Cardiac Arrhythmias, Respiratory Failure, and Profound Hypokalemia in a Trauma Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Toluene Poisoning (Accidental Ingestion of Evostik) Summary
Toluene Poisoning (Accidental Ingestion of Evostik) *Solarin A.U1, Aremu E.O1, Gbelee O.H1, Animasahun A.B1, Akinola A.O1, Ogunlana A.T1, Nwakpele O.T1, Olugbade O1 1. Department of Paediatrics, Lagos State University Teaching Hospital, Ikeja Lagos. Corresponding Author: Solarin A.U. Email address: [email protected] Summary INTRODUCTION Childhood poisoning is one of the causes of high morbidity and mortality especially among under-five children in low income countries. The home and its surroundings may harbour poisonous substances which might be ingested by adventurous children. Evo-stik glue is a modified silane (MS) polymer based high performance adhesive. It contains toluene, a colourless, sweet-smelling liquid with detrimental effects on virtually every organ in the body especially brain and kidneys. Toluene is a component of household items such as gasoline, shoe and nail polish. AIM / OBJECTIVES From a few reported cases of toluene poisoning worldwide there was need to create awareness on the possibility of toluene poisoning as well as its deleterious effects. This is a case report on exposure to the effects of toluene by accidental ingestion that set the platform to emphasize the importance of prompt and appropriate management of toluene poisoning. METHODOLOGY This case report is about a 2year old girl who accidentally ingested 15-20ml evostik glue stored in an attractive container in the home. QH was presented at the Lagos State University Teaching Hospital Paediatric Emergency Unit with a one day history of persistent spontaneous, non-projectile and non-bilous vomiting. On admission, she was conscious, moderately dehydrated with dry buccal mucosa. -

Toxicological Profile for Toluene
TOXICOLOGICAL PROFILE FOR TOLUENE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Agency for Toxic Substances and Disease Registry September 2000 Additional Resources http://www.atsdr.cdc.gov/toxprofiles/tp56.html TOLUENE ii DISCLAIMER The use of company or product name(s) is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry. TOLUENE iii UPDATE STATEMENT Toxicological profiles are revised and republished as necessary, but no less than once every three years. For information regarding the update status of previously released profiles, contact ATSDR at: Agency for Toxic Substances and Disease Registry Division of Toxicology/Toxicology Information Branch 1600 Clifton Road NE, E-29 Atlanta, Georgia 30333 TOLUENE vi *Legislative Background The toxicological profiles are developed in response to the Superfund Amendments and Reauthorization Act (SARA) of 1986 (Public law 99-499) which amended the Comprehensive Environmental Response, Compensation, and Liability Act of 1980 (CERCLA or Superfund). This public law directed ATSDR to prepared toxicological profiles for hazardous substances most commonly found at facilities on the CERCLA National Priorities List and that pose the most significant potential threat to human health, as determined by ATSDR and the EPA. The availability of the revised priority list of 275 hazardous substances was announced in the Federal Register on October 21, 1999 (64 FR 56792). For prior versions of the list of substances, see Federal Register notices dated April 17, 1987 (52 FR 12866); October 20, 1988(53 FR 41280); October 26, 1989 (54 FR 43619); October 17, 1990 (55 FR 42067); October 17, 1991 (56 FR 52166); October 28, 1992 (57 FR 48801); February 28, 1994 (59 FR 9486); April 29, 1996 (61 FR 18744); and November 17, 1997 (62 FR 61332). -

Supranuclear and Internuclear Ocular Motility Disorders
CHAPTER 19 Supranuclear and Internuclear Ocular Motility Disorders David S. Zee and David Newman-Toker OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF THE MEDULLA THE SUPERIOR COLLICULUS Wallenberg’s Syndrome (Lateral Medullary Infarction) OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF Syndrome of the Anterior Inferior Cerebellar Artery THE THALAMUS Skew Deviation and the Ocular Tilt Reaction OCULAR MOTOR ABNORMALITIES AND DISEASES OF THE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN BASAL GANGLIA THE CEREBELLUM Parkinson’s Disease Location of Lesions and Their Manifestations Huntington’s Disease Etiologies Other Diseases of Basal Ganglia OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN THE PONS THE CEREBRAL HEMISPHERES Lesions of the Internuclear System: Internuclear Acute Lesions Ophthalmoplegia Persistent Deficits Caused by Large Unilateral Lesions Lesions of the Abducens Nucleus Focal Lesions Lesions of the Paramedian Pontine Reticular Formation Ocular Motor Apraxia Combined Unilateral Conjugate Gaze Palsy and Internuclear Abnormal Eye Movements and Dementia Ophthalmoplegia (One-and-a-Half Syndrome) Ocular Motor Manifestations of Seizures Slow Saccades from Pontine Lesions Eye Movements in Stupor and Coma Saccadic Oscillations from Pontine Lesions OCULAR MOTOR DYSFUNCTION AND MULTIPLE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN SCLEROSIS THE MESENCEPHALON OCULAR MOTOR MANIFESTATIONS OF SOME METABOLIC Sites and Manifestations of Lesions DISORDERS Neurologic Disorders that Primarily Affect the Mesencephalon EFFECTS OF DRUGS ON EYE MOVEMENTS In this chapter, we survey clinicopathologic correlations proach, although we also discuss certain metabolic, infec- for supranuclear ocular motor disorders. The presentation tious, degenerative, and inflammatory diseases in which su- follows the schema of the 1999 text by Leigh and Zee (1), pranuclear and internuclear disorders of eye movements are and the material in this chapter is intended to complement prominent. -

Toluene Toxicity
Case Studies in Environmental Medicine Course: SS3061 Date: February 2001 Original Date: August 1993 Expiration Date: February 28, 2007 TOLUENE TOXICITY Environmental Alert Use of toluene is increasing, in part because of its popularity as a solvent replacement for benzene. Gasoline contains 5% to 7% toluene by weight, making toluene a common airborne contaminant in industrialized countries. Many organic solvents have great addictive potential; toluene is the most commonly abused hydrocarbon solvent, primarily through “glue sniffing.” This monograph is one in a series of self- instructional publications designed to increase the primary care provider’s knowledge of hazardous substances in the environment and to aid in the evaluation of potentially exposed patients. This course is also available on the ATSDR Web site, www.atsdr.cdc.gov/HEC/CSEM/. See page 3 for more information about continuing medical education credits, continuing nursing education units, and continuing education units. U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Agency for Toxic Substances and Disease Registry Division of Toxicology and Environmental Medicine Toluene Toxicity Table of Contents ATSDR/DHEP Authors: Kim Gehle, MD, MPH; Felicia Pharagood-Wade, MD; Darlene Case Study ......................................................................................... 5 Johnson, RN, BSN, MA; Lourdes Who’s At Risk .................................................................................... 5 Rosales-Guevara, MD ATSDR/DHEP Revision Planners: Exposure Pathways ........................................................................... -

Inhalant Abuse: a Volatile Research Agenda
National Institute on Drug Abuse RESEARCH MONOGRAPH SERIES Inhalant Abuse: A Volatile Research Agenda 129 U.S. Department of Health and Human Services • Public Health Service • National Institutes of Health Inhalant Abuse: A Volatile Research Agenda Editors: Charles Wm. Sharp, Ph.D. Fred Beauvais, Ph.D. Richard Spence, Ph.D. NIDA Research Monograph 129 1992 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 ACKNOWLEDGMENT This monograph is based on the papers from a technical review on “Inhalant Abuse” held in 1989. The review meeting was sponsored by the National Institute on Drug Abuse and the Texas Commission on Alcohol and Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other material in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. Citation of the source is appreciated. Opinions expressed in this volume are those of the authors and do not necessarily reflect the opinions or official policy of the National Institute on Drug Abuse or any other part of the Department of Health and Human Services. The U.S. Government does not endorse or favor any specific commercial product or company. -

IJPP Hemotology 9-2-08
2009; 11(1) : 1 INDIAN JOURNAL OF IJPP PRACTICAL PEDIATRICS • • IJPP is a quarterly subscription journal of the Indian Academy of Pediatrics committed to presenting practical pediatric issues and management updates in a simple and clear manner • • Indexed in Excerpta Medica, CABI Publishing. Vol.11 No.1 JAN.-MAR.2009 Dr. K.Nedunchelian Dr. S. Thangavelu Editor-in-Chief Executive Editor CONTENTS FROM THE EDITOR'S DESK 3 TOPIC OF INTEREST - TOXICOLOGY Organophosphate, carbamate and rodenticide poisoning 6 - Rajendiran C, Ravi G, Thirumalaikolundu Subramanian P Hydrocarbon and related compounds poisoning 15 - Utpal Kant Singh, Prasad R, Gaurav A Common drug poisoning 22 - Suresh Gupta Corrosive poisoning 37 - Jayanthi Ramesh House hold material poisoning 41 - Shuba S, Betty Chacko Cardiotoxins 53 - Rashmi Kapoor Narcotic poisoning 64 - Kala Ebinazer Journal Office and address for communications: Dr. K.Nedunchelian, Editor-in-Chief, Indian Journal of Practical Pediatrics, 1A, Block II, Krsna Apartments, 50, Halls Road, Egmore, Chennai - 600 008. Tamil Nadu, India. Tel.No. : 044-28190032 E.mail : [email protected] 1 Indian Journal of Practical Pediatrics 2009; 11(1) : 2 GENERAL ARTICLES Intrauterine growth retardation : Journey from conception to late adulthood 68 - Neelam Kler, Naveen Gupta Child adoption 82 - Ganesh R, Suresh N, Eswara Raja T, Lalitha Janakiraman, Vasanthi T DERMATOLOGY Ichthyosis - An approach 86 - Anandan V PICTURE QUIZ 91 RADIOLOGIST TALKS TO YOU Disorders of ventral induction and similar conditions - I 92 - Vijayalakshmi G, Elavarasu E, Vijayalakshmi M, Venkatesan MD CASE STUDY Unusual complication of nasogastric tube insertion in a child 95 - Poovazhagi V, Shanthi S, Vijayaraghavan A, Kulandai Kasturi R Congenital miliary tuberculosis 97 - Vijayakumari, Suresh DV CLIPPINGS 14,21,52,63,81,94 NEWS AND NOTES 85,90 FOR YOUR KIND ATTENTION * The views expressed by the authors do not necessarily reflect those of the sponsor or publisher. -

Draft for Review Volume 3 Health and Safety Plan Site Wide Groundwater (Operable Unit 03) West Lake Landfill Site Bridgeton, Missouri
DRAFT FOR REVIEW VOLUME 3 HEALTH AND SAFETY PLAN SITE WIDE GROUNDWATER (OPERABLE UNIT 03) WEST LAKE LANDFILL SITE BRIDGETON, MISSOURI June 5, 2019 Project #: 63N-001-001 SUBMITTED BY: Trihydro Corporation 1252 Commerce Drive, Laramie, WY 82070 DRAFT memorandum To: West Lake OU-3 Project-Team Members From: Mr. Stephen L Lombardo, P.G. Date: June 5, 2019 Re: Health and Safety Plan (HASP) Orientation The purpose of this memorandum is to provide project-team members (specifically field team employees) with a Health and Safety Plan (HASP) orientation, including a summary of the project, its common hazards, minimum personal protective equipment (PPE) required, other relevant safety concerns, plus policies and practices unique to the site. Since project history affects information presented to project team members, this orientation is an evergreen document and should be updated as the project progresses. Lessons learned and hazards identified will be documented during daily tailgate safety meetings, recorded on Job Safety Analyses (JSAs) and memorialized in the HASP. This memo must be read in conjunction with the site-specific HASP, which contains detailed site hazard and response information. INTRODUCTION The Site was added to the Superfund National Priorities List (NPL) in 1990 and consists of three Operable Units (OUs) including former industrial and municipal waste cells and groundwater. Operable Unit 1 (OU-1) includes former waste disposal areas Radiological Area 1 (Area 1) and Radiological Area 2 (Area 2) where radiological impacted materials (RIM) exist (EPA ID#MOD079900932). Operable Unit 2 (OU-2) has no areas impacted with RIM and includes the closed construction and demolition (C&D) cell, inactive sanitary landfill, and the North and South Quarry Portions of the Bridgeton Landfill. -

Chapter 73 1009
C h a p t e r 73 Fluid and Electrolyte Issues in Pediatric Critical Illness Robert Lynch, Ellen Glenn Wood, and Tara M. Neumayr intraoperative fluids influence acid-base and electrolyte status, PEARLS particularly of vulnerable patients.4 The choice of Na+ content • Hypotonic maintenance IV fluids are associated with mild to and balancing ions of IVF for postoperative or critical care moderate hyponatremia in postoperative patients. maintenance may be important for some patients thus justify- Anesthesia, stress, and inflammatory mediators probably ing additional expense. Clearly 0.18 and 0.225 mM saline is 5,6 contribute. Electrolyte monitoring in patients at risk is associated with a higher incidence of mild hyponatremia, essential for detection and management of the occasional although controlled trials do not show this effect for 0.46 mM 7,8 patient who develops severe hyponatremia. This critical saline. Severe hyponatremia has been associated with pul- effect of the syndrome of inappropriate antidiuretic hormone monary or CNS illness in pediatrics and is infrequent even may occur even in patients on isotonic IV fluids. within those categories, with the exception of children with • Medical patients with high levels of inflammatory mediators traumatic brain injury (TBI). Among patients with those and appear to be at increased risk of significant hyponatremia. other illnesses, the evolving study of the influence of inflam- Interleukin effects on antidiuretic hormone release may matory mediators directly on the hypothalamus and indirectly contribute. on vasopressin secretion may further clarify which patients are 9,10 • Albumin infusions have been generally safe but may at most risk of clinically significant hyponatremia. -
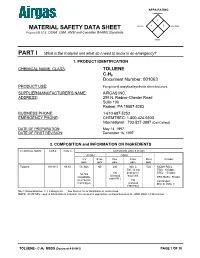
MATERIAL SAFETY DATA SHEET HEALTH 2 REACTIVITY Prepared to U.S
NFPA RATING FLAMMABILITY 3 0 MATERIAL SAFETY DATA SHEET HEALTH 2 REACTIVITY Prepared to U.S. OSHA, CMA, ANSI and Canadian WHMIS Standards OTHER PART I What is the material and what do I need to know in an emergency? 1. PRODUCT IDENTIFICATION CHEMICAL NAME; CLASS: TOLUENE C7H8 Document Number: 001063 PRODUCT USE: For general analytical/synthetic chemical uses. SUPPLIER/MANUFACTURER'S NAME: AIRGAS INC. ADDRESS: 259 N. Radnor-Chester Road Suite 100 Radnor, PA 19087-5283 BUSINESS PHONE: 1-610-687-5253 EMERGENCY PHONE: CHEMTREC: 1-800-424-9300 International: 703-527-3887 (Call Collect) DATE OF PREPARATION: May 14, 1997 DATE OF FIRST REVISION: December 16, 1997 2. COMPOSITION and INFORMATION ON INGREDIENTS CHEMICAL NAME CAS # mole % EXPOSURE LIMITS IN AIR ACGIH OSHA TLV STEL PEL STEL IDLH OTHER ppm ppm ppm ppm ppm Toluene 108-88-3 99.9% 50, Skin NE 200 300, C 500 NIOSH RELs: 500, 10 min TWA: 100 ppm 100 peak per 8 STEL: 150 ppm A4, Not (Vacated hour shift Classifiable DFG MAKs: 50 ppm 1989 PEL) as a Human 150 Carcinogen: Carcinogen (Vacated EPA-D IARC-3 1989 PEL) NE = Not Established C = Ceiling Limit See Section 16 for Definitions of Terms Used. NOTE: All WHMIS required information is included. It is located in appropriate sections based on the ANSI Z400.1-1993 format. TOLUENE - C7H8 MSDS (Document # 001063) PAGE 1 OF 10 3. HAZARD IDENTIFICATION EMERGENCY OVERVIEW: Toluene is a colorless, flammable, toxic liquid, with gasoline-like odor. Inhalation of vapors of Toluene can affect the central nervous system. -
Difficulties in Management of Occupational Exposure in Our
96 CASE REPORT OLGU SUNUMU Difficulties in Management of Occupational Exposure in Our Country: A Case Report Ülkemizde Mesleksel Maruziyet Durumunun Yönetilmesinde Yaşanan Güçlükler: Bir Olgu Sunumu Serkan YILMAZ, Murat PEKDEMİR, Elif YAKA Department of Emergency Medicine, Kocaeli University Faculty of Medicine, Kocaeli, Turkey SUMMARY ÖZET Occupational exposure to hazardous materials is a serious problem Mesleki maruziyet gelişmekte olan ülkelerde, ciddi ancak yete- in developing countries. Unfortunately, the different presentations rince kayıtlara geçirilememiş bir sorundur. Sıklıkla nonspesifik result in nonspecific clinical syndromes, making diagnosis difficult. semptomlarla başvuran bu hastaların tanı ve tedavisinde birçok We discuss lessons learned during the assessment and treatment güçlük yaşanmaktadır. Bu makale, bir mesleki maruziyet vaka- of occupational exposure in two industrial workers. Two employees sının değerlendirmesi sırasında elde edilen deneyimlerin payla- of a facility that manufactures plastic floor covering were admit- şılması amacıyla hazırlanmıştır. Plastik yer döşemeleri üretimin- ted to the emergency department with complaints including in- de çalışan iki işçi yürüyememe, uyuşukluk ve baş dönmesi, bilinç ability to ambulate, lethargy and dizziness. It was thought that the bulanıklığı gibi yakınmalarla acil servise başvurdu. Her iki hasta- patients’ neurological symptoms resulted from toxic encephalitis da da nörolojik semptomlara yol açan toksik ensefalit ve direnç- and refractory hypokalemia due to renal medullary -

Environmental Health Criteria 52 TOLUENE
Environmental Health Criteria 52 TOLUENE Please note that the layout and pagination of this web version are not identical with the printed version. Toluene (EHC 52, 1986) INTERNATIONAL PROGRAMME ON CHEMICAL SAFETY ENVIRONMENTAL HEALTH CRITERIA 52 TOLUENE This report contains the collective views of an international group of experts and does not necessarily represent the decisions or the stated policy of the United Nations Environment Programme, the International Labour Organisation, or the World Health Organization. Published under the joint sponsorship of the United Nations Environment Programme, the International Labour Organisation, and the World Health Organization World Health Orgnization Geneva, 1985 The International Programme on Chemical Safety (IPCS) is a joint venture of the United Nations Environment Programme, the International Labour Organisation, and the World Health Organization. The main objective of the IPCS is to carry out and disseminate evaluations of the effects of chemicals on human health and the quality of the environment. Supporting activities include the development of epidemiological, experimental laboratory, and risk-assessment methods that could produce internationally comparable results, and the development of manpower in the field of toxicology. Other activities carried out by the IPCS include the development of know-how for coping with chemical accidents, coordination of laboratory testing and epidemiological studies, and promotion of research on the mechanisms of the biological action of chemicals. ISBN 92 4 154192 X The World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and enquiries should be addressed to the Office of Publications, World Health Organization, Geneva, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations Page 1 of 104 Toluene (EHC 52, 1986) already available. -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD June 2017 CONTENTS General Toxicology 9 Metals 34 Management 17 Pesticides 35 Drugs 19 Chemical Warfare 36 Chemical Incidents & 28 Plants 36 Pollution Chemicals 29 Animals 37 CURRENT AWARENESS PAPERS OF THE MONTH Is mannitol the treatment of choice for patients with ciguatera fish poisoning? Mullins ME, Hoffman RS. Clin Toxicol 2017; online early: doi: 10.1080/15563650.2017.1327664: Context Ciguatera fish poisoning arises primarily from consumption of carnivorous reef fish caught in tropical and sub-tropical waters. Ciguatoxins, a class of tasteless, heat-stable, polycyclic toxins produced by dinoflagellates, accumulate through the food chain and concentrate in various carnivorous fish, such as groupers, barracudas, wrasses, amberjack, kingfishes, and eels. Characteristics of ciguatera fish poisoning include early nausea, vomiting, and diarrhea in the first one to two days post ingestion, followed by the appearance of sensory disturbances. The classic dysaesthesia is cold allodynia, often described as reversal of hot and cold sensation, but a more accurate description is burning pain on exposure to cold. Objective To discuss and appraise the evidence regarding the use of mannitol or other drugs in treating ciguatera framed in the historical context of the last four decades. Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England 2 Methods We searched PubMed and Embase for all years from 1966 to March 31, 2017 with search terms "ciguatera", "mannitol", and "treatment".