Silent Thyroiditis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thyroid Hormone Misuse and Abuse
Endocrine (2019) 66:79–86 https://doi.org/10.1007/s12020-019-02045-1 REVIEW Thyroid hormone misuse and abuse Victor J. Bernet 1,2 Received: 11 June 2019 / Accepted: 2 August 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Thyroid hormone (TH) plays an essential role in human physiology and maintenance of appropriate levels is important for good health. Unfortunately, there are instances in which TH is misused or abused. Such misuse may be intentional such as when individuals take thyroid hormone for unapproved indications like stimulation of weight loss or improved energy. There are instances where healthcare providers prescribe thyroid hormone for controversial or out of date uses and sometimes in supraphysiologic doses. Othertimes, unintentional exposure may occur through supplements or food that unknowingly contain TH. No matter the reason, exposure to exogenous forms of TH places the public at risk for potential adverse side effects. Keywords Thyrotoxicosis ● Thyroid hormone abuse ● Thyroid hormone misuse ● Factitious thyrotoxicosis ● Supplements ● 1234567890();,: 1234567890();,: Analogs Overdose Thyroid hormone misuse and abuse secondary to exogenous TH ingestion that may be unin- tentional or purposeful such as in some cases of Munch- Almost any substance that impacts body physiology and ausen syndrome. Instances of TH misuse can be associated function is at risk for misuse or frank abuse, usually in the with the development of significant side effects. There are misgiven belief that the particular agent whether it be a other instances of chronic, low-grade over treatment with herb, supplement, medication, or hormone has healing TH, which occur for various misreasoning such as weight properties beyond that of which it actually possesses. -
Subacute Thyroiditis with Non-Toxic Hyperfunctioning Thyroid Nodules
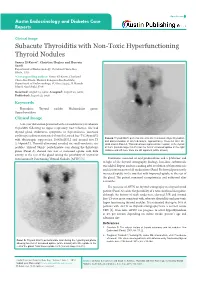
Open Access Austin Endocrinology and Diabetes Case Reports Clinical Image Subacute Thyroiditis with Non-Toxic Hyperfunctioning Thyroid Nodules Samer El-Kaissi*, Christine Hughes and Hussein Saadi Department of Endocrinology, Cleveland Clinic Abu Dhabi, UAE *Corresponding author: Samer El-Kaissi, Cleveland Clinic Abu Dhabi, Medical Subspecialties Institute, Department of Endocrinology, PO Box 112412, Al Maryah Island, Abu Dhabi, UAE Received: August 15, 2016; Accepted: August 22, 2016; Published: August 23, 2016 Keywords Thyroiditis; Thyroid nodule; Multinodular goitre; Hyperthyroidism Clinical Image A 46-year old woman presented with a 4-week history of subacute Thyroiditis following an upper respiratory tract infection. She had thyroid gland tenderness, symptoms of thyrotoxicosis, increased erythrocyte sedimentation rate [45mm/hr], raised free-T4 [29pmol/L] Panel B: Thyroid 99mTc pertechnetate scan after resolution of hyperthyroidism with thyrotropin suppression [0.005mIU/L] and normal free-T3 and discontinuation of all medications, approximately 10-weeks after the [5.64pmol/L]. Thyroid ultrasound revealed six small-moderate size initial scan in Panel A. This scan shows improved tracer uptake in the thyroid nodules. Thyroid 99mTc pertechnetate scan during the thyrotoxic at 0.6% (normal range 0.2-3%) but the foci of increased uptake in the right phase (Panel A) showed two foci of increased uptake with little midzone and left lower zone are still apparent (white arrows). activity in the rest of the gland raising the possibility of coexistent Autonomously Functioning Thyroid Nodules [AFTN] [1]. Treatment consisted of oral prednisolone and a β-blocker and in light of the thyroid scintigraphy findings, low-dose carbimazole was added. Repeat nuclear scanning after resolution of thyrotoxicosis and discontinuation of all medications (Panel B) showed persistently increased uptake in the two foci with improved uptake in the rest of the gland. -

A Case of Thyrotoxic Paralysis Caused by Consumption of Iodocaseine
Journal of Health and Social Sciences 2019; 4,2:277-282 CASE REPORT IN EMERGENCY MEDICINE A case of thyrotoxic paralysis caused by consumption of iodocaseine Antonio Villa1, Gabriella Nucera2 Affiliations: 1 M.D., Department of Emergency, ASST Monza, PO Desio, Monza, Italy 2 M.D., Department of Emergency Medicine, ASST Fatebenefratelli-Sacco, PO Fatebenefratelli, Milano, Italy Corresponding author: Dr Antonio Villa, ASST Monza, PO Desio. Via Fiuggi, 56 20159 Milan, Italy. E-mail: [email protected] Abstract Acute hypokalaemic paralysis is a rare but treatable cause of acute limb weakness. Thyrotoxic paralysis is an uncommon, potentially life-threatening endocrine emergency and it is a rare complication of hyperthyroidism. The most common causes of hyperthyroidism include Graves’ disease, multinodular goiters or solitary thyroid nodule, and iodine-induced thyrotoxicosis ( Jod-Basedow syndrome). Thyreotoxicosis factitia, which is caused by the excessive ingestion of exogenous thyroid hormone or iodine derivatives administration, has been rarely reported as a cause of thyrotoxic paralysis. We describe the case of a young Caucasian male with flaccid paralysis of all four limbs and severe hypokalaemia after inappropriate iodine derivatives (iodocasein) intake to show, in conclusion, how critical care physicians need to be aware of this rare but curable condition. KEY WORDS: Iodocaseine; hypokalaemia; thyrotoxic paralysis. 277 Journal of Health and Social Sciences 2019; 4,2:277-282 Riassunto La paralisi acuta ipokaliemica è una causa rara ma curabile di astenia acuta. La paralisi tireotossica è un'e- mergenza endocrina non comune e potenzialmente pericolosa per la vita ed è una rara complicanza dell'i- pertiroidismo. L'ipertiroidismo è causato prevalentemente dalla malattia di Graves, da gozzi singoli o multi- nodulari, e dalla malattia indotta da iodio ( Jod-Basedow). -
Hyperthyroidism and Thyrotoxicosis
Hyperthyroidism and thyrotoxicosis Assoc. prof. V. Marković, MD, PhD Assoc. prof. A. Punda, MD, PhD A. Barić, MD, nucl. med. spec. Hyperthyroidism- Thyrotoxicosis Hyperthyroidism- elevated serum levels of thyroid hormones caused by overproduction of thyroid hormones Thyrotoxicosis: elevated serum level of thyroid hormones/ excessive amount of circulating thyroid hormone Hyperthyreoidism includes thyreotoxycosis but Thyrotoxicosis is not exclusively caused by hyperthyroidism Classification of thyrotoxicosis Hyperthyroidism Thyrotoxicosis without hyperthyroidism Mb Basedow-Graves Thyrotoxicosis factitia Multinodular toxic goiter Subacute thyroiditis (painfull) Toxic adenoma Subacute thyroiditis (painless) Elevated TSH levels Ectopic thyroid tissue Trophoblastic tumors Iod-Basedow Diffuse toxic goiter (Mb Basedow, Graves) Diffuse toxic goiter Mb. Graves-Basedow Epidemiology and etiology Diffuse toxic goiter (Mb. Graves- Basedow) is an autoimune, multysistemic dissease, wich includes the thyoid gland, infiltrative ophthalmopathy, dermopathy and acropathy. World wide prevalence is about 0,4-2% in women, 0,1% in men, includes 60-90% of hyperthyroidism cases*. It is complex disease with predominant genetic component.& Sex hormones, stress. Disease is caused by TSH receptor stimulating antibodies/ TSH stimulating antibodies (TSAb), in 80-100% patients. *Taunbridge WMG, Vanderpump MPJ. Population screening for autoimmune thyroid disease. Endocriol Metab Clin North Am. 2000;29:239-253. &Brix TH, Kyvik KO, Christensen K, et al. Evdence for a major -

Thyroid Vascularity and Blood Flow
European Journal of Endocrinology (1999) 140 452–456 ISSN 0804-4643 Thyroid vascularity and blood flow are not dependent on serum thyroid hormone levels: studies in vivo by color flow doppler sonography Fausto Bogazzi, Luigi Bartalena, Sandra Brogioni, Alessandro Burelli, Luca Manetti, Maria Laura Tanda, Maurizio Gasperi and Enio Martino Dipartimento di Endocrinologia e Metabolismo, Ortopedia e Traumatologia, Medicina del Lavoro, University of Pisa, Pisa, Italy (Correspondence should be addressed to E Martino, Dipartimento di Endocrinologia e Metabolismo, Ortopedia e Traumatologia, Medicina del Lavoro, Universita` di Pisa, Ospedale di Cisanello, Via Paradisa, 2, 56122 Pisa, Italy) Abstract Objective: Thyroid blood flow is greatly enhanced in untreated Graves’ disease, but it is not known whether it is due to thyroid hormone excess or to thyroid hyperstimulation by TSH-receptor antibody. To address this issue in vivo patients with different thyroid disorders were submitted to color flow doppler sonography (CFDS). Subjects and methods: We investigated 24 normal subjects, and 78 patients with untreated hyperthy- roidism (49 with Graves’ hyperthyroidism, 24 with toxic adenoma, and 5 patients with TSH-secreting pituitary adenoma (TSHoma)), 19 patients with thyrotoxicosis (7 with thyrotoxicosis factitia, and 12 with subacute thyroiditis), 37 euthyroid patients with goitrous Hashimoto’s thyroiditis, and 21 untreated hypothyroid patients with Hashimoto’s thyroiditis. Results: Normal subjects had CFDS pattern 0 (absent or minimal intraparenchimal spots) and mean intraparenchimal peak systolic velocity (PSV) of 4.8 6 1.2 cm/s. Patients with spontaneous hyperthy- roidism due to Graves’ disease, TSHoma, and toxic adenoma had significantly increased PSV (P < 0.0001, P = 0.0004, P < 0.0001 respectively vs controls) and CFDS pattern. -

SUBACUTE THYROIDITIS by SELWYN TAYLOR, M.CH., F.R.C.S
Postgrad Med J: first published as 10.1136/pgmj.33.381.327 on 1 July 1957. Downloaded from 327 SUBACUTE THYROIDITIS By SELWYN TAYLOR, M.CH., F.R.C.S. Surgeon, King's College Hospital, Belgrave Hospitalfor Children, and Hammersmith Hospital; Lecturer in Surgery, Postgraduate Medical School of London The term ' thyroiditis ' implies inflammation of to become much more common in that particular the thyroid gland, but by long usage it has come clinic. I had never seen an example before I950, to be used for a number of conditions in which but saw six in the next three years and pro- infection or trauma play apparently no part. Sub- gressively more each year since then. The con- acute thyroiditis is the title given to a condition dition is much commoner in women than men in which was first clearly described by de Quervain the ratio of about six to one. It has not yet been in I904 and which has been rediscovered, or re- reported in a child and is commonest in the fourth described, on a number of occasions since then, and fifth decades, although I have seen it in a with the result that it now has a multiplicity of student teacher of twenty-one. In our own series different names: granulomatous thyroiditis, giant- there was a history of a pre-existing goitre in 50 cell thyroiditis, pseudotuberculous thyroiditis, per cent. of the patients. The incidence, compared creeping thyroiditis, struma granulomatosa, acute with that of Hashimoto's thyroiditis and Riedel's non-infectious thyroiditis, acute non-suppurative thyroiditis, varies widely in different clinics, but thyroiditis and de Quervain's thyroiditis. -

Thyrotoxicosis
THYROTOXICOSIS: A RETROSPECTIVE STUDY OF CASES SEEN AT NUCLEAR MEDICINE UNIT (NEMROCK) Thesis Submitted for the fulfillment of master degree In nuclear medicine By Amira Hodhod Elsayed M.B.B.CH Under Supervision of Professor Dr. Shawky Ibrahim El.Haddad Professor of Radiotherapy and Nuclear Medicine Faculty of medicine –Cairo University Dr. Gehan Ahmed Yuonis Lecturer of Nuclear Medicine Faculty of medicine –Cairo University Faculty of medicine Cairo University 2013 Acknowledgments First, I would like to thank all my professors who allowed me to quote their work. I particularly grateful to professor Dr/ Shawky El.hadad for his encouragement and generosity in dealing with science and Dr/ Gehan Younis, this study would be much poorer without her help. I am grateful to everyone in Nuclear Medicine department, Cairo University. A special thanks to Dr/ Ahmed Sabrey who helped me in the statistical part of the study. I am deeply indebted to my dear husband Dr/ Hisham Aboelnasr, who was encouraging and supportive throughout. This list would not be completed without mentioning the role of my great mother in supporting me. And last but not least, to my family and my friends for patiently persevering with me. Index List of figures……………………………………………….…….…………………I List of tables………………………………………………………………………….III List of abbreviations………………………………………..………………..….V Introduction and aim of the study………………………..…………….…1 Review of literature……………………………………….………..……………5 Material, methods and data collection…………………………….….49 Results………………………………………………………………………………..52 -

Endocrine Module (PYPP 5260), Thyroid Section, Spring 2002
Endocrine Module (PYPP 5260), Thyroid Section, Spring 2002 THYROID HORMONE TUTORIAL: THYROID PATHOLOGY Jack DeRuiter I. INTRODUCTION Thyroid disorder is a general term representing several different diseases involving thyroid hormones and the thyroid gland. Thyroid disorders are commonly separated into two major categories, hyperthyroidism and hypothyroidism, depending on whether serum thyroid hormone levels (T4 and T3) are increased or decreased, respectively. Thyroid disease generally may be sub-classified based on etiologic factors, physiologic abnormalities, etc., as described in each section below. More than 13 million Americans are affected by thyroid disease, and more than half of these remain undiagnosed. The American Association of Clinical Endocrinologists (AACE) has initiated a campaign to increase public awareness of thyroid disorders and educate Americans about key periods, from birth to advanced age, when people are at increased risk for developing a thyroid disorder (see below). The diagnosis of thyroid disease can be particularly challenging. Patients often present with vague, general clinical manifestations; in particular, the elderly may not associate the signs and symptoms with a disease process and thus may not bring them to the attention of their primary care provider. The prevalence and incidence of thyroid disorders is influenced primarily by sex and age. Thyroid disorders are more common in women than men, and in older adults compared with younger age groups. The prevalence of unsuspected overt hyperthyroidism and hypothyroidism are both estimated to be 0.6% or less in women, based on several epidemiologic studies. Age is also a factor; for overt hyperthyroidism, the prevalence rate is 1.4% for women aged 60 or older and 0.45% for women aged 40 to 60. -

Subacute Thyroiditis Christa M
ENDOCRINECONSULT Subacute Thyroiditis Christa M. Blose, MPAS, PA-C, Holly Jodon, MPAS, PA-C erry, a 48-year-old white man, is referred to endocri- TABLE Jnology for abnormal results Lab Results for Case Patient of thyroid tests performed four Time after symptom onset weeks ago (see table for values). Two months ago, Jerry developed 1 mo 2 mo 4 mo 6 mo an upper respiratory infection TSH (0.40-4.50 mlU/mL) 0.03 0.14 8.23 3.54 (URI) with fever, odynophagia, and anterior neck discomfort. Free T4 (0.8-1.8 ng/dL) 2.58 1.74 0.72 1.66 His symptoms resolved after two weeks; however, he has since de- Free T3 (2.3-4.2 pg/mL) 4.12 1.7 3.0 veloped fatigue and nervousness. The remaining review of sys- TPO antibody (< 20) 11 tems is unremarkable. Medical ESR (0-22 mm/h) 55 history is negative. Jerry denies any factors that can affect thyroid Abbreviations: ESR, erythrocyte sedimentation rate; T3, triiodothyronine; T4, thyroxine; function: He does not take thyroid TPO, thyroid peroxidase antibody. medication, OTC thyroid supple- ments, amiodarone, lithium, or TSH, with normal free thyroxine except for a small, firm thyroid interferon-α, does not have high (T4) and free triiodothyronine gland without the tenderness iodine intake, and has not un- (T3) levels. His thyroid peroxidase elicited previously. Labwork re- dergone head/neck irradiation. antibody (Anti-TPO) is negative. veals an elevated TSH with low There is no personal or family Radioactive iodine uptake (RAIU) free T4 and free T3. -

Thyroid Emergencies
REVIEW ARTICLE Thyroid emergencies Dorina Ylli1, Joanna Klubo ‑Gwiezdzinska2, Leonard Wartofsky3,4 1 Endocrinology Division, University of Medicine, Tirana, Albania 2 National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland, United States 3 Endocrinology Division, Department of Medicine, Georgetown University School of Medicine, Washington DC, United States 4 MedStar Health Research Institute, MedStar Washington Hospital Center, Washington DC, United states KEY WORDS ABSTRACT coma, critical care, Myxedema coma and thyroid storm are among the most common endocrine emergencies presenting to hypothermia, general hospitals. Myxedema coma represents the most extreme, life ‑threatening expression of severe hypothyroidism, hypothyroidism, with patients showing deteriorating mental status, hypothermia, and multiple organ thyrotoxicosis system abnormalities. It typically appears in patients with preexisting hypothyroidism via a common pathway of respiratory decompensation with carbon dioxide narcosis leading to coma. Without early and appropriate therapy, the outcome is often fatal. The diagnosis is based on history and physical find‑ ings at presentation and not on any objective thyroid laboratory test. Clinically based scoring systems have been proposed to aid in the diagnosis. While it is a relatively rare syndrome, the typical patient is an elderly woman (thyroid hypofunction being much more common in women) who may or may not have a history of previously diagnosed or treated thyroid dysfunction. Thyrotoxic storm or thyroid crisis is also a rare condition, established on the basis of a clinical diagnosis. The diagnosis is based on the pres‑ ence of severe hyperthyroidism accompanied by elements of systemic decompensation. Considering that mortality is high without aggressive treatment, therapy must be initiated as early as possible in a critical care setting. -

Uncommon Causes of Thyrotoxicosis*
CONTINUING EDUCATION Uncommon Causes of Thyrotoxicosis* Erik S. Mittra1, Ryan D. Niederkohr1, Cesar Rodriguez1, Tarek El-Maghraby2,3, and I. Ross McDougall1 1Division of Nuclear Medicine and Molecular Imaging Program at Stanford, Department of Radiology, Stanford University Hospital and Clinics, Stanford, California; 2Nuclear Medicine, Cairo University, Cairo, Egypt; and 3Nuclear Medicine, Saad Specialist Hospital, Al Khobar, Saudi Arabia Several of the conditions are self-limiting and do not need Apart from the common causes of thyrotoxicosis, such as prolonged treatment. Graves’ disease and functioning nodular goiters, there are When a patient is thought to be thyrotoxic, a convenient more than 20 less common causes of elevated free thyroid hor- algorithm is to measure free thyroxine (free T ) and mones that produce the symptoms and signs of thyrotoxicosis. 4 thyrotropin (TSH). When the former is higher than normal This review describes these rarer conditions and includes 14 il- lustrative patients. Thyrotropin and free thyroxine should be but the latter is suppressed, thyrotoxicosis is diagnosed. measured and, when the latter is normal, the free triiodothyronine When the former is normal but TSH is low, it is valuable to 123 level should be obtained. Measurement of the uptake of Iis measure free triiodothyronine (free T3); when the latter is recommended for most patients. abnormally high, the diagnosis is T3 toxicosis (2–4). When Key Words: thyrotoxicosis; Graves’ disease; thyroiditis; thyroid both free hormones are normal but TSH is low, the term hormones ‘‘subclinical thyrotoxicosis’’ can be applied (5). Once it has J Nucl Med 2008; 49:265–278 been determined that thyrotoxicosis is present, measure- DOI: 10.2967/jnumed.107.041202 ment of 123I uptake can differentiate among several disor- ders (Table 1). -

Subacute Thyroiditis: Diagnostic Difficulties and Simple Treatment
SUBACUTE THYROIDITIS: DIAGNOSTIC DIFFICULTIES AND SIMPLE TREATMENT Joel I. Hamburger Northland Thyroid Laboratory, Southfield, Michigan Subacute thyroiditis (SAT) constitutes 0.8% produce the systemic manifestations of hyperthyroid of referrals to Northland Thyroid Laboratory ism, usually mild. and is one tenth as common as hyperthyroidism. The laboratory abnormalities are readily under The peak age is 30—SOyears, and women pre standable in terms of the underlying pathophysiology. dominated by a factor of 4.5. Two thirds of the As a consequence of the diffuse inflammation, the patients presented in typical fashion with a thyroidal uptake of radioactive iodine (RAI) is im painful tender goiter, but for one third the paired (1—9). The discharge of thyroid hormone presentation was atypical in that there was no elevates serum thyroxine values (ST4) (1—9). The pain, the principal complaint in most cases erythrocyte sedimentation rate (ESR) is elevated being painless goiter, thyroid nodule, or fea as a nonspecific response to inflammation (1—9), and tures of hyperthyroidism. Elevated erythrocyte occasionally there is an increase in the white blood sedimentation rates were found in all typical cell count (WBC) as well (3,6—9). patients and in 11 of 14 atypical patients. As the disease progresses the local and systemic Serum thyroxine iodide values were elevated in features decline until full recovery is realized, usually two thirds of the patients, typical and atypi within 2—4months. In some instances there is a cal. The radioactive iodine uptake was sub temporary hypothyroid phase (2,3) which rarely nornwl for all and responded subnormally to may prove permanent (10) .