Inhalant Abuse: a Volatile Research Agenda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cambridge International Examinations Cambridge Ordinary Level
Cambridge International Examinations Cambridge Ordinary Level HISTORY 2158/13 Paper 1 World Affairs, 1917–1991 May/June 2014 2 hours 30 minutes Additional Materials: Answer Booklet/Paper *9722304068* READ THESE INSTRUCTIONS FIRST If you have been given an Answer Booklet, follow the instructions on the front cover of the Booklet. Write your Centre number, candidate number and name on all the work you hand in. Write in dark blue or black pen. You may use an HB pencil for any diagrams, graphs or rough working. Do not use staples, paper clips, glue or correction fluid. DO NOT WRITE IN ANY BARCODES. Answer five questions. Section A Answer at least one question from this Section. Sections B to F Answer questions from at least two of these Sections. All questions in this paper carry equal marks. The first part of each question is worth 14 marks and the last part is worth 6 marks. Answer each part of the questions chosen as fully as you can. At the end of the examination, fasten all your work securely together. This document consists of 7 printed pages and 1 blank page. DC (LK) 90309 © UCLES 2014 [Turn over 2 Section A International Relations and Developments 1 Describe how the Treaty of Versailles: (a) changed the European borders of Germany; (b) brought Germany’s colonial empire to an end. How far do you agree that Germany was not treated fairly by the terms of the Treaty of Versailles? 2 Describe the main features of: (a) Mussolini’s conquest of Abyssinia in 1935–36; (b) Hitler’s taking of Austria and Czechoslovakia in 1938–39. -

Toluene Poisoning (Accidental Ingestion of Evostik) Summary
Toluene Poisoning (Accidental Ingestion of Evostik) *Solarin A.U1, Aremu E.O1, Gbelee O.H1, Animasahun A.B1, Akinola A.O1, Ogunlana A.T1, Nwakpele O.T1, Olugbade O1 1. Department of Paediatrics, Lagos State University Teaching Hospital, Ikeja Lagos. Corresponding Author: Solarin A.U. Email address: [email protected] Summary INTRODUCTION Childhood poisoning is one of the causes of high morbidity and mortality especially among under-five children in low income countries. The home and its surroundings may harbour poisonous substances which might be ingested by adventurous children. Evo-stik glue is a modified silane (MS) polymer based high performance adhesive. It contains toluene, a colourless, sweet-smelling liquid with detrimental effects on virtually every organ in the body especially brain and kidneys. Toluene is a component of household items such as gasoline, shoe and nail polish. AIM / OBJECTIVES From a few reported cases of toluene poisoning worldwide there was need to create awareness on the possibility of toluene poisoning as well as its deleterious effects. This is a case report on exposure to the effects of toluene by accidental ingestion that set the platform to emphasize the importance of prompt and appropriate management of toluene poisoning. METHODOLOGY This case report is about a 2year old girl who accidentally ingested 15-20ml evostik glue stored in an attractive container in the home. QH was presented at the Lagos State University Teaching Hospital Paediatric Emergency Unit with a one day history of persistent spontaneous, non-projectile and non-bilous vomiting. On admission, she was conscious, moderately dehydrated with dry buccal mucosa. -

Toxicological Profile for Toluene
TOXICOLOGICAL PROFILE FOR TOLUENE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Agency for Toxic Substances and Disease Registry September 2000 Additional Resources http://www.atsdr.cdc.gov/toxprofiles/tp56.html TOLUENE ii DISCLAIMER The use of company or product name(s) is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry. TOLUENE iii UPDATE STATEMENT Toxicological profiles are revised and republished as necessary, but no less than once every three years. For information regarding the update status of previously released profiles, contact ATSDR at: Agency for Toxic Substances and Disease Registry Division of Toxicology/Toxicology Information Branch 1600 Clifton Road NE, E-29 Atlanta, Georgia 30333 TOLUENE vi *Legislative Background The toxicological profiles are developed in response to the Superfund Amendments and Reauthorization Act (SARA) of 1986 (Public law 99-499) which amended the Comprehensive Environmental Response, Compensation, and Liability Act of 1980 (CERCLA or Superfund). This public law directed ATSDR to prepared toxicological profiles for hazardous substances most commonly found at facilities on the CERCLA National Priorities List and that pose the most significant potential threat to human health, as determined by ATSDR and the EPA. The availability of the revised priority list of 275 hazardous substances was announced in the Federal Register on October 21, 1999 (64 FR 56792). For prior versions of the list of substances, see Federal Register notices dated April 17, 1987 (52 FR 12866); October 20, 1988(53 FR 41280); October 26, 1989 (54 FR 43619); October 17, 1990 (55 FR 42067); October 17, 1991 (56 FR 52166); October 28, 1992 (57 FR 48801); February 28, 1994 (59 FR 9486); April 29, 1996 (61 FR 18744); and November 17, 1997 (62 FR 61332). -

Supranuclear and Internuclear Ocular Motility Disorders
CHAPTER 19 Supranuclear and Internuclear Ocular Motility Disorders David S. Zee and David Newman-Toker OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF THE MEDULLA THE SUPERIOR COLLICULUS Wallenberg’s Syndrome (Lateral Medullary Infarction) OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF Syndrome of the Anterior Inferior Cerebellar Artery THE THALAMUS Skew Deviation and the Ocular Tilt Reaction OCULAR MOTOR ABNORMALITIES AND DISEASES OF THE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN BASAL GANGLIA THE CEREBELLUM Parkinson’s Disease Location of Lesions and Their Manifestations Huntington’s Disease Etiologies Other Diseases of Basal Ganglia OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN THE PONS THE CEREBRAL HEMISPHERES Lesions of the Internuclear System: Internuclear Acute Lesions Ophthalmoplegia Persistent Deficits Caused by Large Unilateral Lesions Lesions of the Abducens Nucleus Focal Lesions Lesions of the Paramedian Pontine Reticular Formation Ocular Motor Apraxia Combined Unilateral Conjugate Gaze Palsy and Internuclear Abnormal Eye Movements and Dementia Ophthalmoplegia (One-and-a-Half Syndrome) Ocular Motor Manifestations of Seizures Slow Saccades from Pontine Lesions Eye Movements in Stupor and Coma Saccadic Oscillations from Pontine Lesions OCULAR MOTOR DYSFUNCTION AND MULTIPLE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN SCLEROSIS THE MESENCEPHALON OCULAR MOTOR MANIFESTATIONS OF SOME METABOLIC Sites and Manifestations of Lesions DISORDERS Neurologic Disorders that Primarily Affect the Mesencephalon EFFECTS OF DRUGS ON EYE MOVEMENTS In this chapter, we survey clinicopathologic correlations proach, although we also discuss certain metabolic, infec- for supranuclear ocular motor disorders. The presentation tious, degenerative, and inflammatory diseases in which su- follows the schema of the 1999 text by Leigh and Zee (1), pranuclear and internuclear disorders of eye movements are and the material in this chapter is intended to complement prominent. -

5849622628* Electronic Calculator
UNIVERSITY OF CAMBRIDGE INTERNATIONAL EXAMINATIONS General Certificate of Education Advanced Level THINKING SKILLS 9694/31 Paper 3 Problem Analysis and Solution May/June 2012 1 hour 30 minutes Additional Materials: Answer Booklet/Paper *5849622628* Electronic Calculator READ THESE INSTRUCTIONS FIRST If you have been given an Answer Booklet, follow the instructions on the front cover of the booklet. Write your Centre number, candidate number and name on all the work you hand in. Write in dark blue or black pen. Do not use staples, paper clips, highlighters, glue or correction fluid. DO NOT WRITE ON ANY BARCODES. Calculators should be used where appropriate. Answer all the questions. Start each question on a new answer sheet. At the end of the examination, fasten all your work securely together. The number of marks is given in brackets [ ] at the end of each question or part question. This document consists of 8 printed pages and 4 blank pages. IB12 06_9694_31/4RP © UCLES 2012 [Turn over 2 1 Study the information below and answer the questions. Show your working. The gold ducat is a coin currently worth 40 silver pennies, but, because of the scarcity of gold, King Offa is going to decree an increase in its value relative to the silver penny. Ethelred knows that this will be done overnight on one of the next four nights (Mon, Tue, Wed, Thu), and that the value will go up once by 1, 2, or 3 pennies. All possibilities are equally likely. Ethelred only has 30 silver pennies. He could get one or more overnight loans, but it costs a half penny to get a loan of 10 pennies from one day to the next. -

Toluene Toxicity
Case Studies in Environmental Medicine Course: SS3061 Date: February 2001 Original Date: August 1993 Expiration Date: February 28, 2007 TOLUENE TOXICITY Environmental Alert Use of toluene is increasing, in part because of its popularity as a solvent replacement for benzene. Gasoline contains 5% to 7% toluene by weight, making toluene a common airborne contaminant in industrialized countries. Many organic solvents have great addictive potential; toluene is the most commonly abused hydrocarbon solvent, primarily through “glue sniffing.” This monograph is one in a series of self- instructional publications designed to increase the primary care provider’s knowledge of hazardous substances in the environment and to aid in the evaluation of potentially exposed patients. This course is also available on the ATSDR Web site, www.atsdr.cdc.gov/HEC/CSEM/. See page 3 for more information about continuing medical education credits, continuing nursing education units, and continuing education units. U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Agency for Toxic Substances and Disease Registry Division of Toxicology and Environmental Medicine Toluene Toxicity Table of Contents ATSDR/DHEP Authors: Kim Gehle, MD, MPH; Felicia Pharagood-Wade, MD; Darlene Case Study ......................................................................................... 5 Johnson, RN, BSN, MA; Lourdes Who’s At Risk .................................................................................... 5 Rosales-Guevara, MD ATSDR/DHEP Revision Planners: Exposure Pathways ........................................................................... -

Appendix D: Important Facts About Alcohol and Drugs
APPENDICES APPENDIX D. IMPORTANT FACTS ABOUT ALCOHOL AND DRUGS Appendix D outlines important facts about the following substances: $ Alcohol $ Cocaine $ GHB (gamma-hydroxybutyric acid) $ Heroin $ Inhalants $ Ketamine $ LSD (lysergic acid diethylamide) $ Marijuana (Cannabis) $ MDMA (Ecstasy) $ Mescaline (Peyote) $ Methamphetamine $ Over-the-counter Cough/Cold Medicines (Dextromethorphan or DXM) $ PCP (Phencyclidine) $ Prescription Opioids $ Prescription Sedatives (Tranquilizers, Depressants) $ Prescription Stimulants $ Psilocybin $ Rohypnol® (Flunitrazepam) $ Salvia $ Steroids (Anabolic) $ Synthetic Cannabinoids (“K2”/”Spice”) $ Synthetic Cathinones (“Bath Salts”) PAGE | 53 Sources cited in this Appendix are: $ Drug Enforcement Administration’s Drug Facts Sheets1 $ Inhalant Addiction Treatment’s Dangers of Mixing Inhalants with Alcohol and Other Drugs2 $ National Institute on Alcohol Abuse and Alcoholism’s (NIAAA’s) Alcohol’s Effects on the Body3 $ National Institute on Drug Abuse’s (NIDA’s) Commonly Abused Drugs4 $ NIDA’s Treatment for Alcohol Problems: Finding and Getting Help5 $ National Institutes of Health (NIH) National Library of Medicine’s Alcohol Withdrawal6 $ Rohypnol® Abuse Treatment FAQs7 $ Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) Keeping Youth Drug Free8 $ SAMHSA’s Center for Behavioral Health Statistics and Quality’s (CBHSQ’s) Results from the 2015 National Survey on Drug Use and Health: Detailed Tables9 The substances that are considered controlled substances under the Controlled Substances Act (CSA) are divided into five schedules. An updated and complete list of the schedules is published annually in Title 21 Code of Federal Regulations (C.F.R.) §§ 1308.11 through 1308.15.10 Substances are placed in their respective schedules based on whether they have a currently accepted medical use in treatment in the United States, their relative abuse potential, and likelihood of causing dependence when abused. -

Impact of Drug Use on the Street Children 11
National Institute of Social Defence (NISD) A Trainer’s Manual on drug use prevention, treatment and care for street children A Trainer’s Manual on drug use prevention, treatment and care for street children National Institute of Social Defence (NISD) A Trainer’s Manual on Drug Use Prevention, Treatment and Care for Street Children Acknowledgments Acknowledgments We are grateful to Shri Chaitanya Murty- Director NISD, Ministry of Social Justice & Empowerment, We are grateful to Shri Chaitanya Murty- Director NISD, Ministry of Social Justice & Empowerment, Government of India, Ms. Cristina Albertin, Representative, UNODC, ROSA & Mr. Sunil Kumar, Government of India, Ms. Cristina Albertin, Representative, UNODC, ROSA & Mr. Sunil Kumar, Deputy Director, NCDAP-NISD, Ministry of Social Justice and Empowerment, Government of India for Deputy Director, NCDAP-NISD, Ministry of Social Justice and Empowerment, Government of India for their guidance and support. their guidance and support. Our sincere thanks to the authors: Our sincere thanks to the authors: Dr. Anju Dhawan- National Drug Dependence Treatment Centre, AIIMS Dr. Anju Dhawan- All India Institute of Medical Sciences, New Delhi Dr. Shekhar Sheshadri- NIMHANS Dr. Shekhar Sheshadri- National Institute of Mental Health and Neuro Sciences, Bangalore Ms. Rita Panicker- Butterflies Ms. Rita Panicker- Butterflies, New Delhi Dr. Koushik Sinha Deb- Department of Psychiatry and National Drug Dependence Treatment Centre, AIIMS Dr. Koushik Sinha Deb- All India Institute of Medical Sciences, New Delhi Dr. Prashanth.R- Department of Psychiatry and National Drug Dependence Treatment Centre, AIIMS Dr. Prashanth.R- All India Institute of Medical Sciences, New Delhi Mr. Raj Kumar Raju- Indian Harm Reduction Network Mr. -

IJPP Hemotology 9-2-08
2009; 11(1) : 1 INDIAN JOURNAL OF IJPP PRACTICAL PEDIATRICS • • IJPP is a quarterly subscription journal of the Indian Academy of Pediatrics committed to presenting practical pediatric issues and management updates in a simple and clear manner • • Indexed in Excerpta Medica, CABI Publishing. Vol.11 No.1 JAN.-MAR.2009 Dr. K.Nedunchelian Dr. S. Thangavelu Editor-in-Chief Executive Editor CONTENTS FROM THE EDITOR'S DESK 3 TOPIC OF INTEREST - TOXICOLOGY Organophosphate, carbamate and rodenticide poisoning 6 - Rajendiran C, Ravi G, Thirumalaikolundu Subramanian P Hydrocarbon and related compounds poisoning 15 - Utpal Kant Singh, Prasad R, Gaurav A Common drug poisoning 22 - Suresh Gupta Corrosive poisoning 37 - Jayanthi Ramesh House hold material poisoning 41 - Shuba S, Betty Chacko Cardiotoxins 53 - Rashmi Kapoor Narcotic poisoning 64 - Kala Ebinazer Journal Office and address for communications: Dr. K.Nedunchelian, Editor-in-Chief, Indian Journal of Practical Pediatrics, 1A, Block II, Krsna Apartments, 50, Halls Road, Egmore, Chennai - 600 008. Tamil Nadu, India. Tel.No. : 044-28190032 E.mail : [email protected] 1 Indian Journal of Practical Pediatrics 2009; 11(1) : 2 GENERAL ARTICLES Intrauterine growth retardation : Journey from conception to late adulthood 68 - Neelam Kler, Naveen Gupta Child adoption 82 - Ganesh R, Suresh N, Eswara Raja T, Lalitha Janakiraman, Vasanthi T DERMATOLOGY Ichthyosis - An approach 86 - Anandan V PICTURE QUIZ 91 RADIOLOGIST TALKS TO YOU Disorders of ventral induction and similar conditions - I 92 - Vijayalakshmi G, Elavarasu E, Vijayalakshmi M, Venkatesan MD CASE STUDY Unusual complication of nasogastric tube insertion in a child 95 - Poovazhagi V, Shanthi S, Vijayaraghavan A, Kulandai Kasturi R Congenital miliary tuberculosis 97 - Vijayakumari, Suresh DV CLIPPINGS 14,21,52,63,81,94 NEWS AND NOTES 85,90 FOR YOUR KIND ATTENTION * The views expressed by the authors do not necessarily reflect those of the sponsor or publisher. -
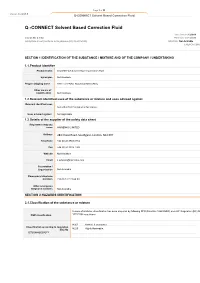
Q -CONNECT Solvent Based Correction Fluid
Page 1 of 11 Version No: 2.1.1.1 Q-CONNECT Solvent Based Correction Fluid Q -CONNECT Solvent Based Correction Fluid 3 Issue Date:01/12/2018 Version No: 2.1.1.2 Print Date: 01/12/2018 Safety Data Sheet (Conforms to Regulations (EC) No 2015/830) Initial Date: Not Available S.REACH.GBR.E SECTION 1 IDENTIFICATION OF THE SUBSTANCE / MIXTURE AND OF THE COMPANY / UNDERTAKING 1.1.Product Identifier Product name Q CONNECT Solvent Based Correction Fluid Synonyms Not Available Proper shipping name PAINT or PAINT RELATED MATERIAL Other means of identification Not Available 1.2.Relevant identified uses of the substance or mixture and uses advised against Relevant identified uses Correction fluid for paper or fax copies. Uses advised against Not Applicable 1.3.Details of the supplier of the safety data sheet Registered company name HAINENKO LIMITED Address 284 Chase Road, Southgate, London, N14 6HF Telephone +44 (0) 20 8882 8734 Fax +44 (0) 20 8882 7749 Website Not Available Email [email protected] Association / Organisation Not Available Emergency telephone numbers +33 (0) 3 27 23 64 00 Other emergency telephone numbers Not Available SECTION 2 HAZARDS IDENTIFICATION 2.1.Classification of the substance or mixture In case of mixtures, classification has been prepared by following DPD (Directive 1999/45/EC) and CLP Regulation (EC) No DSD classification 1272/2008 regulations H302 Harmful if swallowed. Classification according to regulation H225 Highly flammable. (EC) No 1272/2008 [CLP] [1]] Page 2 of 11 Version No: 2.1.1.1 Q-CONNECT Solvent Based Correction Fluid Flammable Liquid Category 2, Acute Toxicity (Oral) Category 4, Aspiration Hazard Category 1, Chronic Aquatic Hazard Category 2 Contains less than 0,1% benzene – (CLP) is applicable. -

Draft for Review Volume 3 Health and Safety Plan Site Wide Groundwater (Operable Unit 03) West Lake Landfill Site Bridgeton, Missouri
DRAFT FOR REVIEW VOLUME 3 HEALTH AND SAFETY PLAN SITE WIDE GROUNDWATER (OPERABLE UNIT 03) WEST LAKE LANDFILL SITE BRIDGETON, MISSOURI June 5, 2019 Project #: 63N-001-001 SUBMITTED BY: Trihydro Corporation 1252 Commerce Drive, Laramie, WY 82070 DRAFT memorandum To: West Lake OU-3 Project-Team Members From: Mr. Stephen L Lombardo, P.G. Date: June 5, 2019 Re: Health and Safety Plan (HASP) Orientation The purpose of this memorandum is to provide project-team members (specifically field team employees) with a Health and Safety Plan (HASP) orientation, including a summary of the project, its common hazards, minimum personal protective equipment (PPE) required, other relevant safety concerns, plus policies and practices unique to the site. Since project history affects information presented to project team members, this orientation is an evergreen document and should be updated as the project progresses. Lessons learned and hazards identified will be documented during daily tailgate safety meetings, recorded on Job Safety Analyses (JSAs) and memorialized in the HASP. This memo must be read in conjunction with the site-specific HASP, which contains detailed site hazard and response information. INTRODUCTION The Site was added to the Superfund National Priorities List (NPL) in 1990 and consists of three Operable Units (OUs) including former industrial and municipal waste cells and groundwater. Operable Unit 1 (OU-1) includes former waste disposal areas Radiological Area 1 (Area 1) and Radiological Area 2 (Area 2) where radiological impacted materials (RIM) exist (EPA ID#MOD079900932). Operable Unit 2 (OU-2) has no areas impacted with RIM and includes the closed construction and demolition (C&D) cell, inactive sanitary landfill, and the North and South Quarry Portions of the Bridgeton Landfill. -

Solvents/Inhalants Information for Health Professionals
Solvents/Inhalants Information for Health Professionals Introduction Inhalants compromise a wide variety of vapours, gases, and aerosols that can be inhaled to induce psychoactive (mind-altering) effects. Unlike other drugs, inhalants are available as legal products with low costs and wide availability. Examples include commercial products such as nail polish remover, hair sprays, lighter fluid, cleaning fluids, vegetable frying pan lubricants, and spray paints. These chemicals can be sniffed or inhaled because they are gaseous at room temperature and pressure. “Inhalant” is a general term that includes all substances used in this way. Most inhalants are volatile solvents, which are liquids that easily vaporize at room temperature and can contain many different chemicals that may be psychoactive. The majority of these solvents are produced from petroleum and natural gas. They have an enormous number of industrial, commercial and household uses, and are found in automobile fuels, cleaning fluids, toiletries, adhesives and fillers, paints, paint thinners, felt-tip markers, and many other products. In addition to volatile solvents, aerosols (hair spray, paint spray) can be abused as inhalants. Other inhalants include the nitrites (amyl and butyl, “poppers”, “Rush”) and gases such as the anesthetics nitrous oxide (laughing gas) and ether. Inhalants can be breathed in through the nose or mouth in a variety of ways, including spraying aerosols directly into the nose or mouth, “sniffing” or "snorting” fumes from containers, inhaling from balloons filled with nitrous oxide, “huffing” from an inhalant-soaked rag stuffed in the mouth, or “bagging”- pouring the substance over a cloth or into a plastic bag and breathing in the vapours.