Subacute Thyroiditis Christa M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Subacute Thyroiditis with Non-Toxic Hyperfunctioning Thyroid Nodules
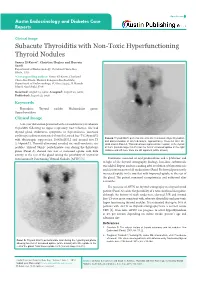
Open Access Austin Endocrinology and Diabetes Case Reports Clinical Image Subacute Thyroiditis with Non-Toxic Hyperfunctioning Thyroid Nodules Samer El-Kaissi*, Christine Hughes and Hussein Saadi Department of Endocrinology, Cleveland Clinic Abu Dhabi, UAE *Corresponding author: Samer El-Kaissi, Cleveland Clinic Abu Dhabi, Medical Subspecialties Institute, Department of Endocrinology, PO Box 112412, Al Maryah Island, Abu Dhabi, UAE Received: August 15, 2016; Accepted: August 22, 2016; Published: August 23, 2016 Keywords Thyroiditis; Thyroid nodule; Multinodular goitre; Hyperthyroidism Clinical Image A 46-year old woman presented with a 4-week history of subacute Thyroiditis following an upper respiratory tract infection. She had thyroid gland tenderness, symptoms of thyrotoxicosis, increased erythrocyte sedimentation rate [45mm/hr], raised free-T4 [29pmol/L] Panel B: Thyroid 99mTc pertechnetate scan after resolution of hyperthyroidism with thyrotropin suppression [0.005mIU/L] and normal free-T3 and discontinuation of all medications, approximately 10-weeks after the [5.64pmol/L]. Thyroid ultrasound revealed six small-moderate size initial scan in Panel A. This scan shows improved tracer uptake in the thyroid nodules. Thyroid 99mTc pertechnetate scan during the thyrotoxic at 0.6% (normal range 0.2-3%) but the foci of increased uptake in the right phase (Panel A) showed two foci of increased uptake with little midzone and left lower zone are still apparent (white arrows). activity in the rest of the gland raising the possibility of coexistent Autonomously Functioning Thyroid Nodules [AFTN] [1]. Treatment consisted of oral prednisolone and a β-blocker and in light of the thyroid scintigraphy findings, low-dose carbimazole was added. Repeat nuclear scanning after resolution of thyrotoxicosis and discontinuation of all medications (Panel B) showed persistently increased uptake in the two foci with improved uptake in the rest of the gland. -

SUBACUTE THYROIDITIS by SELWYN TAYLOR, M.CH., F.R.C.S
Postgrad Med J: first published as 10.1136/pgmj.33.381.327 on 1 July 1957. Downloaded from 327 SUBACUTE THYROIDITIS By SELWYN TAYLOR, M.CH., F.R.C.S. Surgeon, King's College Hospital, Belgrave Hospitalfor Children, and Hammersmith Hospital; Lecturer in Surgery, Postgraduate Medical School of London The term ' thyroiditis ' implies inflammation of to become much more common in that particular the thyroid gland, but by long usage it has come clinic. I had never seen an example before I950, to be used for a number of conditions in which but saw six in the next three years and pro- infection or trauma play apparently no part. Sub- gressively more each year since then. The con- acute thyroiditis is the title given to a condition dition is much commoner in women than men in which was first clearly described by de Quervain the ratio of about six to one. It has not yet been in I904 and which has been rediscovered, or re- reported in a child and is commonest in the fourth described, on a number of occasions since then, and fifth decades, although I have seen it in a with the result that it now has a multiplicity of student teacher of twenty-one. In our own series different names: granulomatous thyroiditis, giant- there was a history of a pre-existing goitre in 50 cell thyroiditis, pseudotuberculous thyroiditis, per cent. of the patients. The incidence, compared creeping thyroiditis, struma granulomatosa, acute with that of Hashimoto's thyroiditis and Riedel's non-infectious thyroiditis, acute non-suppurative thyroiditis, varies widely in different clinics, but thyroiditis and de Quervain's thyroiditis. -

Thyrotoxicosis
THYROTOXICOSIS: A RETROSPECTIVE STUDY OF CASES SEEN AT NUCLEAR MEDICINE UNIT (NEMROCK) Thesis Submitted for the fulfillment of master degree In nuclear medicine By Amira Hodhod Elsayed M.B.B.CH Under Supervision of Professor Dr. Shawky Ibrahim El.Haddad Professor of Radiotherapy and Nuclear Medicine Faculty of medicine –Cairo University Dr. Gehan Ahmed Yuonis Lecturer of Nuclear Medicine Faculty of medicine –Cairo University Faculty of medicine Cairo University 2013 Acknowledgments First, I would like to thank all my professors who allowed me to quote their work. I particularly grateful to professor Dr/ Shawky El.hadad for his encouragement and generosity in dealing with science and Dr/ Gehan Younis, this study would be much poorer without her help. I am grateful to everyone in Nuclear Medicine department, Cairo University. A special thanks to Dr/ Ahmed Sabrey who helped me in the statistical part of the study. I am deeply indebted to my dear husband Dr/ Hisham Aboelnasr, who was encouraging and supportive throughout. This list would not be completed without mentioning the role of my great mother in supporting me. And last but not least, to my family and my friends for patiently persevering with me. Index List of figures……………………………………………….…….…………………I List of tables………………………………………………………………………….III List of abbreviations………………………………………..………………..….V Introduction and aim of the study………………………..…………….…1 Review of literature……………………………………….………..……………5 Material, methods and data collection…………………………….….49 Results………………………………………………………………………………..52 -

Subacute Thyroiditis: Diagnostic Difficulties and Simple Treatment
SUBACUTE THYROIDITIS: DIAGNOSTIC DIFFICULTIES AND SIMPLE TREATMENT Joel I. Hamburger Northland Thyroid Laboratory, Southfield, Michigan Subacute thyroiditis (SAT) constitutes 0.8% produce the systemic manifestations of hyperthyroid of referrals to Northland Thyroid Laboratory ism, usually mild. and is one tenth as common as hyperthyroidism. The laboratory abnormalities are readily under The peak age is 30—SOyears, and women pre standable in terms of the underlying pathophysiology. dominated by a factor of 4.5. Two thirds of the As a consequence of the diffuse inflammation, the patients presented in typical fashion with a thyroidal uptake of radioactive iodine (RAI) is im painful tender goiter, but for one third the paired (1—9). The discharge of thyroid hormone presentation was atypical in that there was no elevates serum thyroxine values (ST4) (1—9). The pain, the principal complaint in most cases erythrocyte sedimentation rate (ESR) is elevated being painless goiter, thyroid nodule, or fea as a nonspecific response to inflammation (1—9), and tures of hyperthyroidism. Elevated erythrocyte occasionally there is an increase in the white blood sedimentation rates were found in all typical cell count (WBC) as well (3,6—9). patients and in 11 of 14 atypical patients. As the disease progresses the local and systemic Serum thyroxine iodide values were elevated in features decline until full recovery is realized, usually two thirds of the patients, typical and atypi within 2—4months. In some instances there is a cal. The radioactive iodine uptake was sub temporary hypothyroid phase (2,3) which rarely nornwl for all and responded subnormally to may prove permanent (10) . -
A Rare Case of Subacute Thyroiditis Simultaneously Complicated by Graves’ Disease: a Case Report and Review of the Literature
Journal of Endocrinology and Thyroid Research ISSN: 2573-2188 Case Report J Endocrinol Thyroid Res Volume 2 Issue 4 August 2017 DOI: 10.19080/JETR.2017.02.555595 Copyright © All rights are reserved by Toshihiko Yanase A Rare Case of Subacute Thyroiditis Simultaneously Complicated by Graves’ Disease: A Case Report and Review of the Literature Ayako Fukushima, Makito Tanabe, Yuichi Terawaki, Takashi Fukuda, Takashi Nomiyama, and Toshihiko Yanase* Department of Endocrinology and Diabetes Mellitus, Fukuoka University, Japan Submission: July 27, 2017; Published: August 28, 2017 *Corresponding author: Toshihiko Yanase, MD, Department of Endocrinology and Diabetes Mellitus, School of Medicine, Fukuoka University, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan, Tel: +81-92-801-1011; Fax: +81-92-865-5163; Email: Abstract A 46-year-old female presented with neck pain and thyrotoxicosis. Further examination revealed that she had both subacute thyroiditis (SAT) and Graves’ disease (GD). These diagnoses were made based on increased thyroid hormone levels, high TSH-R antibody titers, echographic normalized by oral administration of prednisolone. Interestingly, she possessed characteristic HLA typing associated with susceptibility to both SATfindings and ofGD. the A thyroidreview andof four concomitant other cases inflammatory showing simultaneous findings. Her onset thyrotoxicosis, of SAT and inflammatory GD in the literature findings revealed and TSH-R a similar antibodies clinical were course gradually and comparable changes in TRAb in all cases. -

Painless Thyroiditis Associated to Thyroid Carcinoma
case report Painless thyroiditis associated to thyroid carcinoma: role of initial ultrasonography evaluation Raisa Bressan Valentini1, Bruno Mussoi de Macedo1, Rogério Friedrich Izquierdo2, Erika Laurini Souza Meyer1 1 Unidade de Tireoide, Serviço de ABSTRACT Endocrinologia, Irmandade da Santa Casa de Misericórdia de Porto Even though it is a rare event, most associations of thyroid carcinoma with subacute thyroiditis de- Alegre, Universidade Federal de scribed in the literature are related to its granulomatous form (Quervain’s thyroiditis). We present a Ciências da Saúde de Porto Alegre patient with subacute lymphocytic thyroiditis (painless thyroiditis) and papillary thyroid cancer that (UFCSPA), Porto Alegre, RS, Brasil was first suspected in an initial ultrasound evaluation. A 30-year old female patient who was referred 2 Serviço de Radiologia, Irmandade to the emergency room due to hyperthyroidism symptoms was diagnosed with painless thyroiditis da Santa Casa de Misericórdia established by physical examination and laboratory findings. With the presence of a palpable painless de Porto Alegre, UFCSPA, Porto Alegre, RS, Brasil. thyroid nodule an ultrasound was prescribed and the images revealed a suspicious thyroid nodule, microcalcification focus in the heterogeneous thyroid parenquima and cervical lymphadenopathy. Correspondence to: Fine needle aspiration biopsy was taken from this nodule; cytology was assessed for compatibility Erika Laurini Souza Meyer Serviço de Endocrinologia with papillary thyroid carcinoma. Postsurgical pathology evaluation showed a multicentric papillary Irmandade da Santa Casa de carcinoma and lymphocytic infiltration. Subacute thyroiditis, regardless of type, may produce tran- Misericórdia de Porto alegre sitory ultrasound changes that obscure the coexistence of papillary carcinoma. Due to this, initial Professor Annes Dias, 295 90020-090 – Porto Alegre, RS, Brasil thyroid ultrasound evaluation should be delayed until clinical recovery. -

Silent Thyroiditis
CLINICAL REVIEW Silent Thyroiditis Roland Sakiyama, MD Los Angeles, California Silent thyroiditis is an increasingly recognized cause of transient thyrotoxicosis. Inflammatory destruction of thyroid follicles results in release of preformed thyroxine and triiodothyronine. Patients present with symptoms of thyrotoxicosis, but unlike subacute thyroiditis, lack thyroid pain or ten derness. The thyrotoxic state spontaneously resolves in 2 to 12 weeks at which time the patient either returns to a euthyroid state or passes through a transient hypothyroid phase. Diagnostic laboratory findings include eleva tions of thyroxine and triiodothyronine and a markedly depressed radioactive iodine uptake. It is imperative for the primary care physician to distinguish silent thyroiditis from chronic causes of hyperthyroidism, eg, Graves' dis ease, since treatment must be palliative rather than definitive. Long-term prognosis is usually excellent. ver the past decade a newly recognized subacute majority of cases of hyperthyroidism. Silent thyroiditis O thyroid disorder has emerged as an important now accounts for upwards of 20 to 30 percent of newly cause of thyrotoxicosis. First described in 1975 by diagnosed cases of thyrotoxicosis.2'6 While growing Gluck et al,1 this disease, like classical subacute physician awareness may account for part of the in thyroiditis, is characterized by inflammation and dis creased incidence, this silent form of subacute thy ruption of normal thyroid architecture resulting in the roiditis appears to be occurring with increased fre release of preformed stores of thyroid hormone. Un quency.2 like subacute thyroiditis, however, patients lack Silent thyroiditis afflicts women more commonly thyroid pain or tenderness. This subacute form of than men in an approximately 2:1 to 3:1 ratio. -

Subacute Thyroiditis Secondary to Moderna COVID-19 Vaccine: a Case Report of a Rare Manifestation
Advances in Clinical Medical Research and Healthcare Delivery Volume 1 Issue 2 Article 9 2021 Subacute Thyroiditis Secondary to Moderna COVID-19 Vaccine: A Case Report of a Rare Manifestation Mayank Patel HCA Healthcare, [email protected] Marika Shahid HCA Healthcare, [email protected] Ahmad Khawaja HCA Healthcare, [email protected] Chibuzor Ejike HCA Healthcare, [email protected] Kavitha Vemuri HCA Healthcare, [email protected] Follow this and additional works at: https://scholar.rochesterregional.org/advances Part of the Endocrinology, Diabetes, and Metabolism Commons, and the Medical Education Commons Recommended Citation Patel M, Shahid M, Khawaja A, Ejike C, Vemuri K. Subacute Thyroiditis Secondary to Moderna COVID-19 Vaccine: A Case Report of a Rare Manifestation. Advances in Clinical Medical Research and Healthcare Delivery. 2021; 1(2). doi: 10.53785/2769-2779.1019. ISSN: 2769-2779 This Article is brought to you for free and open access by RocScholar. It has been accepted for inclusion in Advances in Clinical Medical Research and Healthcare Delivery by an authorized editor of RocScholar. Subacute Thyroiditis Secondary to Moderna COVID-19 Vaccine: A Case Report of a Rare Manifestation Abstract The SARS-CoV-2 led to a global pandemic, infecting millions of lives within only a short period of time. The symptoms of the disease vary with a subset of the population developing debilitating sequelae. Through the emergency use authorization (EUA), multiple vaccines have been released against the novel virus in record time. Long term and rare sequelae from the vaccine are poorly understood. DeQuervain’s subacute thyroiditis is a self-limiting and painful inflammation of the thyroid gland usually associated with viral infections. -

De Quervain's Subacute Thyroiditis Presenting As a Postgrad Med J: First Published As 10.1136/Pgmj.74.876.602 on 1 October 1998
Postgrad MedJ3 1998;74:602-615 © The Fellowship of Postgraduate Medicine, 1998 Short reports De Quervain's subacute thyroiditis presenting as a Postgrad Med J: first published as 10.1136/pgmj.74.876.602 on 1 October 1998. Downloaded from painless solitary thyroid nodule T Bianda, C Schmid Summary tion, drug or iodine exposure, or pregnancy. We describe a 39-year-old woman pre- Her sister had Graves' disease. Physical exam- senting with a painless solitary thyroid ination showed a regular heart rate of 72 beats/ nodule, initially without signs suggesting min, a blood pressure of 120/85 mmHg, an thyroiditis. The serum level ofthyrotropin axilla temperature of 36.8°C, no tremor and was suppressed whereas those of thyrox- unremarkable reflexes. There were no signs of ine and triiodothyronine were normal. ophthalmopathy or dermopathy. We found a Fine needle aspiration cytology showed no painless nodule in the right lobe of the thyroid signs ofinflammation or malignancy. One gland with a diameter of 2x2 cm without lym- week later, the patient felt pain and phadenopathy. Serum thyrotropin (TSH) was tenderness on her neck, and erythrocyte low (< 0.05 mUll), free thyroxine (fT4) was 17 sedimentation rate and C-reactive protein pmol/l (normal range 8.5-19) and total tri- were markedly elevated. Thyroid scintig- iodothyronine (T3) was 2.6 nmol/l (0.9-2.8). raphy showed a suppressed thyroid TSH-receptor and antimicrosomal antibodies pertechnetate uptake. At that time, the could not be detected. Thyroid sonography diagnosis of subacute thyroiditis was confirmed the presence of an inhomogenous, made. -

Subclinical Hyperthyroidism
Subclinical Hyperthyroidism Disclaimer Contents Contents ........................................................................................................................................................1 Background...................................................................................................................................................2 About Subclinical Hyperthyroidism ...................................................................................................................................... 2 • Thyroiditis .............................................................................................................................................................................. 2 Subacute thyroiditis (also known as de Quervain's) ........................................................................................................ 2 • Graves' disease .................................................................................................................................................................... 2 Assessment ...................................................................................................................................................3 Management ................................................................................................................................................3 Transient subclinical hyperthyroidism in pregnancy ...................................................................................................... 3 Carbimazole dose -
Subacute Thyroiditis As a Presenting Manifestation of COVID-19
BMJ Case Rep: first published as 10.1136/bcr-2020-239953 on 18 December 2020. Downloaded from Case report Subacute thyroiditis as a presenting manifestation of COVID-19: a report of an exceedingly rare clinical entity Uddalak Chakraborty, Shrestha Ghosh, Atanu Chandra , Aritra Kumar Ray Internal Medicine, RG Kar SUMMARY (temperature—99.6°F) with a pulse rate of 104 Medical College and Hospital, The SARS-CoV -2 has wreaked havoc globally and beats/min. His blood pressure was 124/78 mm Hg, Kolkata, West Bengal, India has claimed innumerable lives all over the world. respiratory rate 18/min, a random capillary blood The symptoms of this disease may range from mild glucose 117 mg/dL and oxygen saturation 99% on Correspondence to influenza- like symptoms to severe acute respiratory room air. A tender swelling (4 cm×5 cm) with a Dr Atanu Chandra; chandraatanu123@ gmail. com distress syndrome with high morbidity and mortality. normal surface temperature and firm consistency With improved diagnostic techniques and better disease was noted in the lower part of the front of his Accepted 30 November 2020 understanding, an increased number of cases are neck, with well-defined margins and normal over- being reported with extrapulmonary manifestations of lying skin, clinically resembling a diffusely enlarged this disease ranging from renal and gastrointestinal thyroid gland. The swelling displaced vertically on to cardiac, hepatic, neurological and haematological deglutition, but no movement could be observed dysfunction. Subacute thyroiditis is a self-limiting and on tongue protrusion. No signs of compression painful thyroid gland inflammation most often secondary could be elicited. -

The Good, the Bad, the Thyroid Gland
8 ACOFP 55th Annual Convention & Scientific Seminars New Physicians and Residents: The Good, The Bad, The Thyroid Gland Natasha Bray, DO 3/14/2018 Natasha N. Bray, DO, MSEd, FACOI, FACP Visiting Professor of Rural Medicine – Internal Medicine Oklahoma State University College of Osteopathic Medicine ▪ Length: 5 cm ▪ Width: 2 cm ▪ Depth: 2 cm ▪ Weight 10-20 grams 1 3/14/2018 ▪ Active Thyroid Hormone ▪ Thyroxine (T4) and Triiodothyronine (T3) ▪ Iodine is critical to formation of thyroid hormone ▪ Dietary sources – seafood, dairy products, iodized salt ▪ Iodine deficiency in US is rare ▪ Regulation ▪ TSH secretion ▪ Peripheral conversion of T4 to T3 ▪ T4:T3 secretion by thyroid gland 20:1 ▪ Most T3 (80%) results from 5’-deiodination of T4 in peripheral tissue Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson J, Loscalzo J. Harrison's Manual of Medicine, 18e; 2014 Available at: http://accessmedicine.mhmedical.com/content.aspx?bookid=1140§ionid=63503819 Accessed: January 15, 2018 ▪ Thyroxine-binding globulin (TBG) ▪ Transport T3 & T4 ▪ Only free T4 and free T3 are metabolically active ▪ In the serum, 0.04% of total T4 and T3 are in free or active forms ▪ T3 has up to 10 times the potency of T4 2 3/14/2018 TSH Free T4 Hypothyroid High Low Hyperthyroid Los High 3 3/14/2018 ▪ 36-year-old female reports insomnia, weight loss and anxiety over the past 8-10 weeks. She did not get her period this month. ▪ Physical Exam ▪ Alert and oriented ▪ Vital signs are normal ▪ Thyroid gland is diffusely enlarged. No discrete nodule palpated. ▪ No exophthalmos ▪ No pretibial myxedema What lab results would you expect to find? ▪ 36-year-old female reports insomnia, A.