Pro-Arrhythmic Signaling of Thyroid Hormones and Its Relevance in Subclinical Hyperthyroidism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endothelin System and Therapeutic Application of Endothelin Receptor
xperim ACCESS Freely available online & E en OPEN l ta a l ic P in h l a C r m f o a c l a o n l o r g u y o J Journal of ISSN: 2161-1459 Clinical & Experimental Pharmacology Research Article Endothelin System and Therapeutic Application of Endothelin Receptor Antagonists Abebe Basazn Mekuria, Zemene Demelash Kifle*, Mohammedbrhan Abdelwuhab Department of Pharmacology, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia ABSTRACT Endothelin is a 21 amino acid molecule endogenous potent vasoconstrictor peptide. Endothelin is synthesized in vascular endothelial and smooth muscle cells, as well as in neural, renal, pulmonic, and inflammatory cells. It acts through a seven transmembrane endothelin receptor A (ETA) and endothelin receptor B (ETB) receptors belongs to G protein-coupled rhodopsin-type receptor superfamily. This peptide involved in pathogenesis of cardiovascular disorder like (heart failure, arterial hypertension, myocardial infraction and atherosclerosis), renal failure, pulmonary arterial hypertension and it also involved in pathogenesis of cancer. Potentially endothelin receptor antagonist helps the treatment of the above disorder. Currently, there are a lot of trails both per-clinical and clinical on endothelin antagonist for various cardiovascular, pulmonary and cancer disorder. Some are approved by FAD for the treatment. These agents are including both selective and non-selective endothelin receptor antagonist (ETA/B). Currently, Bosentan, Ambrisentan, and Macitentan approved -
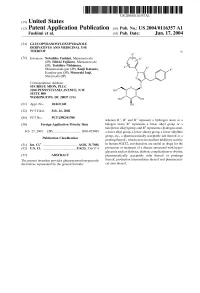
(12) Patent Application Publication (10) Pub. No.: US 2004/0116357 A1 Fushimi Et Al
US 2004O116357A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0116357 A1 Fushimi et al. (43) Pub. Date: Jun. 17, 2004 (54) GLUCOPYRANOSYLOXYPYRAZOLE DERVATIVES AND MEDICINAL USE THEREOF (I) (76) Inventors: Nobuhiko Fushimi, Matsumoto-shi (JP); Hideki Fujikura, Matsumoto-shi (JP); Toshihiro Nishimura, Minamiazumi-gun (JP); Kenji Katsuno, Kamiina-gun (JP); Masayuki Isaji, Shiojiri-shi (JP) Correspondence Address: SUGHRUE MION, PLLC 2100 PENNSYLVANIAAVENUE, N.W. SUTE 800 WASHINGTON, DC 20037 (US) (21) Appl. No.: 10/469,140 (22) PCT Filed: Feb. 26, 2002 (86) PCT No.: PCT/JP02/01708 wherein R', R and R represent a hydrogen atom or a (30) Foreign Application Priority Data halogen atom; R" represents a lower alkyl group or a halo(lower alkyl) group; and R represents a hydrogen atom, Feb. 27, 2001 (JP)...................................... 2001-053085 a lower alkyl group, a lower alkoxy group, a lower alkylthio group, etc., a pharmaceutically acceptable Salt thereof or a Publication Classification prodrug thereof., which exert an excellent inhibitory activity (51) Int. Cl. ................................................ A61K 31/7056 in human SGLT2, and therefore are useful as drugs for the (52) U.S. Cl. ............................................. 514/23: 536/17.4 prevention or treatment of a disease associated with hyper glycemia Such as diabetes, diabetic complications or obesity, (57) ABSTRACT pharmaceutically acceptable Salts thereof or prodrugs The present invention provides glucopyranosyloxypyrazole thereof, production intermediates thereof and pharmaceuti derivatives represented by the general formula: cal uses thereof. US 2004/0116357 A1 Jun. 17, 2004 GLUCOPYRANOSYLOXYPYRAZOLE 0005. In recent years, development of new type antidia DERVATIVES AND MEDICINAL USE THEREOF betic agents has been progressing, which promote urinary glucose excretion and lower blood glucose level by prevent TECHNICAL FIELD ing excess glucose reabsorption at the kidney (J. -

Supplementary Information
Supplementary Information Network-based Drug Repurposing for Novel Coronavirus 2019-nCoV Yadi Zhou1,#, Yuan Hou1,#, Jiayu Shen1, Yin Huang1, William Martin1, Feixiong Cheng1-3,* 1Genomic Medicine Institute, Lerner Research Institute, Cleveland Clinic, Cleveland, OH 44195, USA 2Department of Molecular Medicine, Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH 44195, USA 3Case Comprehensive Cancer Center, Case Western Reserve University School of Medicine, Cleveland, OH 44106, USA #Equal contribution *Correspondence to: Feixiong Cheng, PhD Lerner Research Institute Cleveland Clinic Tel: +1-216-444-7654; Fax: +1-216-636-0009 Email: [email protected] Supplementary Table S1. Genome information of 15 coronaviruses used for phylogenetic analyses. Supplementary Table S2. Protein sequence identities across 5 protein regions in 15 coronaviruses. Supplementary Table S3. HCoV-associated host proteins with references. Supplementary Table S4. Repurposable drugs predicted by network-based approaches. Supplementary Table S5. Network proximity results for 2,938 drugs against pan-human coronavirus (CoV) and individual CoVs. Supplementary Table S6. Network-predicted drug combinations for all the drug pairs from the top 16 high-confidence repurposable drugs. 1 Supplementary Table S1. Genome information of 15 coronaviruses used for phylogenetic analyses. GenBank ID Coronavirus Identity % Host Location discovered MN908947 2019-nCoV[Wuhan-Hu-1] 100 Human China MN938384 2019-nCoV[HKU-SZ-002a] 99.99 Human China MN975262 -

I Regulations
23.2.2007 EN Official Journal of the European Union L 56/1 I (Acts adopted under the EC Treaty/Euratom Treaty whose publication is obligatory) REGULATIONS COUNCIL REGULATION (EC) No 129/2007 of 12 February 2007 providing for duty-free treatment for specified pharmaceutical active ingredients bearing an ‘international non-proprietary name’ (INN) from the World Health Organisation and specified products used for the manufacture of finished pharmaceuticals and amending Annex I to Regulation (EEC) No 2658/87 THE COUNCIL OF THE EUROPEAN UNION, (4) In the course of three such reviews it was concluded that a certain number of additional INNs and intermediates used for production and manufacture of finished pharmaceu- ticals should be granted duty-free treatment, that certain of Having regard to the Treaty establishing the European Commu- these intermediates should be transferred to the list of INNs, nity, and in particular Article 133 thereof, and that the list of specified prefixes and suffixes for salts, esters or hydrates of INNs should be expanded. Having regard to the proposal from the Commission, (5) Council Regulation (EEC) No 2658/87 of 23 July 1987 on the tariff and statistical nomenclature and on the Common Customs Tariff (1) established the Combined Nomenclature Whereas: (CN) and set out the conventional duty rates of the Common Customs Tariff. (1) In the course of the Uruguay Round negotiations, the Community and a number of countries agreed that duty- (6) Regulation (EEC) No 2658/87 should therefore be amended free treatment should be granted to pharmaceutical accordingly, products falling within the Harmonised System (HS) Chapter 30 and HS headings 2936, 2937, 2939 and 2941 as well as to designated pharmaceutical active HAS ADOPTED THIS REGULATION: ingredients bearing an ‘international non-proprietary name’ (INN) from the World Health Organisation, specified salts, esters or hydrates of such INNs, and designated inter- Article 1 mediates used for the production and manufacture of finished products. -

Product Data Sheet
Inhibitors Product Data Sheet Sitaxsentan sodium • Agonists Cat. No.: HY-11103 CAS No.: 210421-74-2 Molecular Formula: C₁₈H₁₄ClN₂NaO₆S₂ • Molecular Weight: 476.89 Screening Libraries Target: Endothelin Receptor Pathway: GPCR/G Protein Storage: Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month SOLVENT & SOLUBILITY In Vitro DMSO : 100 mg/mL (209.69 mM; Need ultrasonic) H2O : 100 mg/mL (209.69 mM; Need ultrasonic) Mass Solvent 1 mg 5 mg 10 mg Concentration Preparing 1 mM 2.0969 mL 10.4846 mL 20.9692 mL Stock Solutions 5 mM 0.4194 mL 2.0969 mL 4.1938 mL 10 mM 0.2097 mL 1.0485 mL 2.0969 mL Please refer to the solubility information to select the appropriate solvent. In Vivo 1. Add each solvent one by one: 10% DMSO >> 40% PEG300 >> 5% Tween-80 >> 45% saline Solubility: ≥ 2.5 mg/mL (5.24 mM); Clear solution 2. Add each solvent one by one: 10% DMSO >> 90% (20% SBE-β-CD in saline) Solubility: ≥ 2.5 mg/mL (5.24 mM); Clear solution BIOLOGICAL ACTIVITY Description Sitaxsentan sodium (IPI 1040 sodium; TBC11251 sodium) is an orally active, highly selective antagonist of endothelin A receptors. In Vitro Sitaxsentan and Bosentan attenuate NTCP transport at higher concentrations, and inhibit human hepatic transporters, which provides a potential mechanism for the increased hepatotoxicity observed for these agents in the clinical setting. Only sitaxsentan decreased OATP transport (52%)[1]. Sitaxsentan and sitaxsentan combined with sildenafil completely prevent the increased expressions of endothelin-1 and of the ETB receptor. -

Advice Concerning the Addition of Certain Pharmaceutical Products
U.S. International Trade Commission COMMISSIONERS Daniel R. Pearson, Chairman Shara L. Aranoff, Vice Chairman Jennifer A. Hillman Stephen Koplan Deanna Tanner Okun Charlotte R. Lane Robert A. Rogowsky Director of Operations Karen Laney-Cummings Director of Industries Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Advice Concerning the Addition of Certain Pharmaceutical Products and Chemical Intermediates to the Pharmaceutical Appendix to the Harmonized Tariff Schedule of the United States Investigation No. 332--476 Publication 3883 September 2006 This report was prepared principally by Office of Industries Philip Stone, Project Leader With assistance from Elizabeth R. Nesbitt Primary Reviewers David G. Michels, Office of Tariff Affairs and Trde Agreements, John Benedetto, and Nannette Christ, Office of Economics Administrative Support Brenda F. Carroll Under the direction of Dennis Rapkins, Chief Chemicals and Textiles Division ABSTRACT Under the Pharmaceutical Zero-for-Zero Initiative, which entered into force in 1995, the United States and its major trading partners eliminated tariffs on many pharmaceuticals, their derivatives, and certain chemical intermediates used to make pharmaceuticals. The U.S. list of pharmaceutical products and chemical intermediates eligible for duty-free treatment under the agreement is given in the Pharmaceutical Appendix to the Harmonized Tariff Schedule of the United States. The Pharmaceutical Appendix is periodically updated to provide duty relief for additional such products, including newly developed pharmaceuticals. This report provides advice on the third update to the agreement, in which approximately 1,300 products are proposed to receive duty-free treatment. -

Orally Active Compound Library (96-Well)
• Bioactive Molecules • Building Blocks • Intermediates www.ChemScene.com Orally Active Compound Library (96-well) Product Details: Catalog Number: CS-L061 Formulation: A collection of 2244 orally active compounds supplied as pre-dissolved Solutions or Solid Container: 96- or 384-well Plate with Peelable Foil Seal; 96-well Format Sample Storage Tube With Screw Cap and Optional 2D Barcode Storage: -80°C Shipping: Blue ice Packaging: Inert gas Plate layout: CS-L061-1 1 2 3 4 5 6 7 8 9 10 11 12 a Empty Vonoprazan Mivebresib AZD0156 BAY-876 Tomivosertib PQR620 NPS-2143 R547 PAP-1 Delpazolid Empty Varenicline b Empty Varenicline (Hydrochlorid Varenicline A-205804 CI-1044 KW-8232 GSK583 Quiflapon MRK-016 Diroximel Empty e) (Tartrate) fumarate SHP099 c Empty A 922500 SHP099 (hydrochlorid Nevanimibe Pactimibe Pactimibe GNF-6231 MLi-2 KDM5-IN-1 PACMA 31 Empty e) hydrochloride (sulfate) Rilmenidine d Empty Cadazolid Treprostinil GSK3179106 Esaxerenone (hemifumarat Rilmenidine Fisogatinib BP-1-102 Avadomide Aprepitant Empty e) (phosphate) Cl-amidine AZD5153 (6- e Empty Maropitant Abscisic acid (hydrochlorid BGG463 WNK463 Ticagrelor Axitinib Hydroxy-2- CGS 15943 Pipamperone Empty e) naphthoic Setogepram Teglarinad f Empty Y-27632 GSK2193874 Lanabecestat CXD101 Ritlecitinib YL0919 PCC0208009 (sodium salt) (chloride) Futibatinib Empty TAK-659 g Empty NCB-0846 GS-444217 (hydrochlorid Navitoclax ABX464 Zibotentan Simurosertib (R)- CEP-40783 MK-8617 Empty e) Simurosertib Choline JNJ- h Empty CCT251236 (bitartrate) Sarcosine Brensocatib AS-605240 PF-06840003 -

Forschung Für Das Leben Entwicklungsprojekte Für Innovative Arzneimittel Inhalt
Forschung für das Leben Entwicklungsprojekte für innovative Arzneimittel Inhalt Vorwort 1 Perspektive 2013 2 Medikamente von übermorgen 12 Wie ein neues Medikament entsteht 16 Innovationen brauchen einen soliden Rahmen 32 Schwerpunkte der vfa-Mitglieder in ihrer Forschung & Entwicklung weltweit 40 Projekte, die bis 2013 zu Zulassungen führen können 42 Der vfa ist der Verband der forschenden Pharma-Unternehmen in Deutschland. Er vertritt die Interessen von 48 weltweit führenden Herstellern und ihren über 100 Tochter- und Schwesterfi rmen in der Gesundheits-, Forschungs- und Wirtschaftspolitik. Die Mitglieder des vfa repräsentieren rund zwei Drittel des gesamten deutschen Arzneimittelmarktes und beschäftigen in Deutschland rund 90.000 Mitarbeiter. Mehr als 17.000 davon arbeiten in Forschung und Entwicklung. Vorwort alle zwei Jahre fragt der vfa – der Verband der forschenden Pharma-Unternehmen – seine Mitglieder, welche Medikamente in den folgenden vier Jahren eine Zulassung erhalten könnten. Das Ergebnis veröff entlicht er dann in einer neuen Ausgabe dieser Broschüre. Schaue ich noch einmal in die Ausgabe von 2007, stelle ich fest, wie viel die Unternehmen mittlerweile von dem eingelöst haben, was sie damals in Aussicht stellten: So haben sie für Krebskranke neue Medikamente herausgebracht, die ihre Lebenserwartung und Lebens- qualität verbessern können, etwa bei Brust- oder Nierenkrebs. Sie haben viele Patienten mit neuen resistenzbrechenden Antibiotika versorgt. Für HIV-Infi zierte stehen nun Medikamente mit zwei neuartigen Wirkprinzipien zur Verfügung, mit denen sich die Viren langfristig in Schach halten lassen. Auch gibt es mittlerweile etliche neue Präparate gegen seltene Krankheiten – etwa bestimmte Leukämien bei Kindern oder den Blutplättchen- mangel bei der Immunkrankheit „thrombozytopenische Purpura“. Zugleich erinnert die Ausgabe 2007 an einige nicht weniger ambitionierte Projekte, die zwischenzeitlich leider eingestellt werden mussten – oftmals nach mehr als zehn Jahren Forschungsarbeit. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -
MM&M Takes a Detailed Look at Key Products in the Pipeline
MM&M takes a detailed look at key products in the pipeline, highlighting the most promising with insights and ratings from Ptop analysts, to IPE provide an overall picture of each therapeutic’s potential value INE 2010 uerosto commodo odionul PROVOCAtiVe AGMM&M’s Pipeline 2010 drawsENTS from the best in drug development, profiling 15 agents with the highest approval probability and brightest commercial prospects. These are the prime near-term launch candidates. The report also provides updates on 202 products in a host of therapeutic areas. Marc Iskowitz reports ualitative change, rather than the quantitative kind, marks best hope to replace warfarin. Then there are the upstarts. Patients this year’s biopharmaceutical pipeline. There has been a shift with rare diseases are finally getting drugs specifically approved for Q in categories poised to yield near-term approvals. And while them. According to a new analysis by the Tufts Center for the Study not the goldmine drug marketers were hoping for, analysts expect of Drug Development, the annual rate of new product approvals the 2010 R&D seam to yield some exciting launch prospects in the worldwide for neglected diseases increased from an average of 1.8 months and years ahead. in 1975-99 to 2.6 in 2000-09. Vaccines and antiviral drugs have also Oncology, a well of innovative approvals in years past, has run seen a resurgence, with physicians talking about a possible cure for relatively dry. “In 2000-2001, we saw Avastin, Tarceva, Sutent, Nexa- hepatitis C and a number of vaccines in the pipeline for ailments var, Gleevec—drugs that revolutionized the way we think about from flu to cancer and diabetes. -

US 2014/0057832 A1 Conrad Et Al
US 20140057832A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0057832 A1 Conrad et al. (43) Pub. Date: Feb. 27, 2014 (54) USE OF RELAXN TO INCREASE ARTERAL Publication Classification COMPLIANCE (51) Int. Cl. (71) Applicants: Kirk P. Conrad, Gainesville, FL (US); A638/22 (2006.01) Sanjeev G. Shroff, Pittsburg, PA (US) (52) U.S. Cl. CPC .................................. A61 K38/2221 (2013.01) (72) Inventors: Kirk P. Conrad, Gainesville, FL (US); USPC 514/1.9; 514/12.7: 514/7.3; 514/6.9; 514/7.4 Sanjeev G. Shroff, Pittsburg, PA (US) (73) Assignee: University of Pittsburgh - Of the (57) ABSTRACT Commonwealth System of Higher Education, Pittsburgh, PA (US) The present invention provides methods for increasing arte rial compliance. The methods generally involve administer (21) Appl. No.: 14/071,705 ing to an individual in need thereof an effective amount of relaxin. The present invention further provides methods of (22) Filed: Nov. 5, 2013 increasing arterial compliance in individuals who have Type 1 or Type 2 diabetes. The present invention further provides Related U.S. Application Data methods of increasing arterial compliance in perimeno (63) Continuation of application No. 12/985,714, filed on pausal, menopausal, and post-menopausal women. The Jan. 6, 2011, now Pat. No. 8,602,998, which is a con present invention further provides methods of increasing arte tinuation of application No. 11/084,670, filed on Mar. rial compliance in individuals who have or who are at risk of 18, 2005, now Pat. No. 7,878,978. developing age-associated arterial stiffness.