Human Resources for Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
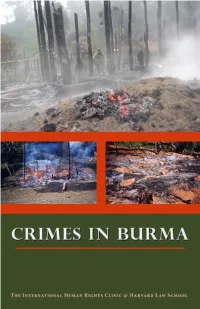
Crimes in Burma
Crimes in Burma A Report By Table of Contents Preface iii Executive Summary 1 Methodology 5 I. History of Burma 7 A. Early History and Independence in 1948 7 B. Military Rule: 1962-1988 9 C. The 1988 Popular Uprising and Democratic Elections in 1990 11 D. Military Rule Since 1988 12 II. International Criminal Law Framework 21 A. Crimes Against Humanity: Chapeau or Common Elements 24 B. War Crimes: Chapeau or Common Elements 27 C. Enumerated or Prohibited Acts 30 III. Human Rights Violations in Burma 37 A. Forced Displacement 39 B. Sexual Violence 51 C. Extrajudicial Killings and Torture 64 D. Legal Evaluation 74 ii Preface IV. Precedents for Action 77 A. The Security Council’s Chapter VII Powers 78 B. The Former Yugoslavia 80 C. Rwanda 82 D. Darfur 84 E. Burma 86 Conclusion 91 Appendix 93 Acknowledgments 103 Preface For many years, the world has watched with horror as the human rights nightmare in Burma has unfolded under military rule. The struggle for democracy of Nobel Peace Prize Laureate Daw Aung San Suu Kyi and other political prisoners since 1988 has captured the imagination of people around the world. The strength of Buddhist monks and their Saffron Revolution in 2007 brought Burma to the international community’s attention yet again. But a lesser known story—one just as appalling in terms of human rights—has been occurring in Burma over the past decade and a half: epidemic levels of forced labor in the 1990s, the recruitment of tens of thousands of child soldiers, widespread sexual violence, extrajudicial killings and torture, and more than a million displaced persons. -

3 Sides to Every Story
33 SSIDES TO EEVERY SSTORY A PROFILE OF MUSLIM COMMUNITIES IN THE REFUGEE CAMPS ON THE THAILAND BURMA BORDER THAILAND BURMA BORDER CONSORTIUM JULY 2010 Note on the Title: The “three sides” refers to the three self-identified sectors of Muslim communities in the camps, defined by the reasons for their presence in the camps (see “Muslim Lifestyle Practices and Preferences/ Socio-Cultural/ Self-identity”). Cover design: http://library.wustl.edu/subjects/islamic/MihrabIsfahan.jpg 2 33 SSIDES TO EEVERY SSTORY A PROFILE OF MUSLIM COMMUNITIES IN THE REFUGEE CAMPS ON THE THAILAND BURMA BORDER THAILAND BURMA BORDER CONSORTIUM JULY 2010 3 CONTENTS PAGE EXECUTIVE SUMMARY ……….......………………………………………………….……………………………. 7 SUMMARY OF STATISTICS BY RELIGION/CAMP ……………………………………………………………....... 9 PREFACE ……….......………………………………………………….……………………………………… 13 BACKGROUND INTRODUCTION OF ISLAM TO BURMA ………………………………………………………………………...... 15 DISPLACEMENT OF BURMESE MUSLIM COMMUNITIES INTO THAILAND ……..……………………………………… 15 Border-wide Camp-Specific Other Influxes CURRENT SITUATION PREVALENCE OF MUSLIM COMMUNITIES IN AND AROUND THE REFUGEE CAMPS ……..……………………. 19 Muslim Communities in Camps Muslim Communities Around the Camps Impacts on Camp Security LIFESTYLE PRACTICES AND PREFERENCES: SOCIO-CULTURAL: ……………………………………………………………………………………………… 21 o The “Three Sides” o Religion and Faith o Gender Roles o Romance, Marriage and Divorce o Social Inclusion FOOD AND SHELTER: ………….…...………………..…………………………….…………………….. 29 o Ration Collection/ Consumption o Ration/ Diet Supplementation -

The Situation in Karen State After the Elections PAPER No
EBO ANALYSIS The Situation in Karen State after the Elections PAPER No. 1 2011 THE SITUATION IN KAREN STATE AFTER THE ELECTIONS EBO Analysis Paper No. 1/2011 For over sixty years the Karens have been fighting the longest civil war in recent history. The struggle, which has seen demands for an autonomous state changed to equal recognition within a federal union, has been bloody and characterized by a number of splits within the movement. While all splinter groups ostensibly split to further ethnic Karen aspirations; recent decisions by some to join the Burmese government’s Border Guard Force (BGF) is seen as an end to such aspirations. Although a number of Karen political parties were formed to contest the November elections, the likelihood of such parties seriously securing appropriate ethnic representation without regime capitulation is doubtful. While some have argued, perhaps correctly, that the only legitimate option was to contest the elections, the closeness of some Karen representatives to the current regime can only prolong the status quo. This papers examines the problems currently affecting Karen State after the 7 November elections. THE BORDER GUARD FORCE Despite original promises of being allowed to recruit a total of 9,000 troops, the actual number of the DKBA (Democratic Karen Buddhist Army) or Karen Border Guard Force has been reduced considerably. In fact, a number of the original offers made to the DKBA have been revoked. At a 7 May 2010 meeting held at Myaing Gyi Ngu, DKBA Chairman U Tha Htoo Kyaw stated that ‘According to the SE Commander, the BGF will retain the DKBA badge.’ In fact the DKBA were given uniforms with SPDC military patches and all Karen flags in DKBA areas were removed and replaced by the national flag. -

Rivalry and Cooperation: Military Rule on the Thai- Burmese Border
International Journal of Management and Applied Science, ISSN: 2394-7926 Volume-4, Issue-2, Feb.-2018 http://iraj.in RIVALRY AND COOPERATION: MILITARY RULE ON THE THAI- BURMESE BORDER SIRINYA SIRIYANUN Suan Sunandha Rajabhat University, College of Innovation and Management, Department of Political Science Thailand E-mail: [email protected] Abstract- For much of the past fifty years, the border region surrounding the Thai and Burmese towns of Mae Sot and Myawaddy has been ruled by the military. The two countries which share this border, Thailand and Burma, have a long history of military rule. In addition, the indigenous people of the region, the Karen, have been conducting a decades-long insurrection against the Burmese government. Since the 1960s, all of the Karen military groups have been headquartered in this region. Ethnic politics in the Mae Sot-Myawaddy border region is therefore the politics of the military. Within this framework, both rivalry and cooperation are apparent. The balance of power between different Karen armed groups has shifted, and each group has made alliances and fought armed conflicts with both the state armies of Thailand and Burma and with other Karen armed groups. Since the 1990s, the trend has shifted towards greater cooperation, as the rise of Southeast Asia as a major economic region has motivated the armed groups of the Thai-Burmese border to work together to improve the region’s economy. Keywords- Thailand, Burma, borders, military rule, politics, cooperation I. MILITARY RULE IN MAE SOT AND In addition to the BPP, the Thai army also has a MYAWADDY significant presence. -

Karen Refugees from Burma in the US: an Overview for Torture Treatment Programs Presentation by Eh Taw Dwe and Tonya Cook Caveat “Karen People Are Very Diverse
Karen Refugees from Burma in the US: an Overview for Torture Treatment Programs Presentation by Eh Taw Dwe and Tonya Cook Caveat “Karen people are very diverse. Among the Karen people there are different languages, different cultures, different religions, and different political groups. No one can claim to speak on behalf of all Karen people, or represent all Karen people.” - Venerable Ashin Moonieinda From “The Karen people: Culture, Faith and History.” (http://www.karen.org.au/docs/karen_people.pdf) Introduction to Burma - January 4th, 1948 –independence - Government type = Military Junta. A brutal military regime has been in power since 1962. - The junta allowed “elections” to be held in Burma in 1990. - The National League for Democracy (NLD) led by Aung San Suu Kyi won over 80% of the vote. The list of party candidates became the hit list of the junta. The NLD was never allowed to claim their rightful seats. Burma or Myanmar? •The military dictatorship changed the name of Burma to Myanmar in 1989. • Parties who do not accept the authority of the unelected military regime to change the official name of the country still call it Burma (minority ethnic groups, the U.S. and the UK. •The UN, France, and Japan recognize it as Myanmar. http://news.bbc.co.uk/2/hi/7013943.stm Who Lives in Burma? There are eight main ethnic groups and 130 distinct sub-groups Total Population = ~55 Million Includes: •Burmans = 37.4 Million (68%) •Karen in Burma = 7 to 9 Million •Karen in Thailand = 400,000 •Karen in Thai refugee camps= ~150,000 Source: http://www.cal.org/co/pdffiles/refugeesfromburma.pdf Map courtesy of Free Burma Rangers Kachin Karenni Chin Mon Rakhine (Arakanese) Shan Burman Karen Map of the Karen State How to Refer to Refugees from Burma There is no single national identity. -

English 2005
Thailand Burma Border Consortium October 2005 Internal Displacement and Protection in Eastern Burma With Field Research and Situation Updates by: Committee for Internally Displaced Karen People Karen Office of Relief and Development Karenni Social Welfare and Development Centre Mon Relief and Development Committee Shan Relief and Development Committee Thailand Burma Border Consortium 12/5 Convent Road, Bangkok, 10500, Thailand [email protected] Artwork by Friends Without Borders www.tbbc.org (under construction) Printed by Wanida Press Front cover photos: New Arrivals in Mon Ceasefire Area, Ye township, January 2005. Peace Rally against Civil War, Kawkareik township, October 2004, CIDKP. CONTENTS Page List of Maps and Charts .................................................................................. i Acronyms ........................................................................................................ ii EXECUTIVE SUMMARY ................................................................................. 1 1. INTRODUCTION ........................................................................................ 5 1.1 Protracted Conflict in Burma ............................................................... 6 1.2 Internally Displaced Persons ............................................................... 7 1.3Humanitarian Protection ...................................................................... 9 1.4 Survey Rationale ................................................................................. 10 1.5 Survey -

IMPERCEPTIBLE NAKED-LIVES & ATROCITIES: Forcffily DISPLACED PEOPLES & the THAI-BURMESE IN-BETWEEN SPACES a DISSERTATION
IMPERCEPTIBLE NAKED-LIVES & ATROCITIES: FORCffiLY DISPLACED PEOPLES & THE THAI-BURMESE IN-BETWEEN SPACES A DISSERTATION SUBMITTED TO THE GRADUATE DIVISION OF THE UNIVERSITY OF HAWAI'I IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN POLITICAL SCIENCE MAY 2003 By Decha Tangseefa Dissertation Committee: Michael J. Shapiro, Chairperson Manfred Henningsen Sankara Krishna Nevzat Soguk Leslie E. Sponsel Acknowledgements When I was in the Burman-Karen war zones, in a gathering of forcibly displaced Karen, one of them asked me what made me decide to pursue this research. I responded to him that it had to do with one story and one incident. The story began with my illiterate mother's life-journey. When she was twelve, she migrated to Thailand with her "owner" boss after being sold to that family three years earlier by her fisher parents living in a seashore village of San Thou, in southeast China. Growing up listening to her stories of suffering, I had invariably felt anguished. But when I started to learn more about the forcibly displaced peoples along the Thai-Burmese border zones, I began to wonder why, as a Thai citizen, I knew almost nothing about them, and also why Thai society had rarely been concerned with the plight of at least one hundred thousand peoples living in a string of "camps" along the border zones and more than one million "illegal" laborers roaming in the country. The more I learnt about the tormenting stories of the forcibly displaced from Burma, the more my mother's stories paled. -

Maximizing Transport Benefits Through Community Engagement Project
Technical Assistance Consultant’s Report Project Number: 46422-002 December 2015 Republic of the Union of Myanmar: Maximizing Transport Benefits through Community Engagement (Financed by the Technical Assistance Special Fund) Prepared by the Mekong Economics, Ltd. and the Adventist Development Relief Agency Myanmar For the Ministry of Construction and the Asian Development Bank This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. Kayin and Mon State Context, Stakeholders and Engagement Kayin and Mon States Context, Stakeholders and Engagement Guidance for the Asian Development Bank (ADB) and implementing partners December 2015 Mekong Economics / ADRA Myanmar 1 Kayin and Mon State Context, Stakeholders and Engagement Table of Contents Acronyms ....................................................................................... 3 Introduction .................................................................................... 6 Terminology ......................................................................................... 8 A note on place names and administrative demarcation .................................... 8 Ethnographic overview ............................................................................ 9 Overview of Conflict and peace in Kayin and Mon States ........................... 10 The Peace Process since 2011 .................................................................. 12 Humanitarian impacts: -

NEITHER WAR NOR PEACE the FUTURE of the CEASE-FIRE AGREEMENTS in BURMA Main Armed Groups in Nothern Burma
TRANSNATIONAL I N S T I T U T E NEITHER WAR NOR PEACE THE FUTURE OF THE CEASE-FIRE AGREEMENTS IN BURMA Main armed groups in nothern Burma. Areas are approximate, status of some groups changed groups some of status approximate, are Areas Burma. in nothern groups armed Main Author Printing Contact: Tom Kramer Drukkerij PrimaveraQuint Transnational Institute Amsterdam De Wittenstraat 25 Copy editor 1052 AK Amsterdam David Aronson Financial Contributions Netherlands Ministry of Foreign Affairs Tel: 31-20-6626608 Design (Netherlands) Fax: 31-20-6757176 Guido Jelsma [email protected] www.tni.org Photo credits Tom Kramer The contents of this document can be quoted or reproduced as long as the source is mentioned. TNI would appreciate receiving a copy of the text in which this document is used or cited. To receive information about TNI’s publications and activities, we suggest that you subscribe to our bi-weekly bulletin by sending a request to: [email protected] or registering at www.tni.org Amsterdam, July 2009 Contents Introduction 2 Burma: Ethnic Conflict and Military Rule 4 The Cease-fire Economy 24 Conflict Actors 4 Infrastructure 24 Independence and Civil War 5 Trade and Investment 25 Military Rule 6 Mono-Plantations 25 Cold War Alliances 7 Investment from Abroad 25 The Democracy Movement 7 Logging 26 Mining 27 The Making of the Cease-fire Agreements 8 Drugs Trade 27 The Fall of the CPB 8 The First Round of Crease-fires 9 International Responses to the Cease-fires 30 The NDF and the Second Round of Cease-fires 9 The Role of Neighbouring Countries -

Ceasefires, Governance and Development: the Karen National
Ceasefires, Governance, and Development: The Karen National Union in Times of Change Kim Jolliffe December 2016 Acknowledgements The author would like to thank the many individuals in the Karen National Union, Karen community based organizations, and other Karen armed organizations who contributed their time, knowledge and encouragement to make this study possible. In particular, this work was inspired by the impressive and diverse Karen social service and humanitarian networks that work tirelessly every day to support communities affected by war. Significant parts of this research would not have been possible without support from the Karen Environmental Social Action Network, which works for rural livelihoods and environmental security of indigenous Karen people. This study benefited greatly from the more than two decade’s worth of testimony from rural Karen civilians collected by the Karen Human Rights Group, which remains a crucial and extraordinary resource to any research on these conflicts. This work was improved immeasurably by input from Brian McCartan, Tim Schroeder, Ashley South, Paul Keenan, and Jared Bissinger, which included feedback on drafts and various published and unpublished materials. Encouragement and dialogue with multiple other Myanmar and international researchers and professionals were also highly valuable. This series of papers has been built on the firm foundations of the broader research program initiated and developed by The Asia Foundation’s Matthew Arnold, among other key individuals. It has been made possible by the tireless production, administrative and editorial work of Mim Koletschka, Win Po Po Aung and the rest of their team. About the Author Kim Jolliffe is an independent researcher, writer, analyst and trainer, specializing in security, aid policy, and ethnic politics in Myanmar/Burma. -

Political Context of the Dams in Karen State
DAMMING AT GUNPOINT BURMA ARMY ATROCITIES PAVE THE WAY FOR SALWEEN DAMS IN KAREN STATE KAREN RIVERS WATCH NOVEMBER 2004 KAWTHOOLEI Karen Rivers Watch is a coalition of Karen organisations – the Karen Office of Relief and Development (KORD), Karen Youth Organisation (KYO), Karen Student Network Group (KSNG), Karen Environmental and Social Action Network (KESAN), Karen Women’s Organisation (KWO) and Federal Trade Union of Kawthoolei (FTUK) - which work on environmental, women’s, youth, human rights and development issues within the Karen community in Karen State. It was formed to monitor development processes affecting the environment, especially rivers, in Karen State in particular and Burma in general, and to mobilize grassroots communities, as well advocate, with other Burma compatriots, for democratic and sustainable development in Burma. Typeset and book design by the Students’ Friend Magazine, KSNG Graphic - Saw Eh Nah (Lynn Kyaw) Rich men dam the water Flooding the hill rice field, causing problems for Mother Rich men dam the river Flooding over the roof and making Mother homeless. Traditional Karen saying Acronyms and terms in the book Terms and acronyms related to SPDC SPDC State Peace and Development Council (Military Junta) IB Infantry Battalion LIB Light Infantry Battalion South Eastern Regional Command - The military command in Karen State and Mon State Terms and acronyms related to KNU KNU Karen National Union KNLA Karen National Liberation Army (KNU’s army) KNDO Karen National Defense Organisation (KNU’s militia) KNU administration zones in Karen State and Tenasserim Division (Civil adminstration and corresponding military command) 1. Thaton District - Brigade 1 2. Taungoo District - Brigade 2 3. -

This Study Is Concerned with a Town and Its Vicinities in the Thailand
INTEGRATING OTHERS: A STUDY OF A BORDER SOCIAL SYSTEM IN THE THAILAND-BURMA BORDERLAND LEE SANG KOOK NATIONAL UNIVERSITY OF SINGAPORE 2007 INTEGRATING OTHERS: A STUDY OF A BORDER SOCIAL SYSTEM IN THE THAILAND-BURMA BORDERLAND LEE SANG KOOK (M.A., Seoul National University/Korea) A THESIS SUBMITTED FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF SOCIOLOGY NATIONAL UNIVERSITY OF SINGAPORE 2007 ACKNOWLEDGEMENTS I was in deep grief at the final stage of writing this thesis due to the sudden demise of my great teacher, Ananda Rajah. With the loss of my great mentor, I struggled to overcome the emptiness of my heart and to find new sources of the inspiration and sharpness he used to provide. The final stages of my writing were filled with regret that I lost him too early before I could appreciate him both as a friend and an intellectual peer. His absence made me realize what a great teacher he was to me and how well I was taken care of by him. I dedicate this thesis to him. Through this sorrowful period, many people stood behind me, shared my sadness and encouraged me to carry on my work. Above all, I am deeply grateful to Saroja Dorairajoo for taking over the supervisory role and wonderfully guiding my study in the remaining period. I am very thankful to Hing Ai Yun for her dedicated care throughout my years at NUS and particularly at the final stage. I also thank the other two members of my thesis committee. Carl Grundy-Warr shared my grief at losing his good friend and was a great help towards the completion of this thesis.