Pharmacology and Toxicology, University of Lausanne, 27 rue du Bugnon, 1005 Lausanne, Switzerland Phone: ++ 41-216925417 Fax: ++ 41-216925355 e-mail: [email protected] 1 Abstract The distal parts of the renal tubule play a critical role in maintaining homeostasis of extracellular fluids. In this review, we present an in-depth analysis of microarray-based gene expression profiles available for microdissected mouse distal nephron segments, i.e., the distal convoluted tubule (DCT) and the connecting tubule (CNT), and for the cortical portion of the collecting duct (CCD) (Zuber et al., 2009). Classification of expressed transcripts in 14 major functional gene categories demonstrated that all principal proteins involved in maintaining of salt and water balance are represented by highly abundant transcripts. However, a significant number of transcripts belonging, for instance, to categories of G protein-coupled receptors (GPCR) or serine-threonine kinases exhibit high expression levels but remain unassigned to a specific renal function. -

Table S2 Differentially Expressed Genes Between Oncogene-Introduced Wild-Type and Atf4-/- Cells
Table S2 Differentially expressed genes between oncogene-introduced wild-type and Atf4-/- cells GeneSymbol Gene Name Zscore ratio Genbank Accession Cfd complement factor D 12.714 25036.184 NM_013459 Saa3 serum amyloid A 3 11.189 7437.106 NM_011315 Hp haptoglobin 10.836 5613.776 NM_017370 Prl2c5 prolactin family 2, subfamily c, member 5 7.688 92.732 NM_181852 Cidec cell death-inducing DFFA-like effector c 7.611 982.214 NM_178373 Nrap nebulin-related anchoring protein 7.569 945.372 NM_008733 Adipoq adiponectin, C1Q and collagen domain containing 7.563 940.547 NM_009605 C3 complement component 3 7.310 339.287 NM_009778 Trim12a tripartite motif-containing 12A 7.214 685.215 NM_023835 Apoc1 apolipoprotein C-I 7.026 270.661 NM_007469 Saa1 serum amyloid A 1 6.880 77.790 NM_009117 Lcn2 lipocalin 2 6.658 201.906 NM_008491 Ddx3y DEAD (Asp-Glu-Ala-Asp) box polypeptide 3, Y-linked 6.620 400.047 NM_012008 Pxt1 peroxisomal, testis specific 1 6.470 349.122 NM_153390 Dll4 delta-like 4 6.455 344.263 NM_019454 Lrg1 leucine-rich alpha-2-glycoprotein 1 6.398 326.917 NM_029796 Dcn decorin 6.335 41.800 NM_007833 Rarres2 retinoic acid receptor responder (tazarotene induced) 2 5.985 118.167 NM_027852 Ccl2 chemokine (C-C motif) ligand 2 5.980 12.764 NM_011333 Cyp2f2 cytochrome P450, family 2, subfamily f, polypeptide 2 5.944 584.071 NM_007817 Ccl11 chemokine (C-C motif) ligand 11 5.936 579.003 NM_011330 Plin1 perilipin 1 5.846 198.287 NM_175640 Gsta3 glutathione S-transferase, alpha 3 5.842 105.447 NM_001077353 Barx2 BarH-like homeobox 2 5.836 40.178 NM_013800