Thyroid Hormone Misuse and Abuse
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Liothyronine Sodium(BANM, Rinnm) Potassium Perchlorate
2174 Thyroid and Antithyroid Drugs with methodological limitations. However, a controlled trial of In myxoedema coma liothyronine sodium may be liothyronine with paroxetine could not confirm any advantage of given intravenously in a dose of 5 to 20 micrograms by 3 O additive therapy. slow intravenous injection, repeated as necessary, usu- 1. Aronson R, et al. Triiodothyronine augmentation in the treat- HO I ally at intervals of 12 hours; the minimum interval be- ment of refractory depression: a meta-analysis. Arch Gen Psychi- OH atry 1996; 53: 842–8. tween doses is 4 hours. An alternative regimen advo- 2. Altshuler LL, et al. Does thyroid supplementation accelerate tri- NH2 cates an initial dose of 50 micrograms intravenously cyclic antidepressant response? A review and meta-analysis of I O the literature. Am J Psychiatry 2001; 158: 1617–22. followed by further injections of 25 micrograms every 3. Appelhof BC, et al. Triiodothyronine addition to paroxetine in I 8 hours until improvement occurs; the dosage may the treatment of major depressive disorder. J Clin Endocrinol then be reduced to 25 micrograms intravenously twice Metab 2004; 89: 6271–6. (liothyronine) daily. Obesity. Thyroid drugs have been tried in the treatment of obes- Liothyronine has also been given in the diagnosis of ity (p.2149) in euthyroid patients, but they produce only tempo- NOTE. The abbreviation T3 is often used for endogenous tri-io- hyperthyroidism in adults. Failure to suppress the up- rary weight loss, mainly of lean body-mass, and can produce se- dothyronine in medical and biochemical reports. Liotrix is USAN rious adverse effects, especially cardiac complications.1 for a mixture of liothyronine sodium with levothyroxine sodium. -

Salutary Lessons from TGA-Approved Sources for Thyroid-Related Medications
REVIEW Barriers in the quest for quality drug information: salutary lessons from TGA-approved sources for thyroid-related medications Jim R Stockigt n iodine-replete countries, about 5% of the population have a ABSTRACT thyroid disorder,1 of whom about a quarter will require long- • term medication either to correct deficiency or to control Product information (PI) for thyroid-related medications I endorsed by the Therapeutic Goods Administration, as thyroid hormone excess. In 2005, about 700 000 Pharmaceutical Benefits Scheme prescriptions were filled in Australia for thyrox- reproduced in the commonly used compilation publications ine, with about 80 000 scripts for the antithyroid drugs carbima- June 2006 MIMS (Monthly index of medical specialties) zole and propylthiouracil.2 annual, MIMS Online and the Australian prescription products Although no major new therapeutic agent has been introduced in guide 2006, was evaluated to see whether it reflects The Medical Journal of Australia ISSN: 0025- contemporary therapeutic practice. the thyroid729X 15 field January for 2007some 186 years, 2 76-79 the body of knowledge and • evidence©The has Medicaladvanced. Journal It is important of Australia that these 2007 developments are Compared with current medical literature, these PI-based reflectedwww.mja.com.au in the product information (PI) widely used by medical sources provide inadequate, inaccurate or outdated practitionersReview and a range of health professionals, who may not refer therapeutic directives. Examples include: directly to current scientific literature on thyroid disorders. MIMS ¾ Incorrect advice that thyroxine therapy should always 3 (Monthly index of medical specialties) annual, in its 30th edition in begin at very low dosage. -

A Case of Thyrotoxic Paralysis Caused by Consumption of Iodocaseine
Journal of Health and Social Sciences 2019; 4,2:277-282 CASE REPORT IN EMERGENCY MEDICINE A case of thyrotoxic paralysis caused by consumption of iodocaseine Antonio Villa1, Gabriella Nucera2 Affiliations: 1 M.D., Department of Emergency, ASST Monza, PO Desio, Monza, Italy 2 M.D., Department of Emergency Medicine, ASST Fatebenefratelli-Sacco, PO Fatebenefratelli, Milano, Italy Corresponding author: Dr Antonio Villa, ASST Monza, PO Desio. Via Fiuggi, 56 20159 Milan, Italy. E-mail: [email protected] Abstract Acute hypokalaemic paralysis is a rare but treatable cause of acute limb weakness. Thyrotoxic paralysis is an uncommon, potentially life-threatening endocrine emergency and it is a rare complication of hyperthyroidism. The most common causes of hyperthyroidism include Graves’ disease, multinodular goiters or solitary thyroid nodule, and iodine-induced thyrotoxicosis ( Jod-Basedow syndrome). Thyreotoxicosis factitia, which is caused by the excessive ingestion of exogenous thyroid hormone or iodine derivatives administration, has been rarely reported as a cause of thyrotoxic paralysis. We describe the case of a young Caucasian male with flaccid paralysis of all four limbs and severe hypokalaemia after inappropriate iodine derivatives (iodocasein) intake to show, in conclusion, how critical care physicians need to be aware of this rare but curable condition. KEY WORDS: Iodocaseine; hypokalaemia; thyrotoxic paralysis. 277 Journal of Health and Social Sciences 2019; 4,2:277-282 Riassunto La paralisi acuta ipokaliemica è una causa rara ma curabile di astenia acuta. La paralisi tireotossica è un'e- mergenza endocrina non comune e potenzialmente pericolosa per la vita ed è una rara complicanza dell'i- pertiroidismo. L'ipertiroidismo è causato prevalentemente dalla malattia di Graves, da gozzi singoli o multi- nodulari, e dalla malattia indotta da iodio ( Jod-Basedow). -

EANM Practice Guideline/SNMMI Procedure Standard for RAIU and Thyroid Scintigraphy
European Journal of Nuclear Medicine and Molecular Imaging (2019) 46:2514–2525 https://doi.org/10.1007/s00259-019-04472-8 GUIDELINES EANM practice guideline/SNMMI procedure standard for RAIU and thyroid scintigraphy Luca Giovanella 1,2 & Anca M. Avram3 & Ioannis Iakovou4 & Jennifer Kwak5 & Susan A. Lawson3 & Elizabeth Lulaj6 & Markus Luster7 & Arnoldo Piccardo8 & Matthias Schmidt9 & Mark Tulchinsky10 & Frederick A. Verburg7 & Ely Wolin11 Received: 11 July 2019 /Accepted: 29 July 2019 / Published online: 7 August 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Introduction Scintigraphic evaluation of the thyroid gland enables determination of the iodine-123 iodide or the 99mTc-pertechnetate uptake and distribution and remains the most accurate method for the diagnosis and quantification of thyroid autonomy and the detection of ectopic thyroid tissue. In addition, thyroid scintigraphy and radioiodine uptake test are useful to discriminate hyperthyroidism from destructive thyrotoxicosis and iodine-induced hyperthyroidism, respectively. Methods Several radiopharmaceuticals are available to help in differentiating benign from malignant cytologically indeterminate thyroid nodules and for supporting clinical decision-making. This joint practice guideline/procedure standard from the European Association of Nuclear Medicine (EANM) and the Society of Nuclear Medicine and Molecular Imaging (SNMMI) provides recommendations based on the available evidence in the literature. Conclusion The purpose of this practice guideline/procedure standard is to assist imaging specialists and clinicians in recommending, performing, and interpreting the results of thyroid scintigraphy (including positron emission tomography) with various radiopharmaceuticals and radioiodine uptake test in patients with different thyroid diseases. Keywords Thyroid . Scintigraphy . Radioiodine uptake test . 99mTc-sestaMIBI, 18F-fluorodeoxyglucose Preamble approval of the Committee on Guidelines and Board of Directors of both organizations. -

Summary of Product Characteristics
Health Products Regulatory Authority Summary of Product Characteristics 1 NAME OF THE MEDICINAL PRODUCT Ultra-TechneKow FM 2.15-43.00 GBq radionuclide generator 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Sodium pertechnetate (99mTc) injection is produced by means of a (99Mo/99mTc) generator. Technetium (99mTc) decays with the emission of gamma radiation with a mean energy of 140 keV and a half-life of 6.01 hours to technetium (99Tc) which, in view of its long half-life of 2.13 x 105 years can be regarded as quasi stable. The radionuclide generator containing the parent isotope 99Mo, adsorbed on a chromatographic column delivers sodium pertechnetate (99mTc) injection in sterile solution. The 99Mo on the column is in equilibrium with the formed daughter isotope 99mTc. The generators are supplied with the following 99Mo activity amounts at activity reference time which deliver the following technetium (99mTc) amounts, assuming a 100% theoretical elution yield and 24 hours time from previous elution and taking into account that branching ratio of 99Mo is about 87%: 99mTc activity (maximum theoretical elutable 1.90 3.81 5.71 7.62 9.53 11.43 15.24 19.05 22.86 26.67 30.48 38.10 GBq activity at ART, 06.00 h CET) 99Mo activity (at ART, 06.00 h 2.15 4.30 6.45 8.60 10.75 12.90 17.20 21.50 25.80 30.10 34.40 43.00 GBq CET) The technetium (99mTc) amounts available by a single elution depend on the real yields of the kind of generator used itself declared by manufacturer and approved by National Competent Authority. -
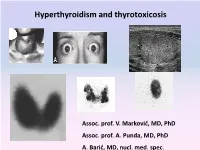
Hyperthyroidism and Thyrotoxicosis
Hyperthyroidism and thyrotoxicosis Assoc. prof. V. Marković, MD, PhD Assoc. prof. A. Punda, MD, PhD A. Barić, MD, nucl. med. spec. Hyperthyroidism- Thyrotoxicosis Hyperthyroidism- elevated serum levels of thyroid hormones caused by overproduction of thyroid hormones Thyrotoxicosis: elevated serum level of thyroid hormones/ excessive amount of circulating thyroid hormone Hyperthyreoidism includes thyreotoxycosis but Thyrotoxicosis is not exclusively caused by hyperthyroidism Classification of thyrotoxicosis Hyperthyroidism Thyrotoxicosis without hyperthyroidism Mb Basedow-Graves Thyrotoxicosis factitia Multinodular toxic goiter Subacute thyroiditis (painfull) Toxic adenoma Subacute thyroiditis (painless) Elevated TSH levels Ectopic thyroid tissue Trophoblastic tumors Iod-Basedow Diffuse toxic goiter (Mb Basedow, Graves) Diffuse toxic goiter Mb. Graves-Basedow Epidemiology and etiology Diffuse toxic goiter (Mb. Graves- Basedow) is an autoimune, multysistemic dissease, wich includes the thyoid gland, infiltrative ophthalmopathy, dermopathy and acropathy. World wide prevalence is about 0,4-2% in women, 0,1% in men, includes 60-90% of hyperthyroidism cases*. It is complex disease with predominant genetic component.& Sex hormones, stress. Disease is caused by TSH receptor stimulating antibodies/ TSH stimulating antibodies (TSAb), in 80-100% patients. *Taunbridge WMG, Vanderpump MPJ. Population screening for autoimmune thyroid disease. Endocriol Metab Clin North Am. 2000;29:239-253. &Brix TH, Kyvik KO, Christensen K, et al. Evdence for a major -

Thyroid Vascularity and Blood Flow
European Journal of Endocrinology (1999) 140 452–456 ISSN 0804-4643 Thyroid vascularity and blood flow are not dependent on serum thyroid hormone levels: studies in vivo by color flow doppler sonography Fausto Bogazzi, Luigi Bartalena, Sandra Brogioni, Alessandro Burelli, Luca Manetti, Maria Laura Tanda, Maurizio Gasperi and Enio Martino Dipartimento di Endocrinologia e Metabolismo, Ortopedia e Traumatologia, Medicina del Lavoro, University of Pisa, Pisa, Italy (Correspondence should be addressed to E Martino, Dipartimento di Endocrinologia e Metabolismo, Ortopedia e Traumatologia, Medicina del Lavoro, Universita` di Pisa, Ospedale di Cisanello, Via Paradisa, 2, 56122 Pisa, Italy) Abstract Objective: Thyroid blood flow is greatly enhanced in untreated Graves’ disease, but it is not known whether it is due to thyroid hormone excess or to thyroid hyperstimulation by TSH-receptor antibody. To address this issue in vivo patients with different thyroid disorders were submitted to color flow doppler sonography (CFDS). Subjects and methods: We investigated 24 normal subjects, and 78 patients with untreated hyperthy- roidism (49 with Graves’ hyperthyroidism, 24 with toxic adenoma, and 5 patients with TSH-secreting pituitary adenoma (TSHoma)), 19 patients with thyrotoxicosis (7 with thyrotoxicosis factitia, and 12 with subacute thyroiditis), 37 euthyroid patients with goitrous Hashimoto’s thyroiditis, and 21 untreated hypothyroid patients with Hashimoto’s thyroiditis. Results: Normal subjects had CFDS pattern 0 (absent or minimal intraparenchimal spots) and mean intraparenchimal peak systolic velocity (PSV) of 4.8 6 1.2 cm/s. Patients with spontaneous hyperthy- roidism due to Graves’ disease, TSHoma, and toxic adenoma had significantly increased PSV (P < 0.0001, P = 0.0004, P < 0.0001 respectively vs controls) and CFDS pattern. -

Thyroid Function Testing and Management During and After Pregnancy Among Women Without Thyroid Disease Before Pregnancy
RESEARCH HEALTH SERVICES Thyroid function testing and management during and after pregnancy among women without thyroid disease before pregnancy Jennifer M. Yamamoto MD, Amy Metcalfe PhD, Kara A. Nerenberg MD, Rshmi Khurana MD, Alex Chin PhD, Lois E. Donovan MD n Cite as: CMAJ 2020 June 1;192:E596-602. doi: 10.1503/cmaj.191664 ABSTRACT BACKGROUND: Screening in pregnancy between October 2014 and September initiated at a median gestational age of for subclinical hypothyroidism, often 2017. We used delivery records, phys- 7 (interquartile range 5–12) weeks. defined as thyroid-stimulating hormone ician billings, and pharmacy and labora- Among women with first TSH measure- (TSH) greater than 2.5 mIU/L or greater tory administrative data. Our key out- ments of 4.01 to 9.99 mIU/L who were than 4.0 mIU/L, is controversial. We comes were characteristics of TSH not immediately treated, the repeat TSH determined the frequency and distribu- testing and the initiation and continua- measurement was 4.00 mIU/L or below tion of TSH testing by gestational age, tion of thyroid hormone therapy. We in 67.9% of pregnancies. Thyroid hor- as well as TSH values associated with calculated the proportion of pregnan- mone was continued post partum for treatment during pregnancy and the fre- cies with thyroid testing and the fre- 44.6% of the women who started ther- quency of postpartum continuation of quency of each specific thyroid test. apy during their pregnancy. thyroid hormone therapy. RESULTS: Of the 188 490 pregnancies INTERPRETATION: The findings of our METHODS: We performed a retrospec- included, 111 522 (59.2%) had at least study suggest that current practice pat- tive cohort study of pregnancies in 1 TSH measurement. -

(12) United States Patent (10) Patent No.: US 8,026,285 B2 Bezwada (45) Date of Patent: Sep
US008O26285B2 (12) United States Patent (10) Patent No.: US 8,026,285 B2 BeZWada (45) Date of Patent: Sep. 27, 2011 (54) CONTROL RELEASE OF BIOLOGICALLY 6,955,827 B2 10/2005 Barabolak ACTIVE COMPOUNDS FROM 2002/0028229 A1 3/2002 Lezdey 2002fO169275 A1 11/2002 Matsuda MULT-ARMED OLGOMERS 2003/O158598 A1 8, 2003 Ashton et al. 2003/0216307 A1 11/2003 Kohn (75) Inventor: Rao S. Bezwada, Hillsborough, NJ (US) 2003/0232091 A1 12/2003 Shefer 2004/0096476 A1 5, 2004 Uhrich (73) Assignee: Bezwada Biomedical, LLC, 2004/01 17007 A1 6/2004 Whitbourne 2004/O185250 A1 9, 2004 John Hillsborough, NJ (US) 2005/0048121 A1 3, 2005 East 2005/OO74493 A1 4/2005 Mehta (*) Notice: Subject to any disclaimer, the term of this 2005/OO953OO A1 5/2005 Wynn patent is extended or adjusted under 35 2005, 0112171 A1 5/2005 Tang U.S.C. 154(b) by 423 days. 2005/O152958 A1 7/2005 Cordes 2005/0238689 A1 10/2005 Carpenter 2006, OO13851 A1 1/2006 Giroux (21) Appl. No.: 12/203,761 2006/0091034 A1 5, 2006 Scalzo 2006/0172983 A1 8, 2006 Bezwada (22) Filed: Sep. 3, 2008 2006,0188547 A1 8, 2006 Bezwada 2007,025 1831 A1 11/2007 Kaczur (65) Prior Publication Data FOREIGN PATENT DOCUMENTS US 2009/0076174 A1 Mar. 19, 2009 EP OO99.177 1, 1984 EP 146.0089 9, 2004 Related U.S. Application Data WO WO9638528 12/1996 WO WO 2004/008101 1, 2004 (60) Provisional application No. 60/969,787, filed on Sep. WO WO 2006/052790 5, 2006 4, 2007. -

Vr Meds Ex01 3B 0825S Coding Manual Supplement Page 1
vr_meds_ex01_3b_0825s Coding Manual Supplement MEDNAME OTHER_CODE ATC_CODE SYSTEM THER_GP PHRM_GP CHEM_GP SODIUM FLUORIDE A12CD01 A01AA01 A A01 A01A A01AA SODIUM MONOFLUOROPHOSPHATE A12CD02 A01AA02 A A01 A01A A01AA HYDROGEN PEROXIDE D08AX01 A01AB02 A A01 A01A A01AB HYDROGEN PEROXIDE S02AA06 A01AB02 A A01 A01A A01AB CHLORHEXIDINE B05CA02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D08AC02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D09AA12 A01AB03 A A01 A01A A01AB CHLORHEXIDINE R02AA05 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S01AX09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S02AA09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S03AA04 A01AB03 A A01 A01A A01AB AMPHOTERICIN B A07AA07 A01AB04 A A01 A01A A01AB AMPHOTERICIN B G01AA03 A01AB04 A A01 A01A A01AB AMPHOTERICIN B J02AA01 A01AB04 A A01 A01A A01AB POLYNOXYLIN D01AE05 A01AB05 A A01 A01A A01AB OXYQUINOLINE D08AH03 A01AB07 A A01 A01A A01AB OXYQUINOLINE G01AC30 A01AB07 A A01 A01A A01AB OXYQUINOLINE R02AA14 A01AB07 A A01 A01A A01AB NEOMYCIN A07AA01 A01AB08 A A01 A01A A01AB NEOMYCIN B05CA09 A01AB08 A A01 A01A A01AB NEOMYCIN D06AX04 A01AB08 A A01 A01A A01AB NEOMYCIN J01GB05 A01AB08 A A01 A01A A01AB NEOMYCIN R02AB01 A01AB08 A A01 A01A A01AB NEOMYCIN S01AA03 A01AB08 A A01 A01A A01AB NEOMYCIN S02AA07 A01AB08 A A01 A01A A01AB NEOMYCIN S03AA01 A01AB08 A A01 A01A A01AB MICONAZOLE A07AC01 A01AB09 A A01 A01A A01AB MICONAZOLE D01AC02 A01AB09 A A01 A01A A01AB MICONAZOLE G01AF04 A01AB09 A A01 A01A A01AB MICONAZOLE J02AB01 A01AB09 A A01 A01A A01AB MICONAZOLE S02AA13 A01AB09 A A01 A01A A01AB NATAMYCIN A07AA03 A01AB10 A A01 -

Triiodothyroacetic Acid in Health and Disease
234 2 S GROENEWEG and others Triac in health and disease 234:2 R99–R121 Review Triiodothyroacetic acid in health and disease Correspondence Stefan Groeneweg, Robin P Peeters, Theo J Visser and W Edward Visser should be addressed Department of Internal Medicine and Academic Center for Thyroid Diseases, Erasmus University to W E Visser Medical Center, Rotterdam, The Netherlands Email [email protected] Abstract Thyroid hormone (TH) is crucial for development and metabolism of many tissues. The Key Words physiological relevance and therapeutic potential of TH analogs have gained attention in f thyroid hormone the field for many years. In particular, the relevance and use of 3,3′,5-triiodothyroacetic f resistance to thyroid hormone (RTH) acid (Triac, TA3) has been explored over the last decades. Although TA3 closely resembles f thyroid hormone analog the bioactive hormone T3, differences in transmembrane transport and receptor isoform- f thyroacetic acid specific transcriptional activation potency exist. For these reasons, the application of TA3 derivatives as a treatment for resistance to TH (RTH) syndromes, especially MCT8 deficiency, is topic of f Triac ongoing research. This review is a summary of all currently available literature about the f TA3 formation, metabolism, action and therapeutic applications of TA3. Endocrinology Journal of Endocrinology of (2017) 234, R99–R121 Journal Introduction Thyroid hormone (TH) is crucial for the development and The deiodinases (D1–3) importantly regulate the bio- metabolism of many tissues. Thyroid stimulating hormone availability of T3 in targets cells, while TH is also (TSH) controls the production and secretion of TH by the metabolized by glucuronidation and sulfation, which thyroid gland, which predominantly produces the pro- enhance biliary excretion (Engler & Burger 1984, Burger hormone thyroxine (T4) and to a lesser extent the bioactive 1986, Visser 1996). -

CYTOMEL - Liothyronine Sodium Tablet Physicians Total Care, Inc
CYTOMEL - liothyronine sodium tablet Physicians Total Care, Inc. ---------- Drugs with thyroid hormone activity, alone or together with other therapeutic agents, have been used for the treatment of obesity. In euthyroid patients, doses within the range of daily hormonal requirements are ineffective for weight reduction. Larger doses may produce serious or even life-threatening manifestations of toxicity, particularly when given in association with sympathomimetic amines such as those used for their anorectic effects. DESCRIPTION Thyroid hormone drugs are natural or synthetic preparations containing tetraiodothyronine (T4, levothyroxine) sodium or triiodothyronine (T3, liothyronine) sodium or both. T4 and T3 are produced in the human thyroid gland by the iodination and coupling of the amino acid tyrosine. T4 contains four iodine atoms and is formed by the coupling of two molecules of diiodotyrosine (DIT). T3 contains three atoms of iodine and is formed by the coupling of one molecule of DIT with one molecule of monoiodotyrosine (MIT). Both hormones are stored in the thyroid colloid as thyroglobulin. Thyroid hormone preparations belong to two categories: (1) natural hormonal preparations derived from animal thyroid, and (2) synthetic preparations. Natural preparations include desiccated thyroid and thyroglobulin. Desiccated thyroid is derived from domesticated animals that are used for food by man (either beef or hog thyroid), and thyroglobulin is derived from thyroid glands of the hog. The United States Pharmacopeia (USP) has standardized the total iodine content of natural preparations. Thyroid USP contains not less than (NLT) 0.17 percent and not more than (NMT) 0.23 percent iodine, and thyroglobulin contains not less than (NLT) 0.7 percent of organically bound iodine.