Making Sense of TB Data Guide for Collection, Analysis and Use of TB Data for Health Workers in Zimbabwe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Zimbabwe Rapid Response Drought 2015
Resident / Humanitarian Coordinator Report on the use of CERF funds RESIDENT / HUMANITARIAN COORDINATOR REPORT ON THE USE OF CERF FUNDS ZIMBABWE RAPID RESPONSE DROUGHT 2015 RESIDENT/HUMANITARIAN COORDINATOR Bishow Parajuli REPORTING PROCESS AND CONSULTATION SUMMARY a. Please indicate when the After Action Review (AAR) was conducted and who participated. The CERF After Action Review took place on 25 May 2016. The review brought together focal points from the following key sectors and agencies: Health and Nutrition: UNICEF and WHO, Agriculture: FAO, Food Security: WFP and WASH: UNICEF. Considering the importance of the lessons learnt element, some sectors which did not benefit from the funding did nevertheless participate in order to gain a better understanding of CERF priorities, requirements and implementation strategies. b. Please confirm that the Resident Coordinator and/or Humanitarian Coordinator (RC/HC) Report was discussed in the Humanitarian and/or UN Country Team and by cluster/sector coordinators as outlined in the guidelines. YES X NO Sector focal points were part of the CERF consultation from inception through to final reporting. In addition, a CERF update was a standing agenda item discussed during the monthly Humanitarian Country Team meetings. c. Was the final version of the RC/HC Report shared for review with in-country stakeholders as recommended in the guidelines (i.e. the CERF recipient agencies and their implementing partners, cluster/sector coordinators and members and relevant government counterparts)? YES X NO All -

GOVERNMENT GAZETTE, 31ST Ocromer, 1986
_ ZIMBABWEAN GOVERNMENT GAZETTE Po a a Published by Authority ra Vol. LXIV, No. 56 31st OCTOBER, 1986 . Price 40c ’ General Notice 740 of 1986. The service to operate as follows— - . ; (a) depart Bulawayo Wednesday and Saturday 9 a.m., arrive i Se at ROAD MOTOR TRANSPORTATION ACT [CHAPTER262] Shashi 2.15 p.m.; i eae (b) depart, Bulawayo ¢ Friday and Sunday..5 p.m., arrive ‘ Applications in Connexion with Road Service Permits . Shashi 10.15 p.m.; , , (c) depart Shashi Monday and Thursday ~ 6 am., arrive Bula- ‘IN terms of subsection (4) of section 7 of the Road Motor wayo 11.15 a.m.; Transportation Act [Chapter 262], notice is hereby given that. (d) depart Shashi Saturday 3.am., arrive Bulawayo the applications detailed in the Schedule, for the issue or . 7.15 a.m.; amendment of road service permits, have been received for the (e). depart Shashi Sunday 7 a.m., arrive Bulawayo 12.15 p.m. consideration of the Controller of Road Motor Transportation. - Any person wishing to object to any such applicationmust lodge with the Controller of Road Motor Transportation, Kukura Kurerwa Bus Co. ' P.O. Box 8332, Causeway— a LOVNAIROBL go186. Permit: 14411. Motor-omnibus. Passenger-capacity: (a) a notice, in writing, of-his intention to ‘object, so asto ~ each the Controller’s office not later than the 21st Route: Nyamasoto Airfield - Masosowa Kraal - Charuwa November; 1986; / Kraal - Fosiyasi Store - Jairosi Kraal - Chironga Mission - (b) his objection and the grounds therefore, on form R.M-T. Chawanda ~ Mt, Darwin - Argyle Park - Bindura - Wayerera "24, together with twocopies thereof, so as to reach the School - Muchapondwa School - Shangwa Kraal - Chabwino Controller’s office not later than the 12th December, Farm - Shamva Road Junction - Harare. -
Approval Form
APPROVAL FORM Midlands State University The undersigned certify that they have read and made recommendations to the Midlands State University for acceptance of a research project entitled: Rural Local Authorities and investment attraction. The case of UMzingwane Rural District Council. The project was submitted in partial fulfilment of the requirements of the Bachelor of Science Honours Degree in Local Governance Studies. Supervisor Signature ………………………………………Date ………/………/………… Chairperson Signature ………………………………………Date ………/………/………… i RELEASEFORM Name of Student: Khulani Dube Registration Number: R101338f Dissertation Title: Rural Local Authorities and investment attraction. The case of UMzingwane Rural District Council. Degree Title: Bachelor of Science Honours Degree inLocal Governance Studies. Year of Completion: 2013 Permission is hereby being granted to Midlands State University Library to produce copies of this dissertation to lendcopies for private, scholarly or scientific research only. The author reserves the publication rights. Neither the dissertation nor extensive extracts from it may be printed or reproduced without the author’s written permission. Signed……………………………………………………………………………………… Date……………………………………………………………………………………….. Contact Details:15255Pumula South Bulawayo Telephone Number: 0772 528 806 Email address : [email protected] ii DECLARATION I KhulaniDubedeclare that this research is my original work that has not been submitted to any other University. The sources I used have been acknowledged. Date : October 2013 Student’s name : KhulaniDube Signature : ………………… iii DEDICATIONS I dedicate this research to my aunt Mrs P Bhebhe and my mother Mrs P Dube. iv ACKNOWLEDGEMENTS I would like to extend my gratitudeto my learning institution Midlands State University for the consistent support in all my academic endeavours. Special mention is due to the Local Governance Studies Department and its dedicated staff for providing me with the necessary and requisite skills and knowledge that have proved to be useful during the compilation of this project. -

Agnes Asekenye-Oonyu/OCHA/Zimbabwe/2006
Agnes Asekenye-Oonyu/OCHA/Zimbabwe/2006 SAMPLE OF ORGANISATIONS PARTICIPATING IN CONSOLIDATED APPEALS AARREC CRS HT MDM TEARFUND ACF CWS Humedica MEDAIR TGH ACTED Danchurchaid IA MENTOR UMCOR ADRA DDG ILO MERLIN UNAIDS Africare Diakonie Emergency Aid IMC NCA UNDP AMI-France DRC INTERMON NPA UNDSS ARC EM-DH Internews NRC UNEP ASB FAO INTERSOS OCHA UNESCO ASI FAR IOM OHCHR UNFPA AVSI FHI IPHD OXFAM UN-HABITAT CARE Finnchurchaid IR OXFAM UK UNHCR CARITAS French RC IRC PA (formerly ITDG) UNICEF CEMIR INTERNATIONAL FSD IRD PACT UNIFEM CESVI GAA IRIN PAI UNJLC CFA GOAL IRW Plan UNMAS CHF GTZ Islamic RW PMU-I UNOPS CHFI GVC JOIN PU UNRWA CISV Handicap International JRS RC/Germany VIS CMA HealthNet TPO LWF RCO WFP CONCERN HELP Malaria Consortium Samaritan's Purse WHO Concern Universal HelpAge International Malteser SECADEV World Concern COOPI HKI Mercy Corps Solidarités World Relief CORDAID Horn Relief MDA SUDO WV COSV TABLE OF CONTENTS 1. EXECUTIVE SUMMARY ............................................................................................................................. 1 Table I: Requirements, Commitments/Contributions and Pledges per Sector ............................................. 3 Table II. Requirements, Commitments/Contributions and Pledges by Priority............................................. 3 Table III. Requirements, Commitments/Contributions and Pledges per Appealing Organisation................. 4 2. CHANGES IN THE CONTEXT, HUMANITARIAN NEEDS, AND RESPONSE........................................... 6 3. RESPONSE PLANS................................................................................................................................... -

Zimbabwe Livelihood Baseline Profile
Zimbabwe Livelihood Baseline Profile Kariba Valley Kariangwe Jambezi Communal August-September 20101 Main Conclusions and Implications Crop production is the main food source over the reference year contributing 38 percent of very poor household food access and 82 percent for the Better-off. The main constraints to improved land utilisation and crop production are lack of draught power and poor access to seeds and fertiliser. Extension services and monitoring of agriculture activities should be strengthened through support to the ministry of agriculture’s department of extension services (AGRITEX). The livelihood zone borders with Mutusadona and Chizarira national parks. Proximity to national parks increases human, livestock and wildlife interaction. Elephants, Baboons, Buffaloes and Quela birds often stray into fields and destroy crops. Livestock production, which has relatively increased in recent years, is also limited by concerns over tsetse fly outbreaks. Surrounding communities receive little benefit from resources in the national parks except for the occasional slaughter of wild animals. Strengthening the CAMPFIRE scheme provides a framework for legal and sustainable access to natural resources found in the national parks. Food aid distributed for six months enabled very poor and poor households to access their minimum food requirements. Limited livelihood options and adverse weather conditions combine to increase very poor and poor households’ vulnerability to food insecurity and poverty. Over the last ten years, the risk of food insecurity has been addressed primarily through food aid distributions. External assistance whose focus has been on addressing immediate consumption needs has created dependency and is undermining long term household coping capacity and development prospects. -

PARKS and WILD LIFE ACT Acts 14/1975, 42/1976 (S
TITLE 20 TITLE 20 Chapter 20:14 PREVIOUS CHAPTER PARKS AND WILD LIFE ACT Acts 14/1975, 42/1976 (s. 39), 48/1976 (s. 82), 4/1977, 22/1977, 19/1978, 5/1979, 4/1981 (s. 19), 46/1981, 20/1982 (s.19 and Part XXVI), 31/1983, 11/1984, 35/1985, 8/1988 (s. 164), 1/1990, 11/1991 (s. 24), 22/1992 (s. 14); 19/2001; 22/2001; 13/2002. R.G.Ns 1135/1975, 52/1977, 126/1979, 294/1979, 265/1979, 294/1979, 748/1979; S.Is 675/1979, 632/1980, 640/1980, 704/1980, 773/1980, 781/1980, 786/1980, 139/1981, 140/1981, 181/1981, 183/1981, 639/1981, 860/1981, 139/1982, 140/1982, 337/1983, 454/1983, 123/1991 ARRANGEMENT OF SECTIONS PART I PRELIMINARY Section 1. Short title. 2. Interpretation. PART II PARKS AND WILD LIFE MANAGEMENT AUTHORITY 3. Establishment of Parks and Wild Life Management Authority. 4. Functions of Parks and Wild Life Management Authority. 5. Establishment and composition of Parks and Wild Life Management Authority Board. 6. Minister may give Board policy directions. 7. Minister may direct Board to reverse, suspend or rescind its decisions or actions. 8. Execution of contracts and instruments by Authority. 9. Reports of Authority. 10. Appointment and functions of Director-General and Directors of Authority. 11. Appointment of other staff of Authority. PART IIA FINANCIAL PROVISIONS 12. Funds of Authority. 13. Financial year of Authority. 14. Annual programmes and budgets of Authority. 15. Investment of moneys not immediately required by Authority. 16. Accounts of Authority. -

Bulletin #38 • July 2020 •
Bulletin #38 • July 2020 • www.zrbf.co.zw IN THIS REPORT The purpose of the ZRBF High Frequency Monitoring Bulletin is to avail Overall Results and Implications 2 real time data and information on identified and agreed trigger indicators Status Update on Macro-Trigger Indicators 4 for the activation of the crisis modifier, performance monitoring, Vegetation Condition Index 4 programming and other decisions for the overall ZRBF adaptive Summary of Broad Classification: Micro programme management. Information presented in this bulletin is readily Trigger Indicators 5 available in the HFM Online Database, accessible using this url Detailed Micro Trigger Indicators Update and Proposed Mitigatory Activities 7 https://197.155.231.242/undp/ZRBF/HFMS/index.php Biophysical Trigger indicators 7 Production Trigger indicators 9 The bulletin contains official information for the month of June 2020 Access Trigger Indicators 10 collected from various sources by ZRBF partners and analysed by Trade Trigger Indicators 12 ZRBF PMU. The High Frequency Monitoring Bulletin is a product of collaboration between the ZRBF Partners and other government agencies. For questions and comments regarding this bulletin, kindly get in touch with Vhusomuzi Sithole ([email protected]), Shupikai Mutyambizi ([email protected]). UNDP Zimbabwe, ZRBF Programme Management Unit Arundel Office Park, Block 9, Norfolk Rd, Mt. Pleasant, Harare, Zimbabwe +263 4 338836-44 1. Overall Results and Implications Summary Classification Key Highlights According to the High Frequency Monitoring (HFM) classification, all the 18 districts were in the Alert category. The following micro indicators, which in the Emergency Stage, drove this overall classification. • Cattle Price in Beitbridge and Binga • Common Diarrhoea Reported Cases in Beitbridge, Chiredzi, Kariba, Lupane, Mberengwa, Mbire, Mudzi, Mutoko, Mwenezi, Nkayi, Nyanga, Umguza and Zvishavane. -

The Impact of Diptank Rehabilitation on the Occurrence of Ticks and Tickborne Diseases in Umzingwane District, Matabeleland South, Zimbabwe
IOSR Journal of Agriculture and Veterinary Science (IOSR-JAVS) e-ISSN: 2319-2380, p-ISSN: 2319-2372. Volume 8, Issue 2 Ver. II (Feb. 2015), PP 112-118 www.iosrjournals.org The Impact of diptank rehabilitation on the occurrence of Ticks and tickborne diseases in Umzingwane District, Matabeleland South, Zimbabwe J. Masuku1,3, A.B. Dube1 and B. Moyo2 1Department of Animal Science and Rangeland management, Lupane State University, P.O. AC 255, Ascot, Bulawayo, Zimbabwe; 2Department of Agribusiness, Solusi University P.O. Solusi, Bulawayo, Zimbabwe. 3 Provincial Veterinary office Matabeleland South, Box 1 Gwanda, Zimbabwe. Abstract: The objective of this study was to determine the impact of diptank rehabilitation on the prevalence of ticks, tick borne diseases (TBDs) and other tick related conditions in Umzingwane district of Zimbabwe. About 120 cattle farmers and three veterinary officers were randomly interviewed using a structured questionnaire. Before diptank rehabilitation programme, 70% of the farmers owned an average of 7 cattle and handling facilities were not intact. Furthermore, they were no footbath, no roof and head clump. As a result, all the farmers reported poor tick control due to the fact that cattle were escaping from the handling facilities before dipping. About 55% farmers lost cattle due to tick related conditions before diptank rehabilitation resulting in 17% cattle mortality. About 57% cases of tick borne diseases were reported and 70% farmers reported that their cattle suffered from teat and udder damage, abscess and screwworm wounds due to tick infestation. As a result 78% farmers resorted to the use of alternative dipping remedies such as used engine oil (45%), hand spraying (18%), and hand pulling (15%). -
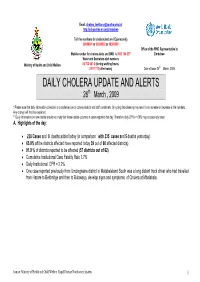
DAILY CHOLERA UPDATE and ALERTS 26Th March , 2009
Email: [email protected] http://ochaonline.un.org/zimbabwe Toll free numbers for cholera alert are ( Econet only) 08089001 or 08089002 or 08089000 Office of the WHO Representative in Mobile number for cholera alerts and SMS is 0912 104 257 Zimbabwe Water and Sanitation alert numbers Ministry of Health and Child Welfare 04 703 941-2 (during working hours) 2 917 710 (after hours) Date of issue:26th March, 2009 DAILY CHOLERA UPDATE AND ALERTS 26th March , 2009 * Please note that daily information collection is a challenge due to communication and staff constraints. On-going data cleaning may result in an increase or decrease in the numbers. Any change will then be explained. ** Daily information on new deaths should not imply that these deaths occurred in cases reported that day. Therefore daily CFRs >100% may occasionally result A. Highlights of the day: • 228 Cases and 8 deaths added today (in comparison with 235 cases and 5 deaths yesterday) • 65.0% of the districts affected have reported today 39 out of 60 affected districts) • 91.9 % of districts reported to be affected (57 districts out of 62) • Cumulative Institutional Case Fatality Rate 1.7% • Daily Institutional CFR = 2.2% • One case reported previously from Umzingwane district in Matabeleland South was a long distant truck driver who had travelled from Harare to Beitbridge and then to Bulawayo, develop signs and symptoms of Cholera at Mbalabala. Source: Ministry of Health and Child Welfare Rapid Disease Notification System 1 High priority districts to be investigated today Districts reported Districts with a Districts with high Districts with Districts which have not reported for more than 3 high number of daily CFR > 5% : number of deaths cases re- days: cases today (cases outside health occurring after added today> 30 facility/ CTC > 3 more than 14 days 1. -

Zimbabwean Government Gazette
ZIMBABWEAN GOVERNMENT GAZETTE Published by Authority Vol. LXVII, No. 29 2nd JUNE,1989 Price 40c General Notice 294 of 1989. (c) depart Harare Sunday 2 p.m., arrive Mudzi Kraal 7 p.m.; ROAD MOTOR TRANSPORTATION ACT [CHAPTER 262] | tet! (d) depart Mudzi Kraal Monday to Saturday 6 a.m., arrive i Applications in Connexion with Road Service Permits ‘ Harare 11.05 a.m.; (e) depart Mudzi Kraal 8 a.m., arrive Harare 1.25 p.m. IN terms of subsection (4) of section 7 of ‘the Road Motor Note.—This application is made to.reinstate permit 17567 eee - Transportation Act (Chupter 262], notice is hereby given that which expired on 30th September, 1988. the applications de‘ailed in the Schedule for the e issue or amendment of road service permits, have been received for the ' GOODS-VEHICLES awe consideration of the Controller of Road Motor Transportation. Additionals : Ary person wishing to object to any such application must K. M. Edwards. lodge with the Controller of Road Motor Transportation, P.O. Box 8332, Causeway— G/550 and 551/88. Two goods-vehicles. Load: 30000 kilo- (a) a notice, in writing, of his intention to object, so as to grams, each. reach the Controller’s Office not later than the 23rd Area: Within Mashonaland West Province, with access to June, 1989. _ Harare. (b) his objection and the grounds therefor, on form R.M.T. Nature of carriage: Goods, wares and merchandise of all kinds. 24, together with two copies thereof, so as to reachthe * Controller’s office not later than the 14th July, 1989. -

Revised HSS Annual Report 2013
ZIM-809-G14-S HEALTH SYSTEMS STRENGTHENING CROSS- CUTTING INTERVENTIONS Annual Report 2013 15 April 2014 TABLE CONTENTS 1 INTRODUCTION .................................................................................................................................... 2 OVERVIEW OF THE GRANT ........................................................................................................................... 2 2.1 BACKGROUND .................................................................................................................................................................................... 2 2.2 COMPONENTS OF THE GRANT ........................................................................................................................................................... 3 2.2.1 Health Retention Scheme ................................................................................................................................................ 3 2.2.2 Community Systems Strengthening (CSS) ................................................................................................................ 4 2.2.3 Health information Systems (HIS) ................................................................................................................................. 4 2.3 COORDINATION OF THE GRANT ........................................................................................................................................................ 5 ACTIVITIES IMPLEMENTED .......................................................................................................................... -

Zimbabwe – Cholera Outbreak
BUREAU FOR DEMOCRACY, CONFLICT, AND HUMANITARIAN ASSISTANCE (DCHA) OFFICE OF U.S. FOREIGN DISASTER ASSISTANCE (OFDA) Zimbabwe – Cholera Outbreak Fact Sheet #13, Fiscal Year (FY) 2009 April 2, 2009 Note: The last fact sheet was dated March 19, 2009. KEY DEVELOPMENTS • Since the cholera outbreak began in August 2008, the disease has spread to 60 of Zimbabwe’s 62 districts. As of April 1, nearly 94,300 reported cases of cholera had caused more than 4,100 deaths, according to the U.N. World Health Organization (WHO). On March 21, the total caseload exceeded 92,000 cases, the previous WHO estimate of the outbreak’s likeliest overall scope. • On April 1, WHO reported a sustained decline in the rates of cholera deaths and new cases over the past eight weeks. On March 27, the U.N. Office for the Coordination of Humanitarian Affairs (OCHA) stressed the ongoing need for vigilant surveillance and robust response activities despite the declining caseload countrywide. • On March 24, WHO recorded the first cholera case in Umzingwane District, Matabeleland South Province. To date, however, the organization has not reported additional cases in the district. NUMBERS AT A GLANCE SOURCE Total Reported Cholera Cases in Zimbabwe 94,277 WHO – April 1, 2009 Total Reported Cholera Deaths in Zimbabwe 4,127 WHO – April 1, 2009 FY 2009 HUMANITARIAN FUNDING Total USAID Humanitarian Assistance to Zimbabwe for the Cholera Outbreak ...........................................$7,305,529 CURRENT SITUATION • On March 30, WHO reported that the outbreak remained uncontrolled, despite the nationwide decline in the weekly rates of cholera deaths and new cases.