Protocol (C) H8H-MC-LAHU a Randomized, Double-Blind, Four
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
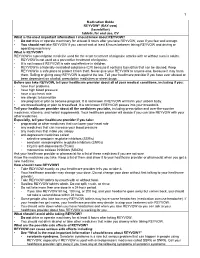
Medication Guide
1 Medication Guide REYVOW® (RAY-vow) (lasmiditan) tablets, for oral use, CV What is the most important information I should know about REYVOW? • Do not drive or operate machinery for at least 8 hours after you take REYVOW, even if you feel well enough. • You should not take REYVOW if you cannot wait at least 8 hours between taking REYVOW and driving or operating machinery. What is REYVOW? REYVOW is a prescription medicine used for the acute treatment of migraine attacks with or without aura in adults. • REYVOW is not used as a preventive treatment of migraine. • It is not known if REYVOW is safe and effective in children. • REYVOW is a federally controlled substance (CV) because it contains lasmiditan that can be abused. Keep REYVOW in a safe place to protect it from theft. Never give your REYVOW to anyone else, because it may harm them. Selling or giving away REYVOW is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. Before you take REYVOW, tell your healthcare provider about all of your medical conditions, including if you: • have liver problems • have high blood pressure • have a low heart rate • are allergic to lasmiditan • are pregnant or plan to become pregnant. It is not known if REYVOW will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if REYVOW passes into your breastmilk. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

Lasmiditan Is an Effective Acute Treatment for Migraine: a Phase 3 Randomized Study Bernice Kuca, Stephen D
ARTICLE OPEN ACCESS CLASS OF EVIDENCE Lasmiditan is an effective acute treatment for migraine A phase 3 randomized study Bernice Kuca, BA, MS, Stephen D. Silberstein, MD, Linda Wietecha, BSN, MS, Paul H. Berg, MS, Correspondence Gregory Dozier, MPH, and Richard B. Lipton, MD, on behalf of the COL MIG-301 Study Group Ms. Wietecha [email protected] Neurology® 2018;91:e2222-e2232. doi:10.1212/WNL.0000000000006641 Abstract RELATED ARTICLE Objective Article To assess the efficacy and safety of lasmiditan in the acute treatment of migraine. Galcanezumab in chronic migraine: The randomized, Methods double-blind, placebo- Adult patients with migraine were randomized (1:1:1) to a double-blind dose of oral lasmiditan controlled REGAIN study 200 mg, lasmiditan 100 mg, or placebo and were asked to treat their next migraine attack within Page 1082 4 hours of onset. Over 48 hours after dosing, patients used an electronic diary to record headache pain and the presence of nausea, phonophobia, and photophobia, one of which was MORE ONLINE designated their most bothersome symptom (MBS). Class of Evidence Criteria for rating Results ≥ therapeutic and diagnostic Of the 1,856 patients who treated an attack, 77.9% had 1 cardiovascular risk factors in addition studies to migraine. Compared with placebo, more patients dosed with lasmiditan 200 mg were free of NPub.org/coe headache pain at 2 hours after dosing (32.2% vs 15.3%; odds ratio [OR] 2.6, 95% confidence interval [CI] 2.0–3.6, p< 0.001), similar to those dosed with lasmiditan 100 mg (28.2%; OR 2.2, 95% CI 1.6–3.0, p< 0.001). -

Acute Migraine Treatment
Acute Migraine Treatment Morris Levin, MD Professor of Neurology Director, Headache Center UCSF Department of Neurology San Francisco, CA Mo Levin Disclosures Consulting Royalties Allergan Oxford University Press Supernus Anadem Press Amgen Castle Connolly Med. Publishing Lilly Wiley Blackwell Mo Levin Disclosures Off label uses of medication DHE Antiemetics Zolmitriptan Learning Objectives At the end of the program attendees will be able to 1. List all important options in the acute treatment of migraine 2. Discuss the evidence and guidelines supporting the major migraine acute treatment options 3. Describe potential adverse effects and medication- medication interactions in acute migraine pharmacological treatment Case 27 y/o woman has suffered ever since she can remember from “sick headaches” . Pain is frontal, increases over time and is generally accompanied by nausea and vomiting. She feels depressed. The headache lasts the rest of the day but after sleeping through the night she awakens asymptomatic 1. Diagnosis 2. Severe Headache relief Diagnosis: What do we need to beware of? • Misdiagnosis of primary headache • Secondary causes of headache Red Flags in HA New (recent onset or change in pattern) Effort or Positional Later onset than usual (middle age or later) Meningismus, Febrile AIDS, Cancer or other known Systemic illness - Neurological or psych symptoms or signs Basic principles of Acute Therapy of Headaches • Diagnose properly, including comorbid conditions • Stratify therapy rather than treat in steps • Treat early -

Acute Treatments for Migraine: Effectiveness and Value
Acute Treatments for Migraine: Effectiveness and Value Modeling Analysis Plan September 24, 2019 Institute for Clinical and Economic Review ©Institute for Clinical and Economic Review, 2019 Table of Contents 1. Approach ............................................................................................................................................ 3 2. Methods ............................................................................................................................................. 3 2.1 Overview and Model Structure .................................................................................................... 3 2.2 Key Model Choices and Assumptions .......................................................................................... 7 2.3 Populations .................................................................................................................................. 7 2.4 Interventions and Comparators ................................................................................................... 9 2.5 Input Parameters ......................................................................................................................... 9 2.6 Model Outcomes........................................................................................................................ 15 2.7 Model Analysis ........................................................................................................................... 16 References .......................................................................................................................................... -

Lasmiditan (Reyvow™) New Drug Update
Lasmiditan (Reyvow™) New Drug Update November 2019 Nonproprietary Name lasmiditan Brand Name Reyvow Manufacturer Eli Lilly and Company Form Tablets Strength 50 mg, 100 mg FDA Approval October 11, 2019 Market Availability Anticipated within 90 days of approval, following Drug Enforcement Agency (DEA) review FDA Approval Classification Standard Review FDB Classification- Specific TBD Therapeutic Class (HIC3) INDICATION1 Lasmiditan (Reyvow) is a serotonin 5-HT1F receptor agonist indicated for the acute treatment of migraine with or without aura in adults. Limitation of Use: Lasmiditan is not indicated for preventive treatment of migraine. PHARMACOKINETICS After oral administration of lasmiditan, the median time to maximum serum concentration (Tmax) is 1.8 hours. Food, age, gender, race, ethnicity, body weight, or renal function do not have a clinically significant effect on the pharmacokinetics of lasmiditan. The agent is 55% to 60% plasma protein bound. Lasmiditan is primarily metabolized via hepatic and extrahepatic metabolism, primarily by non- cytochrome P450 enzymes (e.g., ketone reduction) and has no pharmacologically active metabolites. Its mean terminal half-life is 5.7 hours. CONTRAINDICATIONS/WARNINGS Lasmiditan does not have any contraindications. Lasmiditan has been associated with significant impairment in the ability to drive or operate machinery following a single dose. Patients should be advised not take lasmiditan unless they are able to avoid driving or operating machinery for at least 8 hours after each lasmiditan dose. Prescribers should be aware that the patient’s ability to determine their own mental alertness may also be affected and should discuss this with the patient. Proprietary Information. Restricted Access – Do not disseminate or copy without approval. -

Headache Management: Pharmacological Approaches
REVIEW Headache management: Pract Neurol: first published as 10.1136/practneurol-2015-001167 on 3 July 2015. Downloaded from pharmacological approaches Alex J Sinclair,1,2 Aaron Sturrock,2 Brendan Davies,3 Manjit Matharu4 ▸ Additional material is ABSTRACT be very rewarding for the clinician. The published online only. To view Headache is one of the most common conditions purpose of this article, the first of two please visit the journal online (http://dx.doi.org/10.1136/ presenting to the neurology clinic, yet a linked articles, is to provide an up-to-date practneurol-2015-001167). significant proportion of these patients are overview of the pharmacological manage- unsatisfied by their clinic experience. Headache ment of common headache disorders 1Department of Neurobiology, School of Clinical and can be extremely disabling; effective treatment is (as well as a limited number of non- Experimental Medicine, College not only essential for patients but is rewarding pharmaceutical strategies). of Medical and Dental Sciences, for the physician. In this first of two parts review The University of Birmingham, of headache, we provide an overview of Birmingham, UK THE COMMON PRIMARY HEADACHE 2Neurology Department, headache management, emerging therapeutic DISORDERS University Hospitals Birmingham strategies and an accessible interpretation of In European populations, the annual sex- NHS Trust, Queen Elizabeth clinical guidelines to assist the busy neurologist. Hospital Birmingham, adjusted prevalence for tension-type Birmingham, UK headache is 35%, for migraine is 38%, 3 Department of Neurology, Royal BACKGROUND but for cluster headache is only Stoke University Hospital, ’ 0.15%.45These three together comprise Stoke-on-Trent, UK Headache is listed among the WHO s 4Headache Group, Institute of major causes of disability with a global the most prevalent primary headache dis- Neurology, London, UK prevalence of 47% (symptoms occurring orders. -

Lasmiditan (Reyvow)
Prior Authorization Review Panel Prior Authorization Review Panel CHC-MCO Policy Submission A separate copy of this form must accompany each policy submitted for review. Policies submitted without this form will not be considered for review. Plan: PA Health & Wellness Submission Date: 05/01/2020 Policy Number: PA.CP.PMN.218 Effective Date: 05/2020 Revision Date: 05/2020 Policy Name: Lasmiditan (Reyvow) Type of Submission – Check all that apply: New Policy Revised Policy* Annual Review - No Revisions Statewide PDL - Select this box when submitting policies for Statewide PDL implementation and when submitting policies for drug classes included on the Statewide PDL. *All revisions to the policy must be highlighted using track changes throughout the document. Please provide any changes or clarifying information for the policy below: New Policy Created Name of Authorized Individual (Please type or print): Signature of Authorized Individual: Francis G. Grillo, MD Page 1 of 5 CLINICAL POLICY Lasmiditan Clinical Policy: Lasmiditan (Reyvow) Reference Number: PA.CP.PMN.218 Effective Date: 05/2020 Last Review Date: 05/2020 Revision Log Description Lasmiditan (Reyvow™) is a serotonin (5-HT) 1F agonist. FDA Approved Indication(s) Reyvow is indicated for the acute treatment of migraine with or without aura in adults. Limitation(s) of use: Reyvow is not indicated for the preventive treatment of migraine. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with PA Health & Wellness that Reyvow is medically necessary when the following criteria are met: I. -

Lasmiditan (Reyvow) Reference Number: CP.PMN.218 Effective Date: 03.01.20 Last Review Date: 02.21 Line of Business: Commercial, HIM, Medicaid Revision Log
Clinical Policy: Lasmiditan (Reyvow) Reference Number: CP.PMN.218 Effective Date: 03.01.20 Last Review Date: 02.21 Line of Business: Commercial, HIM, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Lasmiditan (Reyvow™) is a serotonin (5-HT) 1F agonist. FDA Approved Indication(s) Reyvow is indicated for the acute treatment of migraine with or without aura in adults. Limitation(s) of use: Reyvow is not indicated for the preventive treatment of migraine. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Reyvow is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Migraines (must meet all): 1. Diagnosis of migraine headaches; 2. Age ≥ 18 years; 3. Failure of at least TWO formulary 5HT1B/1D-agonist migraine medications (e.g., sumatriptan, rizatriptan, zolmitriptan) at up to maximally indicated doses, unless clinically significant adverse effects are experienced or all are contraindicated; 4. For requests for quantities greater than two doses per month, member meets one of the following (a or b): a. Failure of TWO prophylactic migraine medications, unless clinically significant adverse effects are experienced or all are contraindicated (see Appendix B); b. Member is being treated by or in consultation with a neurologist or a headache specialist; 5. Dose does not exceed 200 mg (2 tablets) per day and 4 days per month. Approval duration: Medicaid/HIM – 12 months Commercial – Length of Benefit B. -

Laws 2021, LB236, § 4
LB236 LB236 2021 2021 LEGISLATIVE BILL 236 Approved by the Governor May 26, 2021 Introduced by Brewer, 43; Clements, 2; Erdman, 47; Slama, 1; Lindstrom, 18; Murman, 38; Halloran, 33; Hansen, B., 16; McDonnell, 5; Briese, 41; Lowe, 37; Groene, 42; Sanders, 45; Bostelman, 23; Albrecht, 17; Dorn, 30; Linehan, 39; Friesen, 34; Aguilar, 35; Gragert, 40; Kolterman, 24; Williams, 36; Brandt, 32. A BILL FOR AN ACT relating to law; to amend sections 28-1202 and 69-2436, Reissue Revised Statutes of Nebraska, and sections 28-401 and 28-405, Revised Statutes Cumulative Supplement, 2020; to redefine terms, change drug schedules, and adopt federal drug provisions under the Uniform Controlled Substances Act; to provide an exception to the offense of carrying a concealed weapon as prescribed; to define a term; to change provisions relating to renewal of a permit to carry a concealed handgun; to provide a duty for the Nebraska State Patrol; to eliminate an obsolete provision; to harmonize provisions; and to repeal the original sections. Be it enacted by the people of the State of Nebraska, Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2020, is amended to read: 28-401 As used in the Uniform Controlled Substances Act, unless the context otherwise requires: (1) Administer means to directly apply a controlled substance by injection, inhalation, ingestion, or any other means to the body of a patient or research subject; (2) Agent means an authorized person who acts on behalf of or at the direction of another person but does not include a common or contract carrier, public warehouse keeper, or employee of a carrier or warehouse keeper; (3) Administration means the Drug Enforcement Administration of the United States Department of Justice; (4) Controlled substance means a drug, biological, substance, or immediate precursor in Schedules I through V of section 28-405. -

How Do I Choose Acute Treatment Medication Options for Migraine Patients?
How Do I Choose Acute Treatment Medication Options for Migraine Patients? Laura Xanders, FNP-BC Maureen Moriarty, DNP, APRN, FAHS, FAANP Step 1: Conduct a history of present illness (HPI) What is their migraine frequency? • What is the frequency of the paent’s moderate to severe migraine aacks? • What associated symptoms do they experience with their migraine aacks? • Are their migraine aacks rapid or gradual in onset? What do they currently take? • Do they get complete relief? • How oSen do they take it? • Can they tolerate oral medicaon during a migraine aack? What have they tried in the past that has or has not worked? Step 2: Determine any comorbid condiIons or concurrent medicaons that may be a contraindicaon to an acute migraine medicaon. A patient with a history of stomach A patient with a history of Pregnancy/lactation status ulcer may not be a good candidate cardiovascular disease or could impact safe or approved for an oral NSAID uncontrolled hypertension use of a medication may not be a good candidate for a triptan Step 3: Review the available acute medicaon opIons. 1. NSAIDs • Faster onset: diclofenac powder, ketorolac IM, ketorolac NS • Slower onset: naproxen, ibuprofen, diclofenac, indomethacin 2. Triptans • Short half life: sumatriptan, rizatriptan, eletriptan, almotriptan, zolmitriptan • Long half life: naratriptan, frovatriptan • Non-PO: sumatriptan NS, zolmitriptan NS, sumatriptan SQ 3. Acute CGRP antagonists (gepants) • ubrogepant • rimegepant 4. Ditans • lasmiditan 5. An-emecs* • metoclopramide • prochlorperazine • promethazine • ondansetron * Metoclopramide, prochlorperazine and promethazine have addiIonal direct anI-migraine effect but may be sedang, and ondansetron has no direct anI-migraine effect but is not sedang. -

Safe Non-Opioid and Non-Barbiturate Containing Acute Medication Combinations in Headache: an Exhaustive
medRxiv preprint doi: https://doi.org/10.1101/2020.06.26.20140897; this version posted June 28, 2020. TheZhang copyright and holder Kaytser, for this preprint 1 (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Title Page Article Title: Safe Non-opioid and Non-barbiturate containing Acute Medication Combinations in Headache: An Exhaustive Approach Based on DrugBank Database Authors: Victor Kaytser, MD Pengfei Zhang, MD Author affiliations: From the Department of Neurology, Rutgers Robert Wood Johnson Medical School, New Brunswick, New Jersey, USA (Victor Kaytser, Pengfei Zhang) Conflict of Interest Statement: Pengfei Zhang: He has received honorarium from Alder Biopharmaceuticals, Board Vitals, Fieve Clinical Research. He collaborates with Headache Science Incorporated without receiving financial support. Ownership interest in Cymbeline LLC Victor Kaytser: No disclosures. Key Words: Polypharmacy, Drug interactions, Combinatorics in medicine, Big data, Data science, Pharmacology Financial Support: None Trial Registration: Not applicable. Abbreviations: API – Application Programming Interface, NSAIDs – Nonsteroidal Anti-inflammatory Drugs, FDA – Food and Drugs Administration, 5HT1F – Serotonin receptor 1 F, CGRP – calcitonin gene-related peptide, CYP – cytochromes P450. Acknowledgements: None NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2020.06.26.20140897; this version posted June 28, 2020. TheZhang copyright and holder Kaytser, for this preprint 2 (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.