Harnessing the Power of Polygenic Risk Scores to Predict Type 2 Diabetes and Its Subtypes in a High-Risk Population of British P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Karoline R.) Son, Morgan
North Carolina Bapst Secretaries Associaon ʹͲʹͲ ͵ǡ ͳ A quarterly publicaon connecng Bapst Secretaries across North Carolina A NOTE FROM THE PRESIDENT Well, here we are in January of 2020, and from everything I have heard and read, the 2019 NCBSA conference at Fort Caswell was another good one! Of course, you will recall that I was absent, regreully. And as thrilled as I was to be able to spend three weeks in California helping my son and his family as they welcomed a new baby, I cannot express just how disappointed I was to miss the conference. Especially aer having spent the year planning and praying and seeing everything come together in the way we believe had God’s fingerprints on it. Becke Joseph is now 3-months old (wearing 9-month-old clothes!) and is a happy, talkave baby. His sister has finally accepted him into her family and they are all doing well. They asked in a recent phone call if I could come for another visit to help as my daughter-in-law transions back into work, right about the me my son is being sent to Bahrain. So, it looks as though I may be making another trip to the West Coast someme in April and I am looking forward to seeing those grandchildren again. I am especially thankful for the ability to do so and even more thankful for frequent flyer miles! This arcle won’t be highlighng the conference, as I can’t really do that. But I appreciate Angela Cockerham, your president-elect, for taking care of that. -

Message from Board President
MESSAGE FROM HEAD OF SCHOOL Head of School MESSAGE FROM BOARD PRESIDENT “Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it's the only thing that ever has.” -Margaret Mead We are forever grateful. Leah Ann Kleinfeldt President, Board of Directors Audrey & William Farber Family William Davidson Foundation The Norman & Esther Allan Foundation Brenda & Samuel Gewurz Julie & Eugene Sherizen Lisa & Gary Shiffman Elana & Max Berlin Penny & Harold, Carol & Richard Blumenstein Nancy & James Grosfeld Rachel & Joshua Opperer The D. Dan & Betty Kahn Foundation Karp Family Foundation Sarah & Dr. Martin Kornblum Nicole & Matthew Lester Dr. Ora & Dr. Michael Singer Lori & Alan Zekelman Rebecca & Gil Feldman Michal & Dr. Howard Korman Rita & Dr. Bert Schreiber Malke & Gary Torgow Sherri & Andrew Weil Bryan Schon Anonymous Anonymous Kimberly Schon Anonymous Rosa & George Chessler Judy & Dr. Fred Zwas April & Kevin Adelson Debbie & Dr. Jeffrey Devries Anonymous Deborah Movsky- Laurie & Dr. Phillip Goldmeier Anonymous Apap & Dr. Yoni Apap Joanne & Dr. Daniel Gotlib Dr. Karoline Puder & Paul Fischer Hadas & Dennis Bernard Rebecca & Dr. Mitchell Klausner Jill & Dr. Joseph Greenbaum Sharon & Larry Berry Dr. Susan & Ed Kresch Leah Ann Kleinfeldt & Penny & Seymour Greenstein Anita & Robert Naftaly Dr. Gerald Kirzner Dr. Shoshana & Sidney Katz Susie & Norman Pappas Sheryl & Dr. Seth Korelitz Linda & Dr. Harvey Lefkowitz Amira & Joseph Skoczylas Anat & Dr. Gabriel Levi Lisa & Dr. Alan Millman Ariella & Michael Skoczylas Cherie & Dr. Noah Levi Donna Zwas Barbara & Dr. Milton Stern Lisa & Dan Mendelson Amy Zwas & Yoram Bitton Marla & Jerald Zwas Susie & Irving Bernhardt |Marci & Dr. David Beneson | Marion & Harvey Bronstein Dave Dombey | Cookie & Dr. Bernard Gonik | Gillian & Daniel Greenbaum Carrie & Dr. -

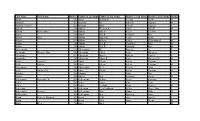
2019 Salary Listing
Last Name First Name Total Earnings for Year ABIDI MOHAMED $12,467.93 ABIDI PEGGY $53,864.36 AHLERS JEFFREY $60,549.34 AKRAMI RAHIMULLAH $21,113.05 ALFORD ADRIENE $782.76 ALLEN ANTHONY $5,307.67 ALLEYNE DEBRA $5,670.71 ALSALEM MAHDI $8,859.50 AMBERG AMY $57,570.58 AMBROSY MARIA $7,147.16 AMBROSY SAMUEL $2,718.89 ANDREGG CARLY $4,620.11 ANDRESEN HOLLY $16,169.20 ANDRESS JENNIFER $13,636.47 ANSEL JACQUELINE $1,142.64 ANSTOETTER BRYCE $221.40 ANSTOETTER GABRIEL $169.46 ARENSDORF PHILIP $87,097.30 ARENSDORF DENNY $53,522.42 ARENSDORF PHYLLIS $47,292.80 ARMOUR EVAN $82,800.01 ATKINSON JERROD $87,484.25 ATKINSON TODD $47,803.89 ATWOOD SYDNEY $2,310.00 AVALOS KRISTYN $20,518.70 AVENARIUS KATHERINE $1,688.18 AVENARIUS PAUL $82,253.20 BAKER KATHRYN $60,844.90 BAKEY DAVID $63,988.39 BANDY NICHOLAS $2,508.68 BANKSON RYAN $25,424.12 BANNON DANIEL $68,713.54 BARRY ROBERT $79,821.34 BARTLETT PAUL $40,616.43 BARTLEY EMILY $6,667.10 BARTON LISA $56,969.09 BASSLER TERESA $78,829.83 BASTEN MICHAEL $1,490.84 BAUER BRANDON $82,714.63 BAUER SCOTT $62,689.45 BAUMGARTNER MARTIN $4,853.42 BAUMHOVER BRANDI $45,446.96 BAXTER SCOTT $110,950.90 BEATTY ERIN $2,862.14 BEAU JANNA $74,743.97 BEAVES DAVID $74,422.33 BECK DANIELLE $77,598.91 BECKER CHRIS $4,757.59 BECKER ROBERT $24,302.07 BEHNKE RAYMOND $65,202.38 BELL GINA $67,590.81 BELLIS JEFFREY $5,226.52 BEN JEROME $76,193.20 BENDA MARTIN $54,897.83 BENDER BRITNIE $116.35 BENEVENTI MACKENZIE $31,544.61 BENNETT MEGGAN $31,473.53 BENTLEY JOHNATHAN $14,657.20 BENZ ROGER $33,913.11 BERENDES CHAD $55,080.19 BERGFELD AMANDA -
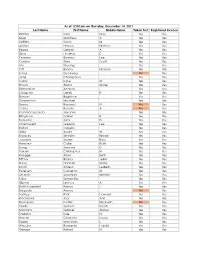
Last Name First Name Middle Name Taken Test Registered License
As of 12:00 am on Thursday, December 14, 2017 Last Name First Name Middle Name Taken Test Registered License Richter Sara May Yes Yes Silver Matthew A Yes Yes Griffiths Stacy M Yes Yes Archer Haylee Nichole Yes Yes Begay Delores A Yes Yes Gray Heather E Yes Yes Pearson Brianna Lee Yes Yes Conlon Tyler Scott Yes Yes Ma Shuang Yes Yes Ott Briana Nichole Yes Yes Liang Guopeng No Yes Jung Chang Gyo Yes Yes Carns Katie M Yes Yes Brooks Alana Marie Yes Yes Richardson Andrew Yes Yes Livingston Derek B Yes Yes Benson Brightstar Yes Yes Gowanlock Michael Yes Yes Denny Racheal N No Yes Crane Beverly A No Yes Paramo Saucedo Jovanny Yes Yes Bringham Darren R Yes Yes Torresdal Jack D Yes Yes Chenoweth Gregory Lee Yes Yes Bolton Isabella Yes Yes Miller Austin W Yes Yes Enriquez Jennifer Benise Yes Yes Jeplawy Joann Rose Yes Yes Harward Callie Ruth Yes Yes Saing Jasmine D Yes Yes Valasin Christopher N Yes Yes Roegge Alissa Beth Yes Yes Tiffany Briana Jekel Yes Yes Davis Hannah Marie Yes Yes Smith Amelia LesBeth Yes Yes Petersen Cameron M Yes Yes Chaplin Jeremiah Whittier Yes Yes Sabo Samantha Yes Yes Gipson Lindsey A Yes Yes Bath-Rosenfeld Robyn J Yes Yes Delgado Alonso No Yes Lackey Rick Howard Yes Yes Brockbank Taci Ann Yes Yes Thompson Kaitlyn Elizabeth No Yes Clarke Joshua Isaiah Yes Yes Montano Gabriel Alonzo Yes Yes England Kyle N Yes Yes Wiman Charlotte Louise Yes Yes Segay Marcinda L Yes Yes Wheeler Benjamin Harold Yes Yes George Robert N Yes Yes Wong Ann Jade Yes Yes Soder Adrienne B Yes Yes Bailey Lydia Noel Yes Yes Linner Tyler Dane Yes Yes -

Baby Girl Names | Registered in 2019
Vital Statistics Baby2019 BabyGirl GirlsNames Names | Registered in 2019 From:Jan 01, 2019 To: Dec 31, 2019 First Name Frequency First Name Frequency First Name Frequency Aadhini 1 Aarnavi 1 Aadhirai 1 Aaro 1 Aadhya 2 Aarohi 2 Aadila 1 Aarora 1 Aadison 1 Aarushi 1 Aadroop 1 Aarya 3 Aadya 3 Aarza 2 Aafiya 1 Aashvee 1 Aaghnya 1 Aasiya 1 Aahana 2 Aasiyah 2 Aaila 1 Aasmi 1 Aaira 3 Aasmine 1 Aaleena 1 Aatmja 1 Aalia 1 Aatri 1 Aaliah 1 Aayah 2 Aalis 1 Aayara 1 Aaliya 1 Aayat 1 Aaliyah 17 Aayla 1 Aaliyah-Lynn 1 Aayna 1 Aalya 1 Aayra 2 Aamina 1 Aazeen 1 Aamna 1 Abagail 1 Aanaya 1 Abbey 4 Aaniya 1 Abbi 1 Aaniyah 1 Abbie 1 Aanya 3 Abbiejean 1 Aara 1 Abbigail 3 Aaradhya 1 Abbiteal 1 Aaradya 1 Abby 10 Aaraya 1 Abbygail 1 Aaria 2 Abdirashid 1 Aariya 1 Abeeha 1 Aariyah 1 Aberlene 1 Aarna 3 Abhideep 1 Abi 1 Abiah 1 10 Jun 2020 1 Abiegail 02:22:21 PM1 Abigael 1 Abigail 141 Abigale 1 1 10 Jun 2020 2 02:22:21 PM Baby Girl Names | Registered in 2019 First Name Frequency First Name Frequency Abigayle 1 Addalyn 4 Abihail 1 Addalynn 1 Abilene 2 Addasyn 1 Abina 1 Addelyn 1 Abisha 2 Addi 1 Ablakat 1 Addie 2 Aboni 1 Addilyn 3 Abrahana 1 Addilynn 2 Abreen 1 Addison 61 Abrielle 2 Addisyn 2 Absalat 1 Addley 1 Abuk 2 Addy 1 Abyan 1 Addyson 2 Abygale 1 Adedoyin 1 Acadia 1 Adeeva 1 Acelynn 1 Adeifeoluwa 1 Achai 1 Adela 1 Achan 1 Adélaïde 1 Achol 1 Adelaide 20 Ackley 1 Adelaine 1 Ada 23 Adelayne 1 Adabpreet 1 Adele 4 Adaeze 1 Adèle 2 Adah 1 Adeleigha 1 Adair 1 Adeleine 1 Adalee 1 Adelheid 1 Adalena 1 Adelia 3 Adaley 1 Adelina 2 Adalina 2 Adeline 40 Adalind 1 Adella -

MSU Commencement Ceremonies Fall 2020
COMMENCEMENT CEREMONIES FALL 2020 “Go forth with Spartan pride and confdence, and never lose the love for learning and the drive to make a diference that brought you to MSU.” Samuel L. Stanley Jr., M.D. President Michigan State University Photo above: an MSU entrance marker of brick and limestone, displaying our proud history as the nation’s pioneer land-grant university. On this—and other markers—is a band of alternating samara and acorns derived from maple and oak trees commonly found on campus. This pattern is repeated on the University Mace (see page 10). Inside Cover: Pattern of alternating samara and acorns. Michigan State University photos provided by University Communications. ENVIRONMENTAL TABLE OF CONTENTS STEWARDSHIP Mock Diplomas and the COMMENCEMENT Commencement Program Booklet 3 Virtual Commencement Ceremonies Commencement mock diplomas, 4 The Michigan State University Board of Trustees which are presented to degree 5 Michigan State University Mission Statement candidates at their commencement 6–8 Congratulatory Letters from the President, Provost, and Executive Vice President ceremonies, are 30% post-consumer 9 Michigan State University recycled content. The Commencement 10 Ceremony Lyrics program booklet is 100% post- 11 University Mace consumer recycled content. 12 Academic Attire 13 Keynote Speakers Caps and Gowns 14–16 Keynote Speaker Profles Graduating seniors’ caps and gowns and master’s degrees’ caps and BACCALAUREATE DEGREES gowns are made of post-consumer 18 Honors recycled content; each cap and 19 Order of Ceremonies gown is made of a minimum of 20–21 College of Agriculture and Natural Resources 23 plastic bottles. 22 Residential College in the Arts and Humanities 23–24 College of Arts and Letters Recycle Your Cap and Gown 25–26 The Eli Broad College of Business Once all of your favorite photos are 27–29 College of Communication Arts and Sciences taken on campus, please recycle 30 College of Education your gown at the MSU Union 31–32 College of Engineering Spartan Spirit Shop. -
Last Name First Name Birth Yrfather's Last Name Father's
Last Name First Name Birth YrFather's Last Name Father's First Name Mother's Last Name Mother's First Name Gender Aaron 1907 Aaron Benjaman Shields Minnie M Aaslund 1893 Aaslund Ole Johnson Augusta M Aaslund (Twins) 1895 Aaslund Oluf Carlson Augusta F Abbeal 1906 Abbeal William A Conlee Nina E M Abbitz Bertha Dora 1896 Abbitz Albert Keller Caroline F Abbot 1905 Abbot Earl R Seldorff Rose F Abbott Zella 1891 Abbott James H Perry Lissie F Abbott 1896 Abbott Marion Forder Charolotta M M Abbott 1904 Abbott Earl R Van Horn Rose M Abbott 1906 Abbott Earl R Silsdorff Rose M Abercrombie 1899 Abercrombie W Rogers A F Abernathy Marjorie May 1907 Abernathy Elmer Scott Margaret F Abernathy 1892 Abernathy Wm A Roberts Laura J F Abernethy 1905 Abernethy Elmer R Scott Margaret M M Abikz Louisa E 1902 Abikz Albert Keller Caroline F Abilz Charles 1903 Abilz Albert Keller Caroline M Abircombie 1901 Abircombie W A Racher Allos F Abitz Arthur Carl 1899 Abitz Albert Keller Caroline M Abrams 1902 Abrams L E Baker May F Absher 1905 Absher Ben Spillman Zoida M Achermann Bernadine W 1904 Ackermann Arthur Krone Karolina F Acker 1903 Acker Louis Carr Lena F Acker 1907 Acker Leyland Ryan Beatrice M Ackerman 1904 Ackerman Cecil Addison Willis Bessie May F Ackermann Berwyn 1905 Ackermann Max Mann Dolly M Acklengton 1892 Achlengton A A Riacting Nattie F Acton Rebecca Elizabeth 1891 Acton T M Cox Josie E F Acton 1900 Acton Chas Payne Minnie M Adair Elles 1906 Adair Adel M Last Name First Name Birth YrFather's Last Name Father's First Name Mother's Last Name Mother's -
Bow Knot 4-H Newsletter
Bow Knot 4-H Newsletter 431 So. 10th Avenue | Broken Bow, NE 68822 | (308) 872-6831 | www.custer.unl.edu UPCOMING EVENTS NOVEMBER 11 Office closed for holiday 13 2018 CWF Curriculum Meeting, 4-H Building, 2:00 p.m. 15 2018 CWF Payment Due November 2016 18 4-H Recognition Night, City Auditorium, BBQ-5:30-7:00 p.m., Program-7:00 p.m. 21 NRA Grant Applications Due 21 4-H Council Meeting, 4-H Building, 7:30 p.m. 24-25 Office closed for holiday DECEMBER 25-26 Office closed for holiday JANUARY 2 Office closed for holiday 15 2018 CWF Trip Curriculum Meeting, 4-H Building, 2:00 p.m. 15 2018 CWF Payment Due 16 Office Closed for Martin Luther King Holiday 16 4-H Council Meeting, 4-H Building, 6:30 p.m. 4-H VOLUNTEER INFORMATION SERIES 4-H CLUB OFFICERS AND DUTIES YOU’RE INVITED TO… Record books are completed, premium money is being awarded, and 4-H Recognition Night is upon us. In the 4-H Recognition Night next few months, 4-H clubs will be Friday, November 18, 2016 reorganizing and electing officers for the 2017 Broken Bow City Auditorium year. Enclosed is a handout listing the responsibilities of 4-H club officers. 5:30 - 7:00 p.m. 4-H Family Barbecue Great Food and Door Prizes 4-H officer guides, treasurer’s record, secretary’s record, and a news reporter guide 7:00 p.m. are all available at the Extension Office. 4-H Council Election 4-H Member and Leader Recognition 2016 CWF Presentation RSVP to the Extension Office by Monday, November 14 The event is co-sponsored by: Arrow Seed Co., Inc. -
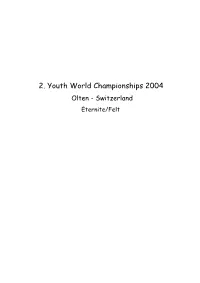
2004 JWM Olten, CH
2. Youth World Championships 2004 Olten - Switzerland Eternite/Felt 2. Youth World Championships 2004 Olten - Switzerland Rank Score - Rounds - Average Overall/Eternite/Felt Player Nation Score Eternit / Felt Youth Men 1 17 1 Linus Sundström Sweden 289 131 6 21,83 158 6 26,33 2 3 2 Peter Eisenschmidt Sweden 292 127 6 21,17 165 6 27,50 3 2 4 Karel Molnar II Czech Republic 293 126 6 21,00 167 6 27,83 4 7 3 Pekka Itälä Finnland 294 128 6 21,33 166 6 27,67 5 3 6 Marcus Johansson Sweden 297 127 6 21,17 170 6 28,33 6 12 6 Peter Samuelsson Sweden 300 130 6 21,67 170 6 28,33 7 26 5 Gustav Björnberg Sweden 302 134 6 22,33 168 6 28,00 8 12 10 Philippe Charriere Switzerland 302 130 6 21,67 172 6 28,67 9 9 11 Michal Švehla Czech Republic 303 129 6 21,50 174 6 29,00 10 7 16 Lars Brown Sweden 305 128 6 21,33 177 6 29,50 11 21 9 Daniel Klosek Germany 254 111 5 22,20 143 5 28,60 12 18 11 Dominik Müller Germany 255 110 5 22,00 145 5 29,00 13 10 14 Csaba Palinkas Hungary 255 108 5 21,60 147 5 29,40 14 14 14 Thomas Emich Austria 256 109 5 21,80 147 5 29,40 15 5 17 Lutz Ermel Germany 256 106 5 21,20 150 5 30,00 16 1 26 Matias Peltola Finnland 257 101 5 20,20 156 5 31,20 17 47 8 Andreas Fransson Sweden 260 118 5 23,60 142 5 28,40 18 31 13 Florian Feichtner Austria 261 115 5 23,00 146 5 29,20 19 21 21 Simo Tuomi Finnland 263 111 5 22,20 152 5 30,40 20 31 17 Jan Aschenbrenner Germany 265 115 5 23,00 150 5 30,00 21 21 22 Marian Strasko Czech Republic 265 111 5 22,20 154 5 30,80 22 31 19 Kris Stille Germany 266 115 5 23,00 151 5 30,20 23 5 33 Reto Sommer Switzerland -

Housing in Vienna Annual Report 2016 Housing in Vienna Annual Report 2016 Housing in Vienna
Housing in Vienna Annual Report 2016 Annual Report 2016 Housing in Vienna Housing in Vienna Housing in Vienna Annual Report 2016 Online at www.wohnbauforschung.at Housing in Vienna Annual Report 2016 Contents STUDIOVLAY Foreword Management and Care Dedicated with Heart and Passion Page 7 At Home in a Municipal Housing Page 28 Wohnservice Wien - Bundling Service Skills Page 30 Introduction Mieterhilfe - The Experts in Rental Law Page 32 Social Housing Shapes the Future Page 10 wohnpartner: Working Together for a Good Neighborhood Page 34 Funding Social Housing Advice on Funding Page 36 Subsidized Housing Projects Page 16 Decorative Figures on the Town Hall Page 37 Page 20 Biotope City in Favoriten Research & Innovation An Additional Tool for Affordable Housing Page 21 IBA_Vienna 2022 - New Social Housing Page 40 Involving the Neighborhood Page 22 Smarter Together Page 42 Modern Living with Historic Flair Page 24 Well-Founded Know-How Page 44 Trailblazer Page 45 Notes Page 48 4 Housing in Vienna Annual Report 2016 Housing in Vienna Annual Report 2016 5 Foreword Sonnwendviertel, plot C.01 Architecture: Univ.-Prof. Arch. DI Klaus Kada / Riepl Riepl Architects / DI Bernd Vlay and Mag.a arch. Karoline Streeruwitz Spatial planning: rajek barosch landschaftsarchitektur Developer: win4wien Dedicated with Heart and Passion The City of Vienna is known for its special focus on social dimension in urban housing far beyond mere economic criteria. Thanks to decades of political emphasis on afforda- ble housing, Vienna is currently in a much better position than other metropolitan cities, where social housing has been either neglected or even completely abandoned. -

Nurse Aide Employment Roster Report Run Date: 9/24/2021
Nurse Aide Employment Roster Report Run Date: 9/24/2021 EMPLOYER NAME and ADDRESS REGISTRATION EMPLOYMENT EMPLOYMENT EMPLOYEE NAME NUMBER START DATE TERMINATION DATE Gold Crest Retirement Center (Nursing Support) Name of Contact Person: ________________________ Phone #: ________________________ 200 Levi Lane Email address: ________________________ Adams NE 68301 Bailey, Courtney Ann 147577 5/27/2021 Barnard-Dorn, Stacey Danelle 8268 12/28/2016 Beebe, Camryn 144138 7/31/2020 Bloomer, Candace Rae 120283 10/23/2020 Carel, Case 144955 6/3/2020 Cramer, Melanie G 4069 6/4/1991 Cruz, Erika Isidra 131489 12/17/2019 Dorn, Amber 149792 7/4/2021 Ehmen, Michele R 55862 6/26/2002 Geiger, Teresa Nanette 58346 1/27/2020 Gonzalez, Maria M 51192 8/18/2011 Harris, Jeanette A 8199 12/9/1992 Hixson, Deborah Ruth 5152 9/21/2021 Jantzen, Janie M 1944 2/23/1990 Knipe, Michael William 127395 5/27/2021 Krauter, Cortney Jean 119526 1/27/2020 Little, Colette R 1010 5/7/1984 Maguire, Erin Renee 45579 7/5/2012 McCubbin, Annah K 101369 10/17/2013 McCubbin, Annah K 3087 10/17/2013 McDonald, Haleigh Dawnn 142565 9/16/2020 Neemann, Hayley Marie 146244 1/17/2021 Otto, Kailey 144211 8/27/2020 Otto, Kathryn T 1941 11/27/1984 Parrott, Chelsie Lea 147496 9/10/2021 Pressler, Lindsey Marie 138089 9/9/2020 Ray, Jessica 103387 1/26/2021 Rodriquez, Jordan Marie 131492 1/17/2020 Ruyle, Grace Taylor 144046 7/27/2020 Shera, Hannah 144421 8/13/2021 Shirley, Stacy Marie 51890 5/30/2012 Smith, Belinda Sue 44886 5/27/2021 Valles, Ruby 146245 6/9/2021 Waters, Susan Kathy Alice 91274 8/15/2019 -

Namensverzeichnis Von Straßen, Plätzen Und Anlagen in Darmstadt Mit Erläuterungen Zur Benennung
Namensverzeichnis von Straßen, Plätzen und Anlagen in Darmstadt mit Erläuterungen zur Benennung Suchen: <STRG> <F> Name Erläuterung Lage im Zeitpunkt der Stadtgebiet Benennung Achatweg Benannt nach dem Edelstein Innenstadt 27. Februar 2002 Adelungstraße Bernhard Adelung (1876-1943), gelernter Schriftsetzer, 1923-1933 Hessi- Innenstadt Benennung 1945 scher Staatspräsident Adenauerplatz Dr. Konrad Adenauer (1876-1967), Deutscher Bundeskanzler von 1949- Stadtteil Eberstadt 10. Januar 1973 1963 Adolf-Spieß-Straße Adolf Spieß, geb. 1810 (Lauterbach), gest. 1858 (Darmstadt)), "hessi- Innenstadt *) scher Turnvater", Begründer des Schulturns, geboren in Lauterbach, Stu- dium der Theologie. International namhafter Förderer der Leibesübungen, wurde 1848 beauftragt, den Turnunterricht an allen hessischen Schulen einzuführen Ahastraße Benannt nach dem früher gegenüber vorhandenen Durchblick (Aha!) in Innenstadt *) der Umfriedung des Prinz-Emils-Gartens Akazienweg Baumart Innenstadt 21. August 1959 Alarich-Weiss-Straße Alarich Weiss (1925-1995), Professor für Physikalische Chemie an der Innenstadt 19. Juni 2013 Technischen Hochschule Darmstadt (heute: Technische Universität), Pio- nier der magnetischen Resonanz Albert-Schweitzer-Anlage Dr. Albert Schweitzer (1875-1965), Arzt und Forscher Innenstadt 3. April 1968 Albinmüllerweg Albin Müller (1871-1941), Architekt, entwarf u. a. das Löwentor am Ein- Innenstadt 24. Juni 1987 gang zur Rosenhöhe Albrechtstraße Benennung erfolgte aus einer Vorschlagsliste der Arheilger Bezirksverwal- Stadtteil Arheilgen