Annual Report and Accounts 2014/15
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Suffolk's Framework for Growth
Suffolk’s Framework for Growth 1 Foreword Suffolk’s local authorities are working together to address our residents and businesses’ future needs and deliver our growth plans in an inclusive and integrated way. Responding to the Government’s ambitions to increase the nation’s overall prosperity and recognising past growth has not always benefitted all communities equally, our Framework sets out how we will utilise Suffolk’s potential to ensure we plan and achieve the growth that is right for us and our communities. A Framework provides a mechanism to bring together work across teams; including local planning, economic development, skills, and housing; alongside our partners at the University of Suffolk, Suffolk Chamber of Commerce and New Anglia LEP. It sets out how we are working across our administrative boundaries and with our key partners to deliver our physical development (homes, employment sites, public and private buildings) in a way that matches our communities’ aspirations for growth and ensures we can match this with the investment in our infrastructure both now and in the future. The Framework includes links where you can find further, more detailed information. It builds on our conversations with Government, our partners and our communities, which started with our proposals for devolution and have been built on through our responses to both the Industrial Strategy and the Housing White Paper. It will provide the mechanism for monitoring our successes and realigning work that is not achieving the outcomes we anticipate. This Framework has been agreed by all Suffolk Local Authority Leaders and the joint Suffolk Growth Portfolio Holders (GP/H). -

Suffolk County Council
Suffolk County Council Western Suffolk Employment Land Review Final Report May 2009 GVA Grimley Ltd 10 Stratton Street London W1J 8JR 0870 900 8990 www.gvagrimley.co.uk This report is designed to be printed double sided. Suffolk County Council Western Suffolk Employment Land Review Final Report May 2009 Reference: P:\PLANNING\621\Instruction\Clients\Suffolk County Council\Western Suffolk ELR\10.0 Reports\Final Report\Final\WesternSuffolkELRFinalReport090506.doc Contact: Michael Dall Tel: 020 7911 2127 Email: [email protected] www.gvagrimley.co.uk Suffolk County Council Western Suffolk Employment Land Review CONTENTS 1. INTRODUCTION........................................................................................................... 1 2. POLICY CONTEXT....................................................................................................... 5 3. COMMERCIAL PROPERTY MARKET ANALYSIS.................................................... 24 4. EMPLOYMENT LAND SUPPLY ANALYSIS.............................................................. 78 5. EMPLOYMENT FLOORSPACE PROJECTIONS..................................................... 107 6. BALANCING DEMAND AND SUPPLY .................................................................... 147 7. CONCLUSIONS AND RECOMMENDATIONS......................................................... 151 Suffolk County Council Western Suffolk Employment Land Review LIST OF FIGURES Figure 1 The Western Suffolk Study Area 5 Figure 2 Claydon Business Park, Claydon 26 Figure 3 Industrial Use in -

September 2015
Chatsworth The Secret Garden The Felixstowe Society Newsletter Issue Number 110 September 1 2015 In this issue: Our trip to Chatsworth, Hardwick and Lincoln The Secret Garden of Westmorland Road Society News, Reviews and Research Registered Charity No. 277442 Founded 1978 The Felixstowe Society is established for the public benefit of people who either live or work in Felixstowe and Walton. Members are also very welcome from the Trimleys and the surrounding villages. The Society endeavours to: stimulate public interest in these areas promote high standards of planning and architecture and secure the improvement, protection, development and preservation of the local environment. Contents 3 Notes from the Chairman – Roger Baker 4 Calendar – September to December 2015 5 Can You Help Us? 6 Society News 8 Speaker Evening Report - An Audience with Peter Phillips 9 The Society Dinner 10 Speaker Evening Report - The Home Front in Suffolk 1914-18 11 An Evening at The Hut 12 Beach Clean 13 Society Members’ Feature 14 Felixstowe Youth Society 16 Our Three Day Trip to Derbyshire, South Yorkshire and Lincolnshire 18 Visit to Norwich and Kirstead Hall 19 Felixstowe Walkers 20 The Abbey Grove Challenge 22 Book Reviews 23 The Felixstowe Beach Hut and Chalet Association 24 News from The Felixstowe Museum 25 Research Corner 24 - Felixstowe’s Prefabs 28 Planning Applications March 21 to July 7 2015 30 If you wish to join The Society 32 More pictures from The Secret Garden Notes from the Chairman Welcome back after the summer break. I hope that you are looking forward to the new season of talks and activities – see the list of Speaker Meetings in this issue of the Newsletter. -
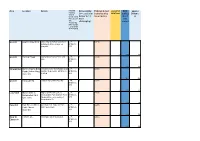
(3 = Easiest to Deliver to 1 = Most Challenging) Estimated Cost
Area Location Details Potential Deliverability Estimated Cost unweighted BCR approx Funding (3 = easiest to (calculated by MCAF total (ebike) Distance Source (Local Travel deliver to 1 = linear metre) nb 0 = m Plan, Section most not 106, challenging) scored Community Infrastructur e Levy, Dept. of Transport) Ipswich Ipswich Waterfront University of Suffolk waterfont LTP, 3 £473k building to Stoke bridge on S106/CIL, quayside DfT 5 44.1 789 Ipswich Portman Road Barrack Corner to Princes St LTP, 3 £214k junc S106/CIL, DfT 3 32.6 360 Stowmarket Chilton Way to Bury This link Lowry Way/Rugby Club LTP, 2 £495k Road (Chilton Way) junction to Bury Rd - BCR to be S106/CIL, Cycle link verified DfT 3 27.4 825 Ipswich Yarmouth Rd London Rd to Bramford Rd - LTP, 3 £327k S106/CIL, DfT 2 22.9 545 Lowestoft Higher Drive to Higher Dr/Woods Loke to LTP, 3 £432k Normanston Park Normanston Park (not incl Park S106/CIL, cycle route tracks) will need crossing of DfT Normanston Dr. 2 22.5 720 Haverhill Park Rd - A1307 to potential new route (or Park LTP, 3 £420k Castle Manor Rd?) spine route S106/CIL, Academy DfT 6 21.8 750 Bury St Cotton Lane Northgate St to Mustow St LTP, 1 £205k Edmunds S106/CIL, DfT 4 15.2 685 Ipswich Princes St link to rail station LTP, 2 £461k S106/CIL, DfT 3 14.9 770 Ipswich Belstead Rd Luther Rd to Stoke Bridge LTP, 2 £969k S106/CIL, DfT 3 13.4 1615 Ipswich Grove Ln to Civic Dr Rope Walk, Tackett St, Dogs LTP, 2 £1163k Head St S106/CIL, DfT 3 13.1 1940 Haverhill Manor Rd Ruffles Rd/Millfields Way junc, LTP, 3 £174k Manor Rd,Eringhausen -

2 Bedroom Apartments with 3 Bedroom Homes, Located in The
Akenham Spencer’s Court Tuddenham Whitton Bramford Road A14 Suffolk, IP1 5BQ Bramford Rushmere Saint Andrew Spencers Court A1214 A1156 How to find Spencer Court Valley Road Kesgrave A1214 Spencer’s Court Hadleigh Road A1214 Industrial Estate Ipswich A1071 From the A14 take junction 53 signposted A1156. Penzance Bramford Road At the roundabout take the exit signposted Ipswich A14 A1189 West and North (A1156). You will see Anglia Park A1071 London Road Suffolk, IP1 5BQ on the left and ASDA on the right. At the next A137 A1156 Felixstowe Roa roundabout take the second exit signposted Foxhall Hall ad d o town centre. You are now entering Ipswich. At the Chantry R traffic lights continue straight over into Norwich stead Wher Road (Shell petrol station on the right hand side) A137 Pinewood past the BP petrol station; continue to follow the Warren Heath A14 A12 A1189 Norwich Road through several sets of traffic lights. Copdock Just before the bridge turn right into Cromer Road. At the end of Cromer Road go straight over the crossroads into Eustace Road. Turn left into Bramford Ln A14 Brockleyr Cr Pitcairn Road and follow to the end. Turn right A1156 into Bramford Road and continue forward passing Cromer Rd Dandalan Close on the left and a new homes Hennisker Rd development on the left and right. You will see Spencers Court Bramford Rd Wallace Rd Spencers Court directly opposite the Post Office on Europe Way the fringe of Adair Road. Bramford Ln Bramford Rd Farthing Rd Sproughton Rd Sproughton Rd Hadleigh Rd Industrial Estate A1214 Yarmouth RdYarmouth High St Church Ln A14 London Rd Hadleigh Rd 2 bedroom apartments with Church Ln Hadleigh Rd Chantry Park London Rd 3 bedroom homes, located in the stunning area of Suffolk. -
SUFFOLK LOCAL PLAN MODELLING Forecasting Report - Forecasts with Demand Adjustments
Suffolk County Council SUFFOLK LOCAL PLAN MODELLING Forecasting Report - Forecasts with demand adjustments SCC LP 9.2 OCTOBER 2020 PUBLIC Suffolk County Council SUFFOLK LOCAL PLAN MODELLING Forecasting Report - Forecasts with demand adjustments TYPE OF DOCUMENT (VERSION) PUBLIC PROJECT NO. 70044944 OUR REF. NO. SCC LP 9.2 DATE: OCTOBER 2020 WSP WSP House 70 Chancery Lane London WC2A 1AF Phone: +44 20 7314 5000 Fax: +44 20 7314 5111 WSP.com PUBLIC QUALITY CONTROL Issue/revision First issue Revision 1 Revision 2 Revision 3 Remarks Draft Draft Final Date July 2020 September 2020 October 2020 Prepared by Louise Murray- Leonardo Mendes Leonardo Mendes Bruce Signature Checked by Leonardo Mendes Charlotte Herridge Charlotte Herridge Signature Authorised by Michael Johns Michael Johns Michael Johns Signature Project number 70044944 70044944 70044944 Report number SCC_LP 9.0 SCC_LP 9.1 SCC_LP 9.2 File reference SUFFOLK LOCAL PLAN MODELLING PUBLIC | WSP Project No.: 70044944 | Our Ref No.: SCC LP 9.2 October 2020 Suffolk County Council CONTENTS EXECUTIVE SUMMARY 1 GLOSSARY 1 2 INTRODUCTION 4 2.1 BACKGROUND 4 2.2 TRANSPORT MODEL 4 2.3 STUDY AREA 6 2.4 FUTURE HIGHWAY SCHEMES 11 2.5 FORECAST DEVELOPMENT ASSUMPTIONS 14 3 RESULTS 16 3.1 SUFFOLK HIGHWAY FOCUS 16 3.2 VOLUME TO CAPACITY RATIO 16 3.3 MODEL RUNS COMPARED 16 3.4 PASSENGER CAR UNIT HOUR DELAY REDUCTION BY LPA – DEMAND ADJUSTMENT IMPACT 17 3.5 OVERALL JUNCTION V/C SUMMARY BY LPA – DEMAND ADJUSTMENT IMPACT 22 3.6 OVERALL LINK V/C SUMMARY BY LPA – DEMAND ADJUSTMENT IMPACT 25 3.7 RESULTS SUMMARIES -

Ipswich Borough Council Local Plan
Ipswich Borough Council Local Plan Statement of Compliance with the Duty to Co-operate January 2020 Planning and Development Ipswich Borough Council Grafton House, Russell Road Ipswich IP1 2DE (01473) 432019 email: [email protected] website: www.ipswich.gov.uk Contents 1. Introduction 2. Context 3. Neighbouring local planning authorities 4. Key management / operational arrangements 5. Suffolk Devolution proposals 6. Addressing strategic issues 7. Undertaking joint studies 8. Summary of co-operation in the preparation of the Ipswich Local Plan Table 1 – Summary of Duty to Co-operate process Table 2 – Site Allocations Appendix 1 – Plan showing the Ipswich Policy Area Appendix 2 – Draft Memorandum of Understanding relating to the delivery of housing and employment development within the Ipswich Housing Market Area and Ipswich Functional Economic Area Appendix 3 – Ipswich Policy Area Board Terms of Reference 1. Introduction The Duty to Co-operate (the duty) was introduced through Section 110 of the Localism Act 2011. The Act inserts a new Section 33A into the Planning and Compulsory Purchase Act 2004. The duty is a legal duty on local planning authorities to co-operate constructively, actively and on an ongoing basis with neighbouring authorities, county councils and other prescribed bodies in planning for strategic cross boundary matters. The National Planning Policy Framework 2019 states that in order to demonstrate effective and on-going joint working, strategic policy making authorities should prepare and maintain one or more statements of common ground, documenting the cross-boundary matters being addressed and progress in cooperating to address these. Cooperation is ongoing and statements will be updated as necessary. -

Bramford GSP (East) – Diss and Stowmarket
Regional Development Plan RDP10 Bramford GSP (East) – Diss and Stowmarket (EPN) Planner D J Whiteley Version 2.0 UK Power Networks (Operations) Limited. Page 1 of 28 Date 20/03/2014 Registered in England and Wales. Regional Development Plan Bramford East – Diss & Stowmarket All of the cost numbers displayed in this document are before the application of on-going efficiencies and real price effects. Contents 1 EXECUTIVE SUMMARY .................................................................................................................................. 3 1.1 SUMMARY OF ISSUES ADDRESSED ........................................................................................................................ 3 1.2 RECOMMENDED STRATEGY ................................................................................................................................. 4 2 NETWORK CONFIGURATION .......................................................................................................................... 7 2.1 EXISTING NETWORK .......................................................................................................................................... 7 2.2 NETWORK CHANGES IN PROGRESS ........................................................................................................................ 7 3 SUMMARY OF ISSUES .................................................................................................................................. 8 3.1 DEVELOPMENT AREAS ...................................................................................................................................... -

3592 the London Gazette, 20Th May 1960
3592 THE LONDON GAZETTE, 20TH MAY 1960 EAST SUFFOLK COUNTY COUNCIL Extensions of Speed Limits in East Suffolk Notice is hereby given that the East Suffolk County Council intend to make application to the Minister of Transport for his consent to the making of an Order, the effect of which will be that the sections of road referred to in the Schedule hereto .shall be deemed to be roads in a built-up area for the purposes of the Road Traffic Act, 1934, Section 1. The purpose of the Order is to extend existing restricted sections of road and to impose restrictions on additional .•sections in consequence of alterations in street lighting and traffic conditions. Any objection to the making of such Order should be sent to the under-signed not later than 17th June 1960. G. C. Lightfoot, Clerk of the County Council. County Hall, Ipswich. .16th May 1960. SCHEDULE Situation Description of Length of Road Length Lin. Yds. Borough • of Aldeburgh That section of the Aldeburgh-Thorpeness Road which lies between Tiffany's Corner and a point 343 lin. yds. to the north 343 Barham That section of the Claydon-Norwich Road (A. 140) which lies between a point approx. 270 lin. yds. south of Barham Church Lane and a point 100 lin. yds. south from the same junction 170 Uotesdale . That section of the Bury St. Edmunds-Harleston Road (A.143) which lies between a point 129 lin. yds, east of its junction with Garden House Lane and a point approx. 562 lin. yds. north-east of the same junction .. -

Ipswich Strategic Planning Area Local Plan Modelling
Suffolk County Council SUFFOLK LOCAL PLAN MODELLING Methodology Report ISPA-MR9.3 OCTOBER 2020 PUBLIC Suffolk County Council SUFFOLK LOCAL PLAN MODELLING Methodology Report TYPE OF DOCUMENT (VERSION) PUBLIC PROJECT NO. 70044944 OUR REF. NO. ISPA-MR9.3 DATE: OCTOBER 2020 WSP WSP House 70 Chancery Lane London WC2A 1AF Phone: +44 20 7314 5000 Fax: +44 20 7314 5111 WSP.com PUBLIC QUALITY CONTROL Issue/revision First issue Revision 1 Revision 2 Revision 3 Remarks Draft Draft Draft Final Date July 2020 July 2020 September 2020 October 2020 Prepared by Michael Johns Michael Johns Michael Johns Michael Johns Signature Checked by Michael Johns Charlotte Herridge Charlotte Herridge Charlotte Herridge Signature Authorised by Michael Johns Michael Johns Michael Johns Michael Johns Signature Project number 70044944 70044944 70044944 70044944 Report number ISPA-MR9 ISPA-MR9.1 ISPA-MR9.2 ISPA-MR9.3 File reference SUFFOLK LOCAL PLAN MODELLING PUBLIC | WSP Project No.: 70044944 | Our Ref No.: ISPA-MR9.3 October 2020 Suffolk County Council CONTENTS 1 GLOSSARY 1 2 INTRODUCTION 3 2.1 BACKGROUND 3 2.2 REPORT STRUCTURE 5 3 FUTURE HIGHWAY SCHEMES 6 4 LOCAL PLAN GROWTH 9 4.1 STRATEGIC PLANNING AREAS 9 4.2 HOUSING AND JOB GROWTH INPUTS 10 4.3 TRIP GENERATION APPROACH 12 4.4 LGV / HGV GROWTH 12 5 DEMAND ADJUSTMENTS AND FORECAST METHODOLOGY 14 5.1 OVERVIEW 14 5.2 EXISTING ROAD USERS / TRAVEL PATTERNS 15 5.3 NEW ROAD USERS 15 5.4 RESIDUAL LOCAL PLAN GROWTH 17 6 COMPARISON OF MATRIX TOTALS 19 6.1 SECTORING SYSTEM 19 6.2 REDUCTION IN EXISTING ROAD USERS / TRAVEL PATTERNS -

Ipswich Summer League Matches 2015 LADIES 1
Woodbridge Tennis Club - Ipswich Summer League Matches 2015 LADIES 1 - CAPTAIN : Dee Oakley / Alison Hallwright Mon 11th May Div 1 Woodbridge V Felixstowe Home Mon 18th May Div 1 Woodbridge V YM Tennis Home Mon 1st June Div 1 St Johns 1 V Woodbridge Away 6.30pm Mon 8th June Div 1 Felixstowe V Woodbridge Away 6.30pm Mon 22nd June Div 1 YM Tennis V Woodbridge Away 6.45pm Mon 29th June Div 1 Ipswich V Woodbridge Away 7pm Mon 6th July Div 1 Woodbridge V St Johns Home Mon 20th July Div 1 Woodbridge V Ipswich Home LADIES 2 - CAPTAIN : Di Start Fri 1st May Div 4 David Lloyd 2 V Woodbridge Away 7pm Mon 18th May Div 4 Kesgrave V Woodbridge Away 7pm Mon 1st June Div 4 Woodbridge V Creekers Home Mon 15th June Div 4 Woodbridge V Woolpit Home Thu 18th June Div 4 Creekers V Woodbridge Away 7pm Wed 1st July Div 4 Woolpit V Woodbridge Away 7pm Mon 6th July Div 4 Woodbridge V Kesgrave Home Mon 13th July Div 4 Woodbridge V David Lloyd 2 Home Contacts Felixstowe 1 Lysette Fulcher 07963 118428 St Johns 1 Sue Palmer 01473 742389 YM Tennis Laura Mee 07917 874516 / 01473 403859# Ipswich 1 Tip Flory 07720 890656 / 01473 738055 David Lloyd 2 Sue Thomas 07880 593218 Creekers Karen Wolf-Evans 07768 764632 Woolpit TBC Kesgrave Rosie Ven or 07771 968415 / 01473 611808 Coleen Howard 07751 888651 / 01473 717273 Woodbridge Tennis Club - Ipswich Summer League Matches 2015 MENS 1 - CAPTAIN : Jon Mansfield 07796 366032 Wed 6th May Div 4 Woodbridge V Creekers Home Wed 13th May Div 4 David Lloyd 3 V Woodbridge Away 7pm Wed 3rd June Div 4 Woodbridge V YM Tennis Home Wed 24th -

Memorials of Old Suffolk
I \AEMORIALS OF OLD SUFFOLK ISI yiu^ ^ /'^r^ /^ , Digitized by the Internet Archive in 2009 with funding from University of Toronto http://www.archive.org/details/memorialsofoldsuOOreds MEMORIALS OF OLD SUFFOLK EDITED BY VINCENT B. REDSTONE. F.R.HiST.S. (Alexander Medallitt o( the Royal Hul. inK^ 1901.) At'THOB or " Sacia/ L(/* I'm Englmnd during th* Wmrt »f tk* R»ut,- " Th* Gildt »nd CkMHtrUs 0/ Suffolk,' " CiUendar 0/ Bury Wills, iJS5-'535." " Suffolk Shi^Monty, 1639-^," ttc. With many Illustrations ^ i^0-^S is. LONDON BEMROSE & SONS LIMITED, 4 SNOW HILL, E.G. AND DERBY 1908 {All Kifkts Rtterifed] DEDICATED TO THE RIGHT HONOURABLE Sir William Brampton Gurdon K.C.M.G., M.P., L.L. PREFACE SUFFOLK has not yet found an historian. Gage published the only complete history of a Sufifolk Hundred; Suckling's useful volumes lack completeness. There are several manuscript collections towards a History of Suffolk—the labours of Davy, Jermyn, and others. Local historians find these compilations extremely useful ; and, therefore, owing to the mass of material which they contain, all other sources of information are neglected. The Records of Suffolk, by Dr. W. A. Copinger shews what remains to be done. The papers of this volume of the Memorial Series have been selected with the special purpose of bringing to public notice the many deeply interesting memorials of the past which exist throughout the county; and, further, they are published with the view of placing before the notice of local writers the results of original research. For over six hundred years Suffolk stood second only to Middlesex in importance ; it was populous, it abounded in industries and manufactures, and was the home of great statesmen.