Safe Non-Opioid and Non-Barbiturate Containing Acute Medication Combinations in Headache: an Exhaustive
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kava (Piper Methysticum) and Its Methysticin Constituents Protect Brain Tissue Against Ischemic Damage in Rodents
5 Refs: Arletti R et al, Stimulating property of Turnera diffusa and Pfaffia paniculata extracts on the sexual-behavior of male rats. Psychopharmacology 143(1), 15-19, 1999. Berger F, Handbuch der drogenkunde . Vol 2, Maudrich, Wien, 1950. Martinez M, Les plantas medicinales de Mexico . Cuarta Edicion Botas Mexico , p119, 1959. Tyler VE et al, Pharmacognosy , 9 th edition, Lea & Febiger, Philadelphia, 1988. KAVA ( Piper methysticum ) - A REVIEW The Kava plant (Piper methysticum) is a robust, well-branching and erect perennial shrub belonging to the pepper family (Piperaceae). The botanical origin remains unknown, although it is likely that early Polynesian explorers brought the plant with them from island to island. Numerous varieties of Kava exist, and today it is widely cultivated in several Pacific Island countries both for local use as well as the rapidly growing demand for pharmaceutical preparations. The dried rhizomes (roots) are normally used. The first description to the western world of the ceremonial use of an intoxicating beverage prepared from Kava was made by Captain James Cook following his Pacific voyage in 1768. The drink, prepared as an infusion in an elaborate manner after first chewing the root, is consumed on formal occasions or meetings of village elders and chiefs, as well as in reconciling with enemies and on a more social basis. It remains an important social custom in many Pacific Island countries today. Most of the islands of the Pacific possessed Kava prior to European contact, particularly those encompassed by Polynesia, Melanesia and Micronesia. After drinking the Kava beverage a pleasantly relaxed and sociable state develops, after which a deep and restful sleep occurs. -
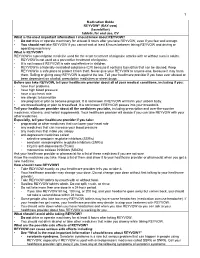
Medication Guide
1 Medication Guide REYVOW® (RAY-vow) (lasmiditan) tablets, for oral use, CV What is the most important information I should know about REYVOW? • Do not drive or operate machinery for at least 8 hours after you take REYVOW, even if you feel well enough. • You should not take REYVOW if you cannot wait at least 8 hours between taking REYVOW and driving or operating machinery. What is REYVOW? REYVOW is a prescription medicine used for the acute treatment of migraine attacks with or without aura in adults. • REYVOW is not used as a preventive treatment of migraine. • It is not known if REYVOW is safe and effective in children. • REYVOW is a federally controlled substance (CV) because it contains lasmiditan that can be abused. Keep REYVOW in a safe place to protect it from theft. Never give your REYVOW to anyone else, because it may harm them. Selling or giving away REYVOW is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. Before you take REYVOW, tell your healthcare provider about all of your medical conditions, including if you: • have liver problems • have high blood pressure • have a low heart rate • are allergic to lasmiditan • are pregnant or plan to become pregnant. It is not known if REYVOW will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if REYVOW passes into your breastmilk. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. -

Alternative Treatments for Depression and Anxiety
2019 PCB Conference: Strickland Benzodiazepines (BZDs), Herbal and Alternative Treatments for Anxiety & Depression BZD Learning Objectives • List at least three uses for benzodiazepines • Discuss at least two risk factors associated with benzodiazepine prescriptions Craig Strickland, PhD, Owner Biobehavioral Education and Consultation https://sites.google.com/site/bioedcon 1 2 BZD Pharmacokinetics Clinical Uses of BZDs Generic Name Trade Name Rapidity ½ Life Dose (mg) • Treat a variety of anxiety disorders alprazolam Xanax Intermediate Short 0.75-4 • Hypnotics • Muscle relaxants chlordiaze- Librium Intermediate Long 15-100 poxide • To produce anterograde amnesia clonazepam Klonopin Intermediate Long 0.5-4 • Alcohol & other CNS depressant withdrawal • Anti-convulsant therapy diazepam Valium Rapid Long 4-40 triazolam Halcion Intermediate Very short 0.125-0.5 temazepam Restoril Short Short 7.5-30 3 4 1 2019 PCB Conference: Strickland Issues with BZDs Herbal Medication and Alternative Therapies Used in the Treatment of Depression and Anxiety • Addictive potential • Confusion between “anti-anxiety” effects and the “warm-fuzzy) • Large dose ranges • Comparison of BZDs with medications like Buspar, etc. • They work, they work well and they work quickly 5 6 Alternative Tx. Learning Objectives Background Information on herbals: Natural does not necessarily mean “safe” • List several amino acid treatments for depression • Side-effects and adverse reactions • List at least three of the most common herbal – Herbal medications are “drugs” although -

Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin Healthcare
Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin healthcare 4/22/2020 Overview benzodiazepines • Examples of benzos and benzo like drugs • Indications for benzos • Pharmacology of benzos • Side effects and contraindications • Benzo withdrawal • Benzo tapers 12/06/2018 Sedative/Hypnotics • Benzodiazepines • Alcohol • Z-drugs (Benzo-like sleeping aids) • Barbiturates • GHB • Propofol • Some inhalants • Gabapentin? Pregabalin? 12/06/2018 Examples of benzodiazepines • Midazolam (Versed) • Triazolam (Halcion) • Alprazolam (Xanax) • Lorazepam (Ativan) • Temazepam (Restoril) • Oxazepam (Serax) • Clonazepam (Klonopin) • Diazepam (Valium) • Chlordiazepoxide (Librium) 4/22/2020 Sedatives: gaba stimulating drugs have incomplete “cross tolerance” 12/06/2018 Effects from sedative (Benzo) use • Euphoria/bliss • Suppresses seizures • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Sleep inducing • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 Tolerance to benzo effects? • Effects quickly diminish with repeated use (weeks) • Euphoria/bliss • Suppresses seizures • Effects incompletely diminish with repeated use • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Seep inducing • Durable effects with repeated use • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 If you understand this pharmacology you can figure out the rest... • Potency • 1 mg diazepam <<< 1 mg alprazolam • Duration of action • Half life differences • Onset of action • Euphoria, clinical utility in acute -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

Lasmiditan Is an Effective Acute Treatment for Migraine: a Phase 3 Randomized Study Bernice Kuca, Stephen D
ARTICLE OPEN ACCESS CLASS OF EVIDENCE Lasmiditan is an effective acute treatment for migraine A phase 3 randomized study Bernice Kuca, BA, MS, Stephen D. Silberstein, MD, Linda Wietecha, BSN, MS, Paul H. Berg, MS, Correspondence Gregory Dozier, MPH, and Richard B. Lipton, MD, on behalf of the COL MIG-301 Study Group Ms. Wietecha [email protected] Neurology® 2018;91:e2222-e2232. doi:10.1212/WNL.0000000000006641 Abstract RELATED ARTICLE Objective Article To assess the efficacy and safety of lasmiditan in the acute treatment of migraine. Galcanezumab in chronic migraine: The randomized, Methods double-blind, placebo- Adult patients with migraine were randomized (1:1:1) to a double-blind dose of oral lasmiditan controlled REGAIN study 200 mg, lasmiditan 100 mg, or placebo and were asked to treat their next migraine attack within Page 1082 4 hours of onset. Over 48 hours after dosing, patients used an electronic diary to record headache pain and the presence of nausea, phonophobia, and photophobia, one of which was MORE ONLINE designated their most bothersome symptom (MBS). Class of Evidence Criteria for rating Results ≥ therapeutic and diagnostic Of the 1,856 patients who treated an attack, 77.9% had 1 cardiovascular risk factors in addition studies to migraine. Compared with placebo, more patients dosed with lasmiditan 200 mg were free of NPub.org/coe headache pain at 2 hours after dosing (32.2% vs 15.3%; odds ratio [OR] 2.6, 95% confidence interval [CI] 2.0–3.6, p< 0.001), similar to those dosed with lasmiditan 100 mg (28.2%; OR 2.2, 95% CI 1.6–3.0, p< 0.001). -

Deliberate Self-Poisoning with a Lethal Dose of Pentobarbital: Survival with Supportive Care
Deliberate self-poisoning with a lethal dose of pentobarbital: Survival with supportive care. (1) (1,2) Santosh Gone , Andis Graudins (1) Clinical Toxicology Service, Program of Emergency Medicine, Monash Health (2) Monash Emergency Research Collaboration, Clinical Sciences at Monash Health, Monash University Abstract 84 INTRODUCTION CASE REPORT (continued) DISCUSSION Pentobarbital (Nembutal) is short acting In the ED: Pentobarbital has been a banned substance for barbiturate sedative-hypnotic, currently widely GCS: 3/15, fixed dilated pupils, apnoeic and human use in Australia since 1998. However, it can used in veterinary practice for anesthesia and ventilated. be procured overseas or bought on the internet. euthanasia. Pulse: 116 bpm sinus tachycardia BP: 115/60 on epinephrine infusion. Pentobarbital is recommended as an effective It is also commonly recommended as a VBG: pH 7.03 pCO2 77 mmHg Bicarb 19 mmol/L agent for use in euthanasia due to its apparently euthanasia drug for assisted suicide and it is Lactate 8.8 mmol/L peaceful transition to death. unlikely that any resuscitative measures will be Activated charcoal (50g) given via an NG tube. attempted in such cases. Course in the Intensive Care Department: In a case series of 150 assisted suicides in Day-1 post-OD: Sweden, a 100% success rate was seen with Intentional overdose results in depression of - Absent brain stem reflexes and fixed dilated pupils for ingestion of 9 grams. Cardiovascular collapse was brain stem function and rapid onset respiratory five days. seen within 15 minutes in 30% of patients. It is rare depression and apnoea. Hypotension also - Diabetes insipidus developed with urine output of to see survival after intentional ingestion for develops, followed by cardiovascular collapse 300ml/hour. -

Acute Migraine Treatment
Acute Migraine Treatment Morris Levin, MD Professor of Neurology Director, Headache Center UCSF Department of Neurology San Francisco, CA Mo Levin Disclosures Consulting Royalties Allergan Oxford University Press Supernus Anadem Press Amgen Castle Connolly Med. Publishing Lilly Wiley Blackwell Mo Levin Disclosures Off label uses of medication DHE Antiemetics Zolmitriptan Learning Objectives At the end of the program attendees will be able to 1. List all important options in the acute treatment of migraine 2. Discuss the evidence and guidelines supporting the major migraine acute treatment options 3. Describe potential adverse effects and medication- medication interactions in acute migraine pharmacological treatment Case 27 y/o woman has suffered ever since she can remember from “sick headaches” . Pain is frontal, increases over time and is generally accompanied by nausea and vomiting. She feels depressed. The headache lasts the rest of the day but after sleeping through the night she awakens asymptomatic 1. Diagnosis 2. Severe Headache relief Diagnosis: What do we need to beware of? • Misdiagnosis of primary headache • Secondary causes of headache Red Flags in HA New (recent onset or change in pattern) Effort or Positional Later onset than usual (middle age or later) Meningismus, Febrile AIDS, Cancer or other known Systemic illness - Neurological or psych symptoms or signs Basic principles of Acute Therapy of Headaches • Diagnose properly, including comorbid conditions • Stratify therapy rather than treat in steps • Treat early -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive -

Choice of Drugs in the Treatment of Rheumatoid Arthritis
RHEUMATOLOGY IN GENERAL PRACTICE 7 Those with predominant but never exclusive involvement of the terminal finger joint, usually associated with changes in the nail of the same finger; they are serologically negative. There may be a swollen finger with loss of the skin markings-a sort of dactylitis, again serologically negative. (2) Those with a much more severe process which produces loss of movement in the spine and changes in the sacroiliac joints much the same as those in ankylosing spondylitis; unlike ankylosing spondylitis, it produces severe deformity often with ankylosis in peripheral joints. Many of the finger joints become deformed and ankylosed. (3) Those cases indistinguishable from rheumatoid arthritis although the majority are sero-negative. The Stevens Johnson syndrome produces acute effusions, particularly in large joints. It is sometimes associated with the rash of erythema multiforme, always with ulceration in the mouth and genital tract; the mouth ulcers are accompanied by sloughing, unlike those of Beh9et's syndrome which we come to next. BehCet's syndrome, originally described as a combination of orogenital ulceration with relapsing iritis, is now expanded to include skin lesions, other eye lesions, lesions of the central nervous system, thrombophlebitis migrans, and arthropathy (occurring in 64 per cent). The onset is acute, often affecting only a single joint and settling without residual trouble. Choice of drugs in the treatment of rheumatoid arthritis Dr Dudley Hart, M.D., F.R.C.P. (Consultant physician, Westminster Hospital and Medical School) There are many potential drugs for the treatment of rheumatoid disease, but what are we treating in this disorder? Pain in rheumatoid arthritis is but one of the symp- toms. -

S1 Table. List of Medications Analyzed in Present Study Drug
S1 Table. List of medications analyzed in present study Drug class Drugs Propofol, ketamine, etomidate, Barbiturate (1) (thiopental) Benzodiazepines (28) (midazolam, lorazepam, clonazepam, diazepam, chlordiazepoxide, oxazepam, potassium Sedatives clorazepate, bromazepam, clobazam, alprazolam, pinazepam, (32 drugs) nordazepam, fludiazepam, ethyl loflazepate, etizolam, clotiazepam, tofisopam, flurazepam, flunitrazepam, estazolam, triazolam, lormetazepam, temazepam, brotizolam, quazepam, loprazolam, zopiclone, zolpidem) Fentanyl, alfentanil, sufentanil, remifentanil, morphine, Opioid analgesics hydromorphone, nicomorphine, oxycodone, tramadol, (10 drugs) pethidine Acetaminophen, Non-steroidal anti-inflammatory drugs (36) (celecoxib, polmacoxib, etoricoxib, nimesulide, aceclofenac, acemetacin, amfenac, cinnoxicam, dexibuprofen, diclofenac, emorfazone, Non-opioid analgesics etodolac, fenoprofen, flufenamic acid, flurbiprofen, ibuprofen, (44 drugs) ketoprofen, ketorolac, lornoxicam, loxoprofen, mefenamiate, meloxicam, nabumetone, naproxen, oxaprozin, piroxicam, pranoprofen, proglumetacin, sulindac, talniflumate, tenoxicam, tiaprofenic acid, zaltoprofen, morniflumate, pelubiprofen, indomethacin), Anticonvulsants (7) (gabapentin, pregabalin, lamotrigine, levetiracetam, carbamazepine, valproic acid, lacosamide) Vecuronium, rocuronium bromide, cisatracurium, atracurium, Neuromuscular hexafluronium, pipecuronium bromide, doxacurium chloride, blocking agents fazadinium bromide, mivacurium chloride, (12 drugs) pancuronium, gallamine, succinylcholine -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC).